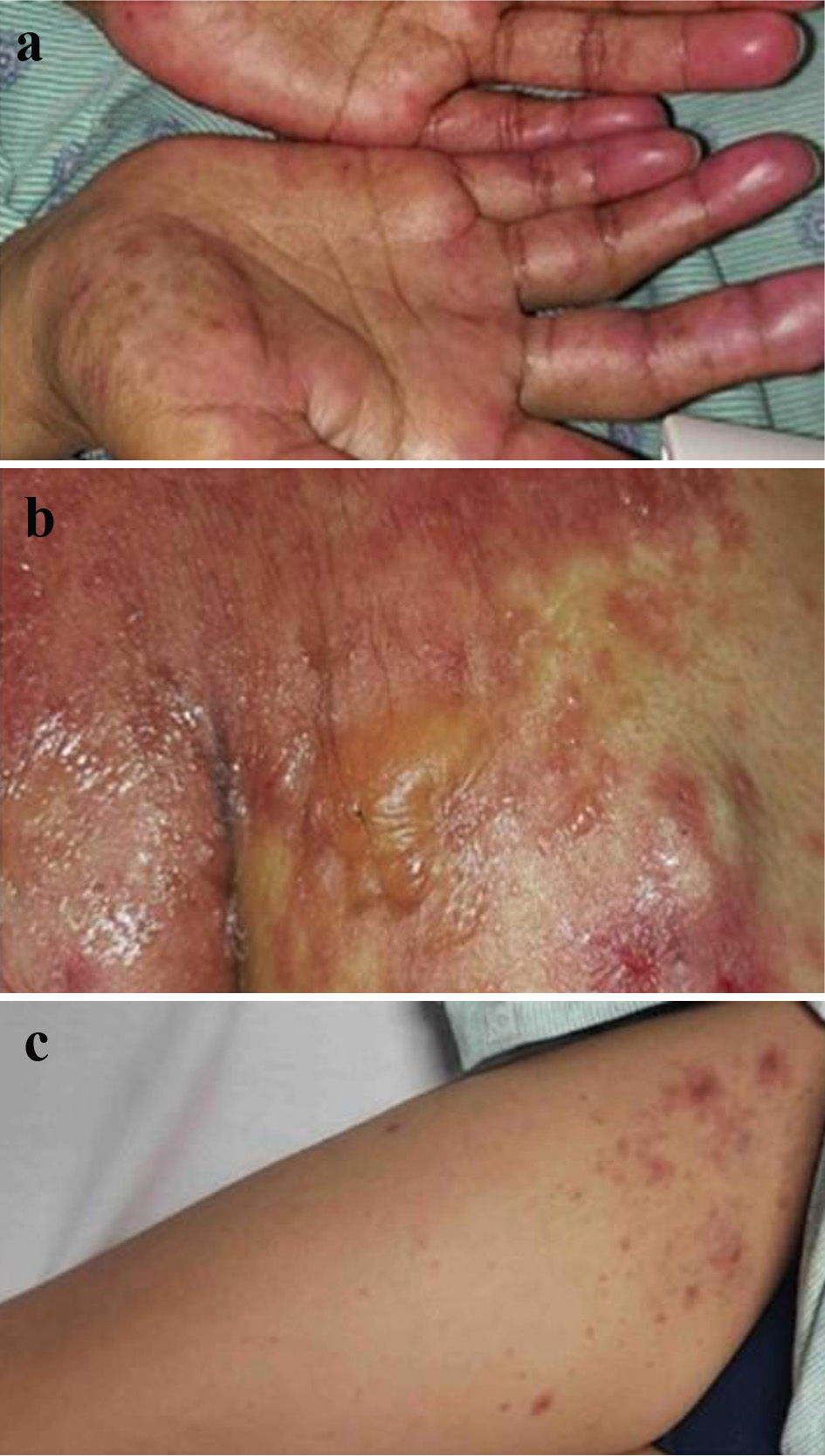
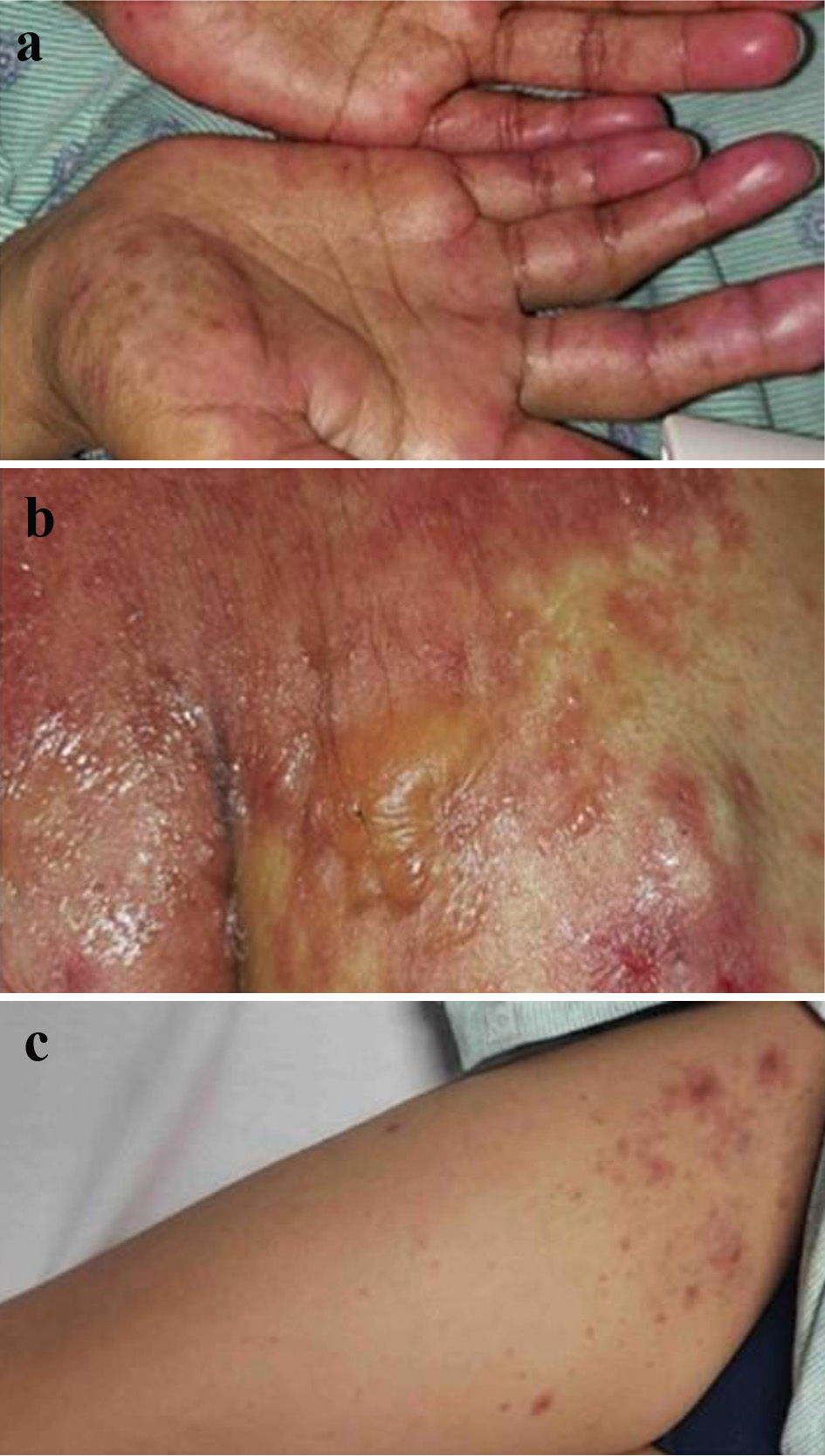
Figure 1. (a) A confluent papular rash over both hands. (b) Erupted rash with vesicles and bullae over the right shoulder. (c) A maculopapular rash over the right upper extremity.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 13, Number 9, September 2022, pages 449-455
Steven-Johnson Syndrome: A Rare but Serious Adverse Event of Nivolumab Use in a Patient With Metastatic Gastric Adenocarcinoma
Figure
Tables
| Blood test | Patient’s result | Reference result |
|---|---|---|
| Venous lactate | 2.1 mmol/L | 0.6 - 2.1 mmol/L |
| Serum bicarbonate | 14.0 mmol/L | 21.0 - 28.0 mmol/L |
| Serum anion gap | 10.0 mmol/L | 6.0 - 14.0 mmol/L |
| Serum creatinine | 1.30 mg/dL | 0.6 - 1.30 mg/dL |
| Serum sodium | 130 mmol/L | 133 - 144 mmol/L |
| Serum chloride | 99 mmol/L | 98 - 107 mmol/L |
| Serum potassium | 4.6 mmol/L | 3.5 - 5.2 mmol/L |
| Blood urea | 23.0 mg/dL | 8.6 - 25.0 mg/dL |
| Serum magnesium | 1.4 mg/dL | 1.5 - 2.6 mg/dL |
| Serum phosphate | 4.1 mg/dL | 2.5 - 4.5 mg/dL |
| Serum uric acid | 6.9 mg/dL | 4.4 - 7.6 mg/dL |
| Hemoglobin | 9.5 g/dL | 13.0 - 15.0 g/dL |
| Platelets | 103 × 103/mm3 | 150 - 450 × 103/mm3 |
| White blood cell | 1.8 × 103/mm3 | 4.0 - 11.0 × 103/mm3 |
| Serum albumin | 3.8 g/dL | 3.5 - 5.7 g/dL |
| Procalcitonin | 0.60 ng/mL | 0.20 - 0.49 ng/mL |
| Cutaneous irAE | Patients number | Time to onset from the last cycle of anti-PD-1 agents (weeks) |
|---|---|---|
| aSix patients had more than one specific skin reaction. irAEs: immune-related adverse effects; SJS: Steven-Johnson syndrome; TEN: toxic epidermal necrolysis; anti-PD-1: anti-programmed cell death receptor-1. | ||
