Figures
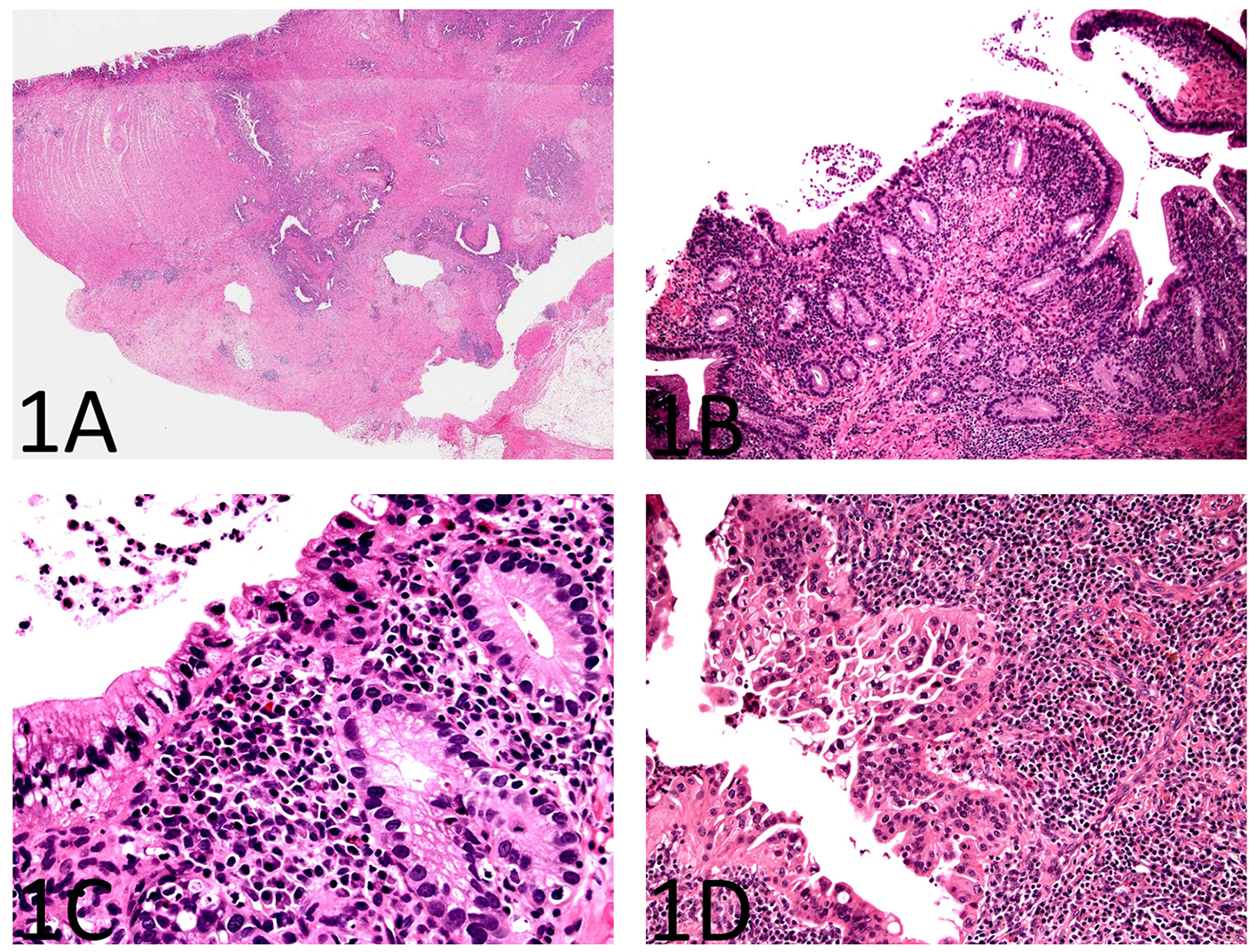
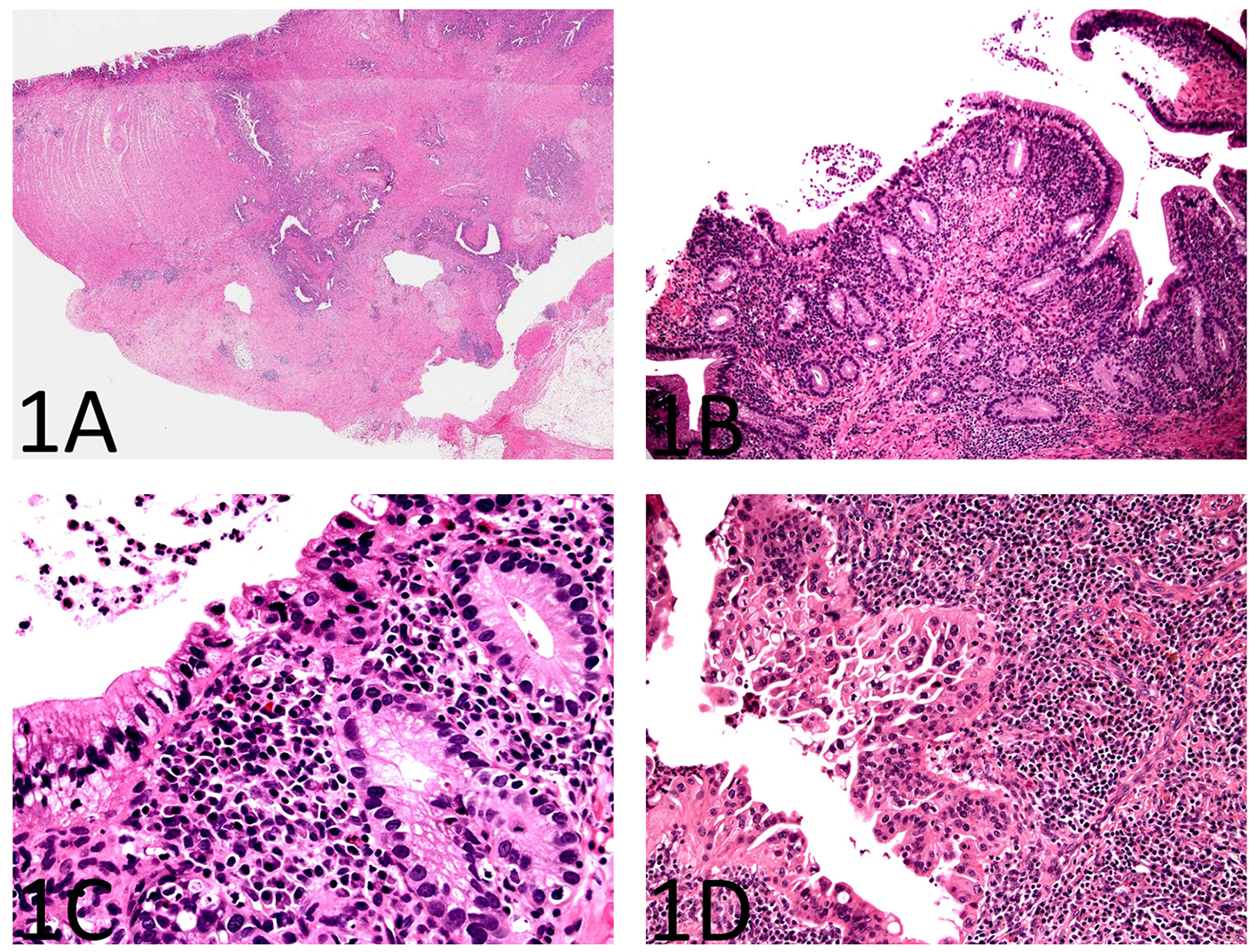
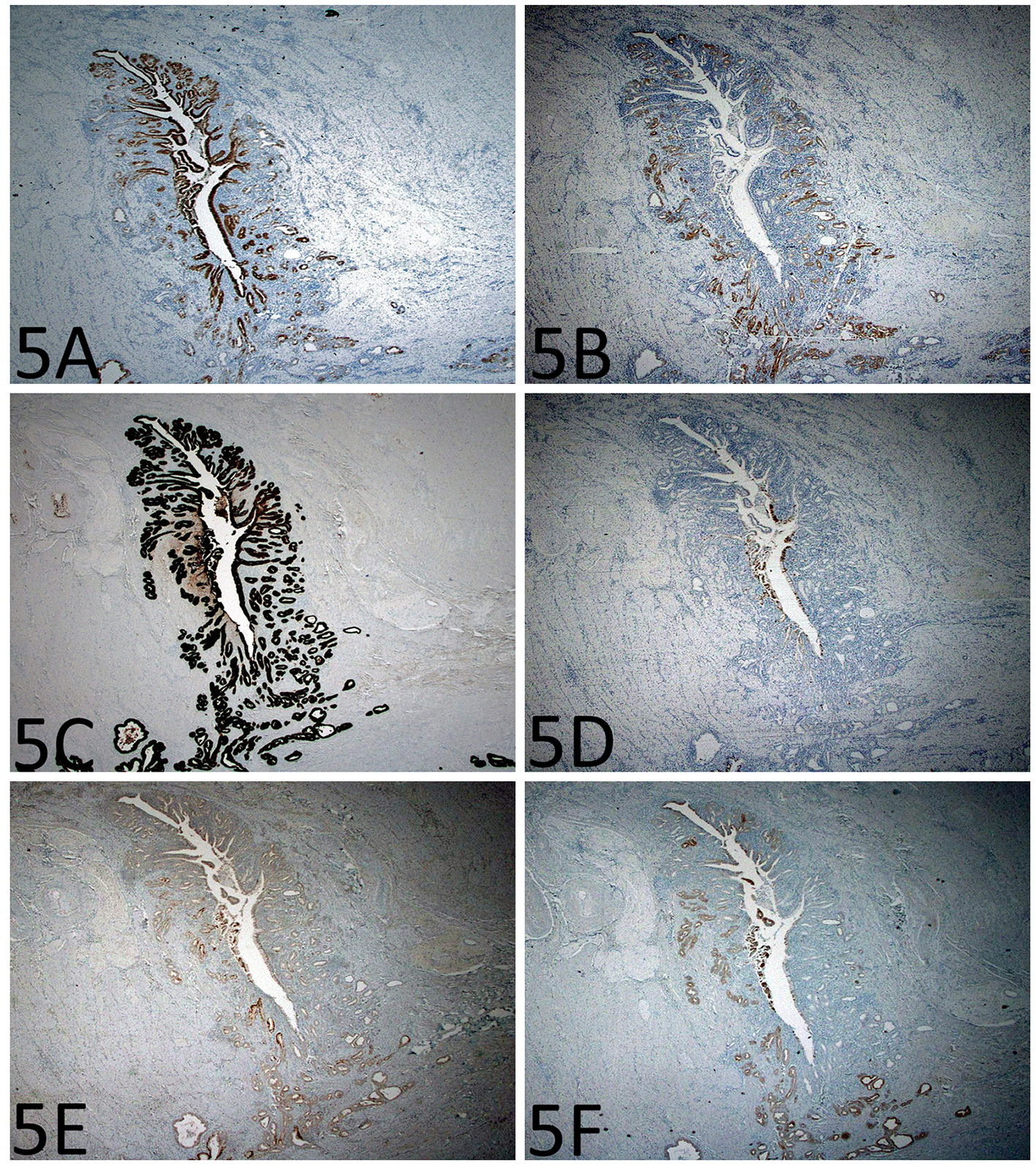
Figure 1. Histopathology of enteritis cystica profunda with high-grade dysplasia in the setting of Crohn’s disease of the small bowel. (A) A section from the stricture shows chronic active enteritis with extensive ulceration, submucosal and mural fibrosis, hypertrophy of muscular wall, transmural inflammation including prominent lymphoid aggregates, and neural hypertrophy (H&E, × 40). There are many, variably sized, cysts or diverticulum predominantly lined by small bowel type mucosa. Some of the cysts are seen in the deep portion of the muscularis propria and in the subserosa. (B) The small bowel mucosa lining the cysts is chronically and actively inflamed and the epithelium resembling pyloric glands composed of cuboidal cells (H&E, × 100). (C) The cyst-lining cuboidal cells are monotonous, have relatively high nucleus to cytoplasm (N/C) ratio, and do not show surface maturation, features of low-grade dysplasia (H&E, × 400). (D) Some of the cyst-lining cuboidal cells have thickened nuclear membranes and demonstrate nuclear pleomorphism and loss of nuclear polarity, features of high-grade dysplasia (H&E, × 400).
