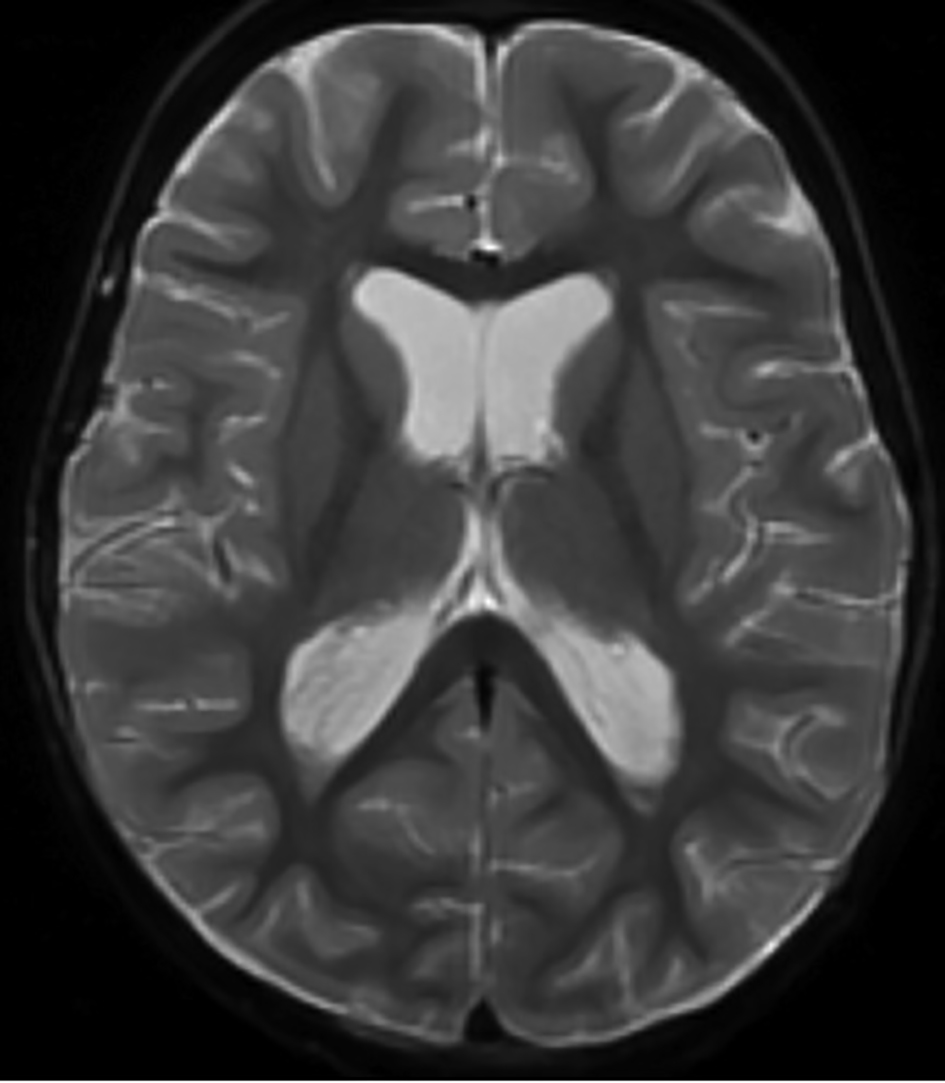
Figure 1. Magnetic resonance imaging of the brain showing intraventricular T2 hypointense signal compatible with intraventricular hemorrhage. Dependent layering is seen within the occipital horns of the lateral ventricles.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 10, October 2016, pages 461-466
Central Nervous System Hemorrhage Following Lumbar Puncture for Intrathecal Chemotherapy in a Pediatric Oncology Patient
Figures
Table
| Author | Case | Hemorrhagic complication | Procedure | Coagulation disorder | Neurologic deficit, therapies, and outcome |
|---|---|---|---|---|---|
| ALL: acute lymphoblastic lymphoma; LP: lumbar puncture; MRI: magnetic resonance imaging; IT: intrathecal. | |||||
| Hatzipantelis et al [7] | 5-year-old boy with ALL | Epidural hematoma | LP | Thrombocytopenia | Headache and lower back pain with paraparesis, decreased sensation of both legs, and urinary retention after LP. Sensation of lower extremities was recovered quickly, whereas motor function of legs improved gradually. Urinary retention followed a slower course of recovery. |
| Adler et al [9] | 5-year-old boy | Epidural hematoma | LP for fever evaluation | None | Pain in the legs and back. MRI revealed epidural blood extending from L4-5 up to L2 with compression of the thecal sac. There was no progression of his neurologic symptoms and no surgical intervention was deemed necessary. |
| Boran et al [13] | 6-year-old boy with non-Hodgkin lymphoma | Fronto-parietal hematoma | LP for IT chemotherapy | None | Right hemiparesis and focal seizures. Neurosurgery team recommended surgical evacuation of the hematoma, but the parents refused. The intracerebral hematoma resolved spontaneously over 6 weeks and the patient’s symptoms improved. |
| Tubbs et al [14] | Preterm infant | Conus medullaris hematoma | LP | None | Spontaneous movement of the lower extremities decreased after LP. Residual neurologic deficit with lower extremity paresis and incontinence of bowel and bladder. |
| Wirtz et al [15] | 12-year-old boy | Spinal subdural hematoma | LP | Thrombocytopenia | Lower back pain, leg weakness, and urinary retention developed after LP. Surgical laminectomy was performed from T11 to L2 with partial evacuation of the hematoma. After surgery, his neurologic condition gradually improved. He was able to walk without support and urinary retention had resolved. |