| Pigmentation changes/vitiligo | 58 | 1 - 36 |
| Psoriasis | 33 | 2 - 22 |
| Bullous pemphigoid | 31 | 3 - 84 |
| Lichenoid dermatitis | 30 | < 1 - 92 |
| Granulomatous reactions | 10 | 4 - 40 |
| Erythema multiforme/SJS/TEN | 10 | < 1 - 20 |
| Lupus erythematosus-like rash | 8 | 4 - 43 |
| Authors, year of publication | Patient’s age (years/gender | Underlying malignancy | Latency of onset of SJS/TEN symptoms | Management | Outcome of SJS/TEN |
|---|---|---|---|---|---|
| HCC: hepatocellular carcinoma; SCC: squamous cell carcinoma; NSCLC: non-small cell lung carcinoma; SJS: Steven-Johnson syndrome; TEN: toxic epidermal necrolysis; anti-PD-1: anti-programmed cell death receptor-1; ICU: intensive care unit. | |||||
| Vivar et al, 2017 [12] | 50/male | Metastatic malignant melanoma treated with dual anti-PD-1 agents (ipilimumab and nivolumab) | Initial clinical and pathological findings were consistent with a morbilliform drug rash which then progressed over 3 months to clinicopathological TEN. SCORTEN 5. | Poor response to infliximab and oral prednisone, followed by high-dose methylprednisolone and immunoglobulins | Lack of response of cutaneous lesions to immunosuppressive therapy with global clinical condition’s decline from polymicrobial sepsis. Death from multiorgan failure. |
| Kim et al, 2021 [13] | 86/male | Metastatic HCC | Mucocutaneous lesions appeared after 14 days of the second cycle. Histology confirmed TEN. SCORTEN 3, mortality rate 35.5%. | Failure of oral prednisone. ICU admission with high-dose methylprednisolone and immunoglobulins | Initial re-epithelization of some skin lesions but overall clinical course deteriorated due to polymicrobial sepsis and advanced HCC. Death from multiorgan failure. |
| Dasanu, 2019 [14] | 69/male | Metastatic HCC status post resection and recurrent tumor arterial embolization | Late onset of mucocutaneous lesions after 4 months (eight cycles) of nivolumab. Histology confirmed SJS. | Oral prednisone and supportive care | Complete resolution of mucocutaneous lesions within 3 weeks of treatment |
| Griffin et al, 2018 [15] | 54/male | Recurrent follicular lymphoma | Mucocutaneous lesions appeared after 10 days of the first cycle. Histology confirmed TEN. SCORTEN 3, mortality rate 32%. | High-dose methylprednisolone followed by oral prednisone and supportive care | Initial rash improvement followed by TEN of respiratory mucosa, hospital-acquired cases of pneumonia leading to progressive respiratory failure and death |
| Garcia-Canzana et al, 2021 [16] | 78/male | Metastatic SCC lung | Mucocutaneous lesions and constitutional symptoms 1 week after the second cycle. Histology confirmed SJS. | High-dose methylprednisolone followed by oral prednisone with tapering, and supportive care | Complete disappearance of mucocutaneous lesions after 1 month |
| Koshizuka et al, 2021 [17] | 76/male | Metastatic SCC tongue status post resection and neck dissection, radiotherapy, and chemotherapy | Cutaneous lesions appeared after 27 days of the first cycle followed by the constitutional symptoms. Histology confirmed SJS. TEN was clinically diagnosed later in the second week of symptoms onset. | High-dose methylprednisolone followed by oral prednisone with gradual tapering and supportive care | Gradual improvement of rash with epithelization of the erupted lesions |
| Ito et al, 2017 [18] | 76/female | Stage IV NSCLC | The unspecified onset of cutaneous lesions after the second cycle. SJS was complicated by refractory pruritis. Histology confirmed SJS. | Oral prednisone for 2 weeks and a topical steroid with supportive care | Complete disappearance of the rash but refractory pruritis that was, interestingly, aprepitant-responsive. |
| Salati et al, 2018 [19] | 59/female | Metastatic NSCLC status post chemotherapy | Mucosal lesions and constitutional symptoms 1 week after the second cycle followed by a diffuse eruptive rash. | High-dose methylprednisolone and supportive care | Gradual rash improvement and skin healing |
| Shah et al, 2018 [20] | 63/male | Stage IV SCC of uvula and soft palate status post neck dissection and local radiotherapy | Mucosal and cutaneous lesions appeared after 1 week after the first cycle. Skin rash distributed over recent radiation sites. Histology confirmed SJS. | Supportive care only | Good outcome of SJS rash |
| Rouyer et al, 2018 [21] | 63/male | Recurrent pulmonary epidermoid carcinoma status post palliative radiotherapy and immunotherapy | Oral mucositis after 5 days from the second cycle and cutaneous lesions after 2 weeks, the rash appeared over previous radiation sites. Histology confirmed SJS with recall radiation dermatitis. | Unspecified | Unspecified |
| Nayar et al, 2016 [22] | 64/female | Metastatic malignant melanoma refractory to ipilimumab therapy | Initial morbilliform rash that appeared after 2 weeks from the second cycle of nivolumab. The rash progressed into diffuse eruptive rash over 2 weeks with histology confirmed SJS. | High-dose methylprednisolone and immunoglobulins initially, followed by cyclosporin and oral prednisone taper | Gradual improvement of the skin rash. |
| Question | