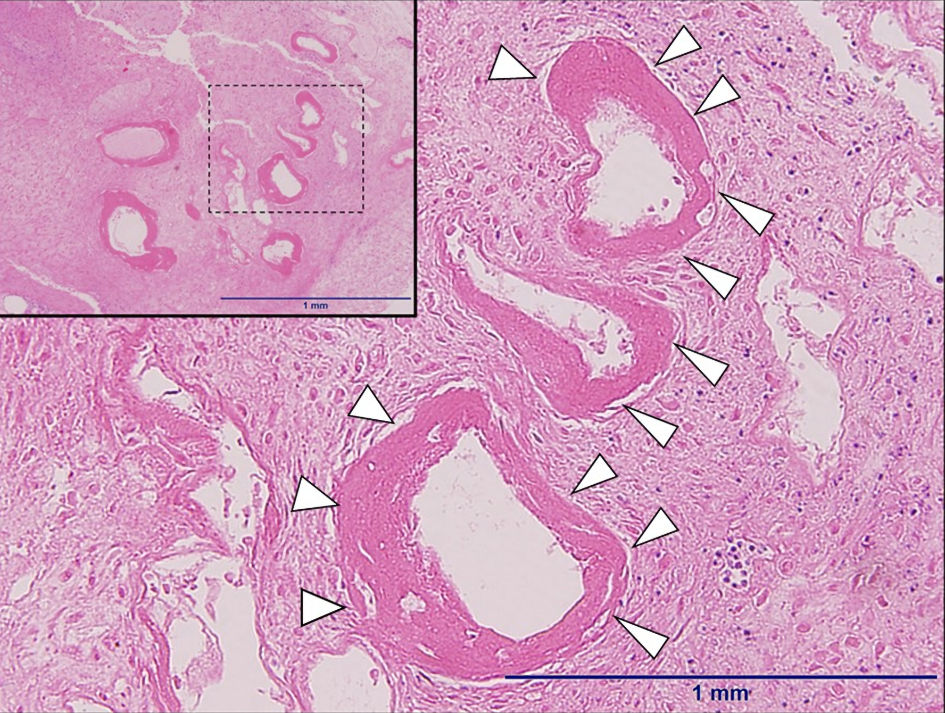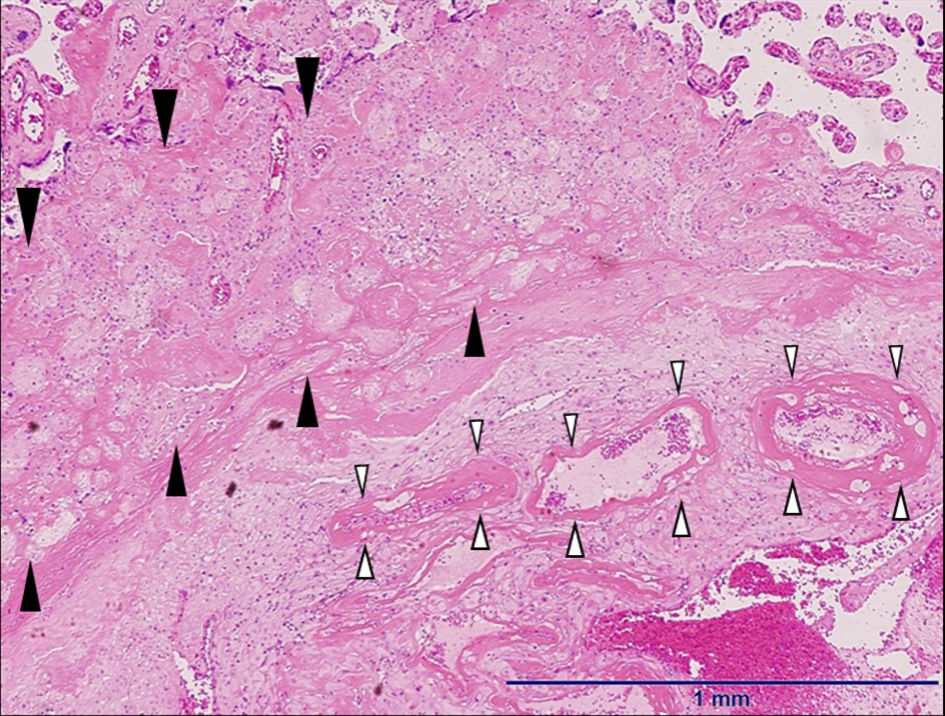
Figure 1. The microscopic findings of the placenta (hematoxylin and eosin stain, × 4). The pathology of the placenta shows fibrin deposition of intervillous space and fibrinoid necrosis of terminal villus called placental circulatory failure with ischemic changes (black arrow heads). Fibrinoid necrosis was observed around the small maternal arteries in the decidua of the placental site (white arrow heads).