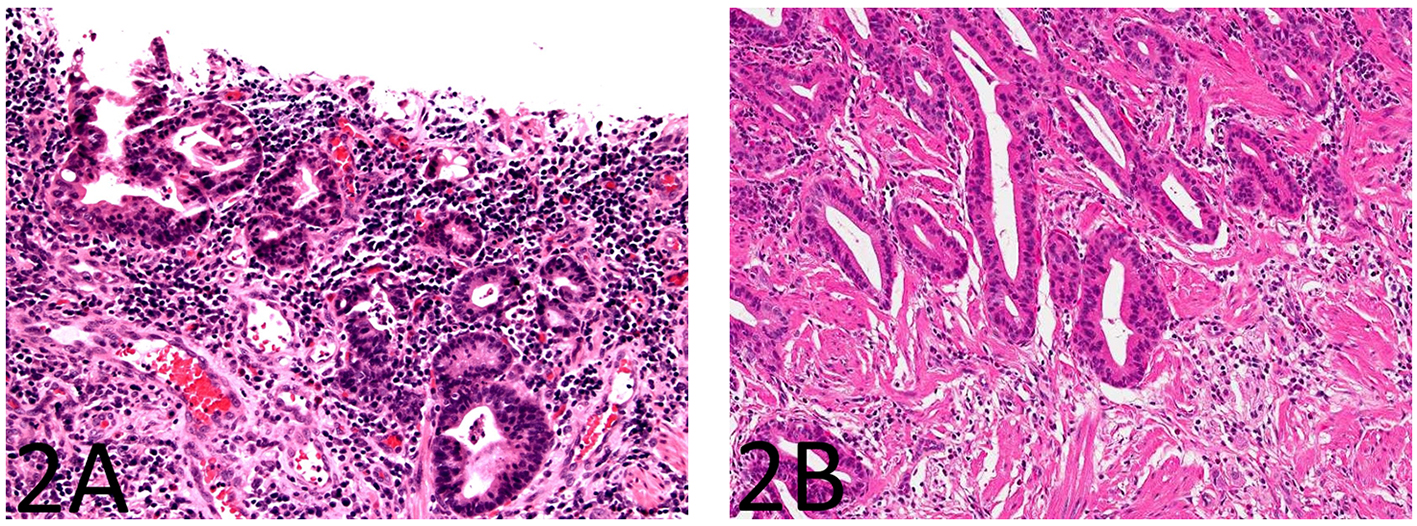
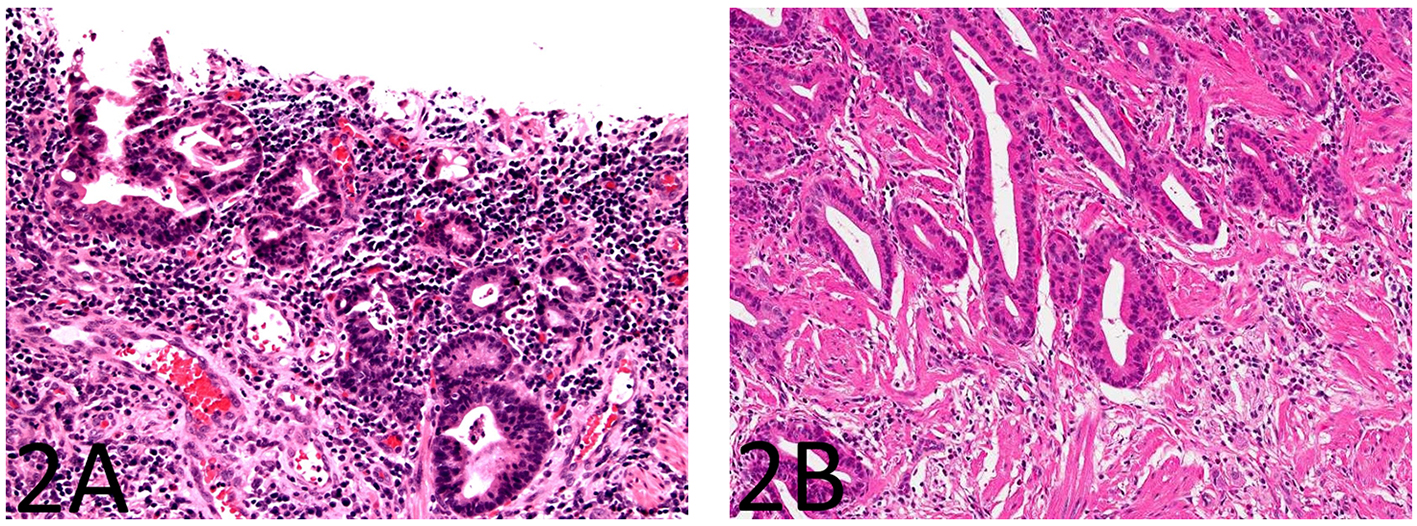
Figure 2. The small bowel mucosa overlying the strictured segment shows marked chronic active enteritis with high-grade dysplasia and intramucosal adenocarcinoma of gastric type (A: H&E stain, × 200; B: H&E stain, × 100).
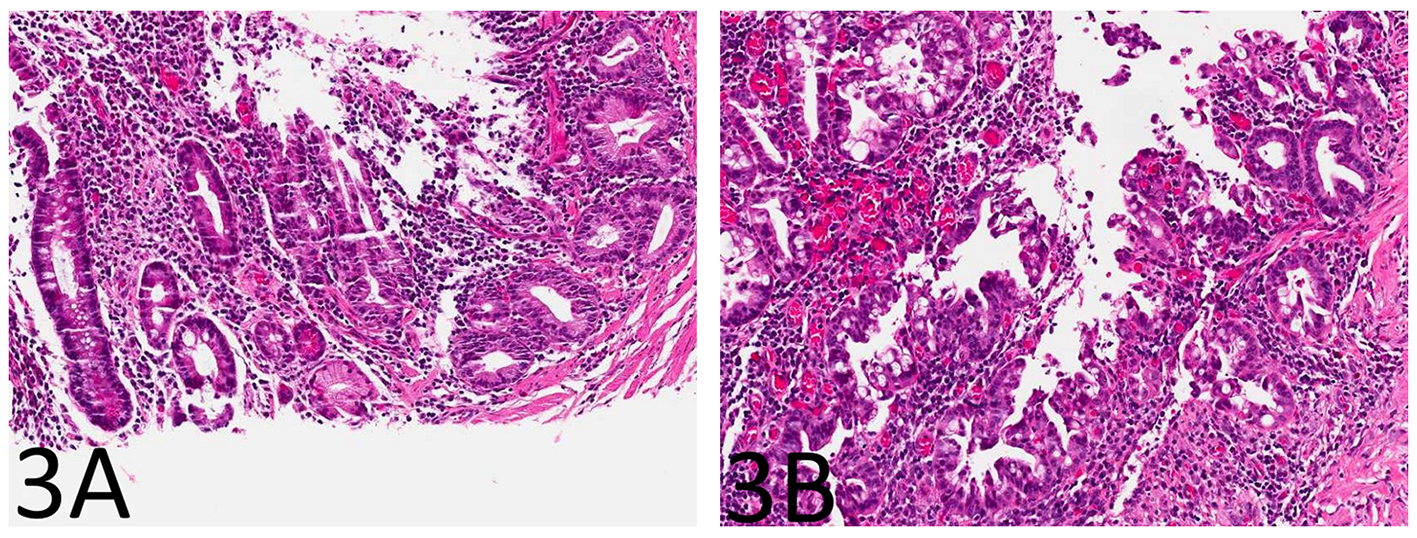
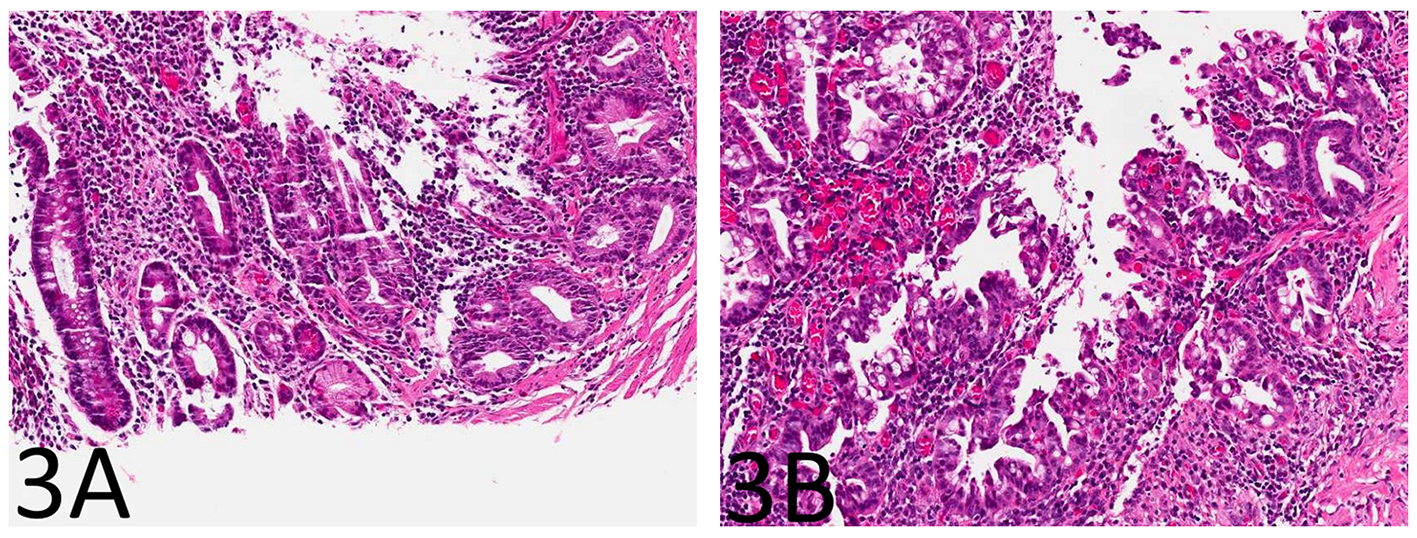
Figure 3. The small bowel mucosa from the area adjacent to the stricture shows chronic active enteritis with focal pyloric gland metaplasia (A: H&E stain, × 100) and areas of low-grade dysplasia and high-grade dysplasia resembling the epithelial lining of the enteritis cystic profunda (B: H&E stain, × 100).
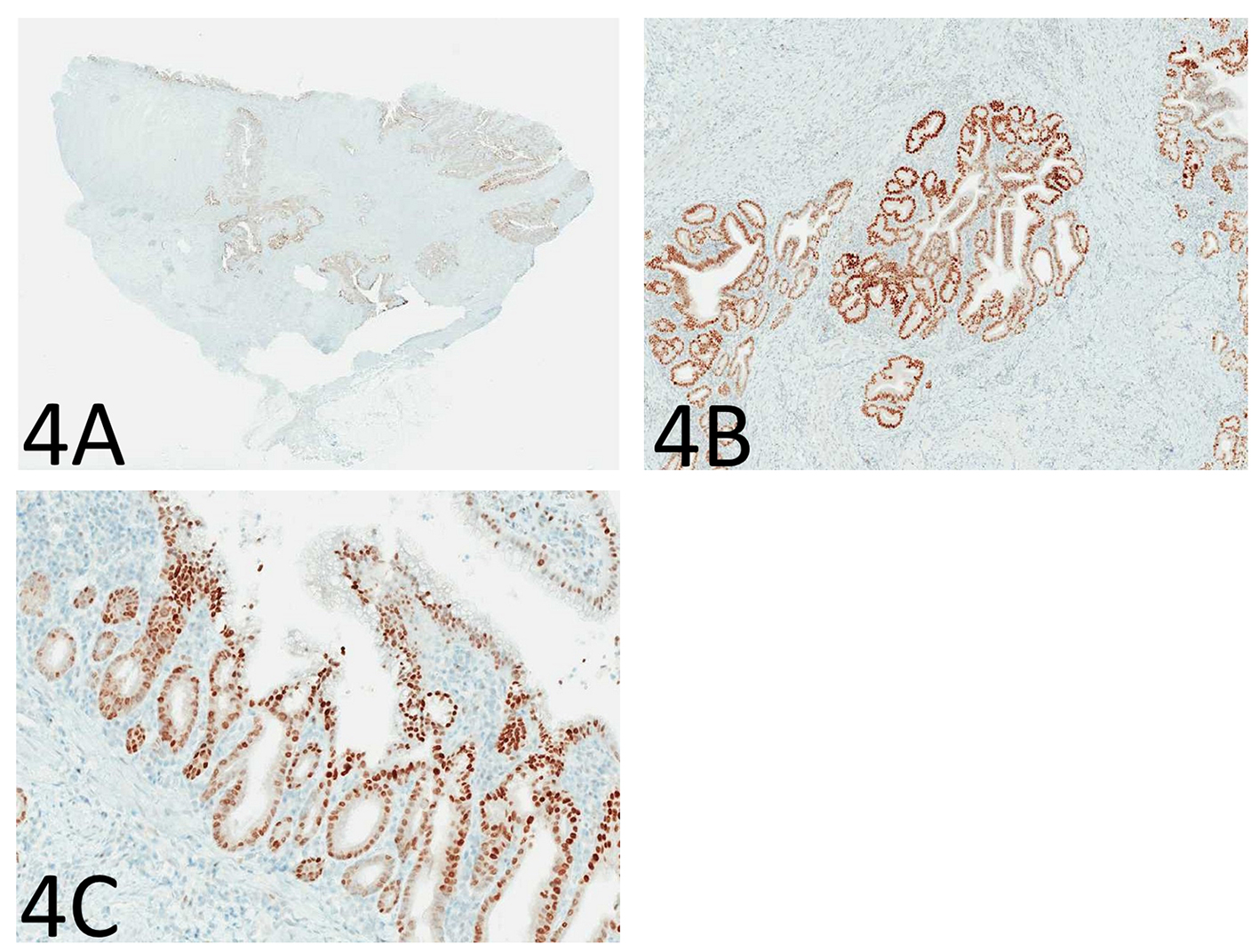
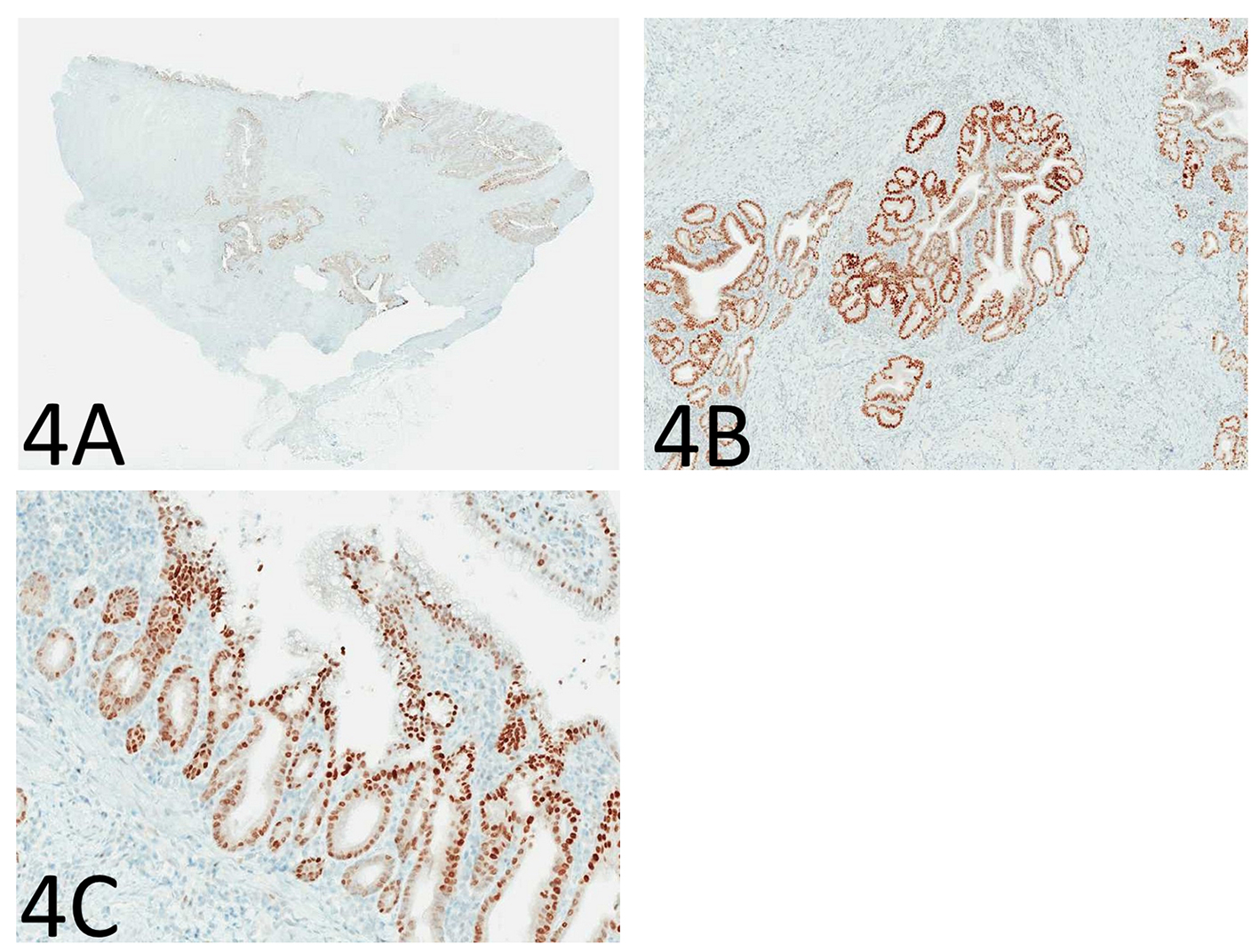
Figure 4. Immunohistochemistry for p53 shows diffuse and strong nuclear immunoreactivity in the epithelium of the enteritis cystica profunda (A: immunoperoxidase stain, × 40; B: immunoperoxidase stain, × 100) as well as its overlying mucosa (C: immunoperoxidase stain, × 100), supporting the neoplastic nature of the epithelium.
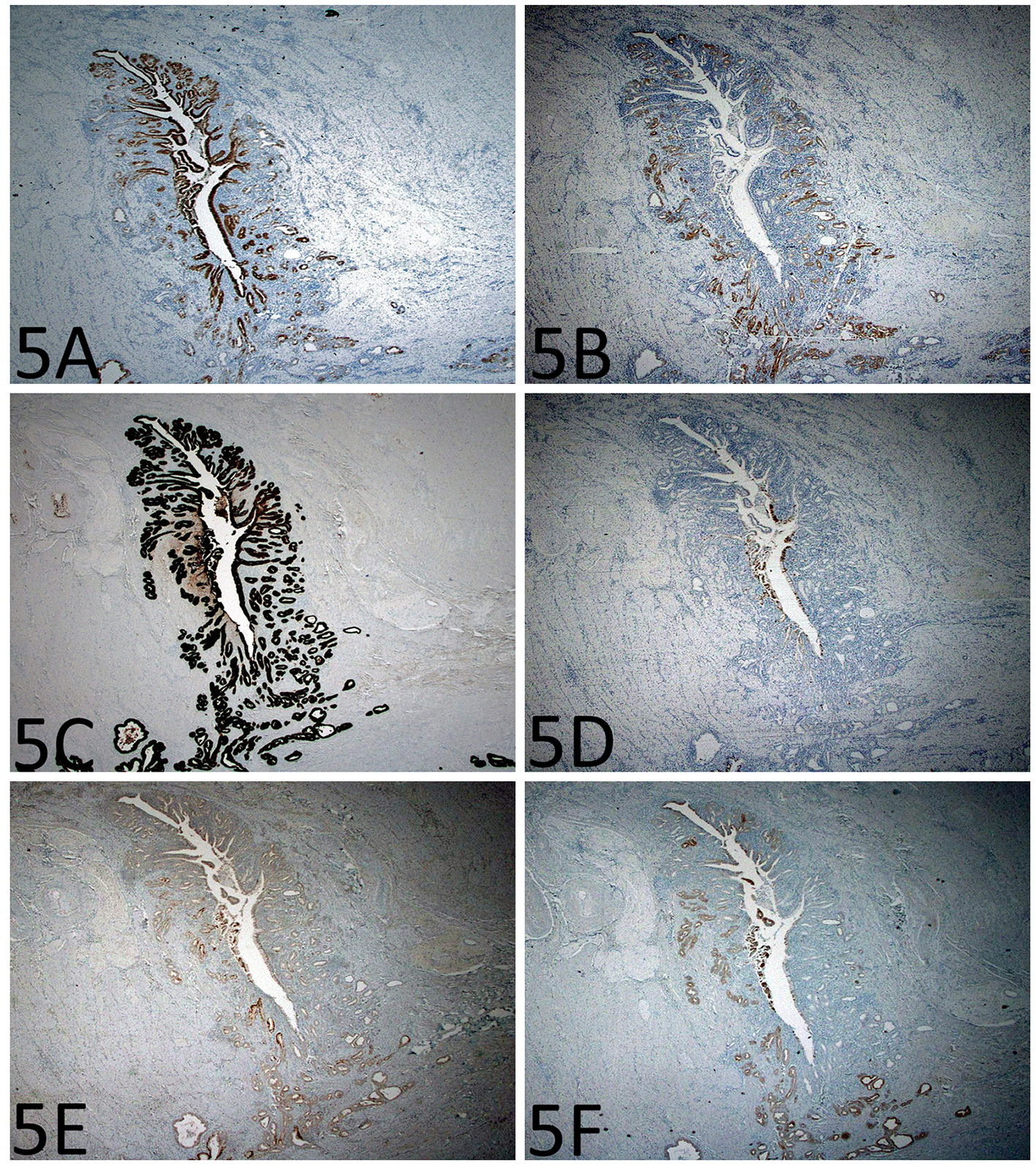
Figure 5. Immunohistochemistry shows gastric differentiation in the epithelium of the enteritis cystica profunda. (A) MUC5AC immunoreactivity in the foveolar type epithelium (immunoperoxidase stain, × 200). (B) MUC6 immunoreactivity in the mucus glands (immunoperoxidase stain, × 200). (C-F) There is strong CK7 immunoreactivity, but only focal CDX2, MUC2, and CK20 immunoreactivity (immunoperoxidase stain, × 200).
Table
Table 1. Antibodies Used for Immunohistochemical Analysis
| Antigen | Clone/antibody | Dilution | Source |
|---|
| p53 | Clone: DO-7
Catalog no.: M7001 | 1:20 | Dako |
| Cytokeratin 7 | Clone: OV-TL 12/30
Catalog no.: M7018 | 1:40 | Dako |
| Cytokeratin 20 | Clone: Ks20.8
Catalog no.: M7019 | 1:20 | Dako |
| CDX2 | Clone: CDX2-88 | 1:100 | Biogenex |
| MUC2 | CCP58 | 1:25 | NovoCastra, UK |
| MUC5AC | CLH2 | 1:25 | NovoCastra, UK |
| MUC6 | CLH5 | 1:25 | NovoCastra, UK |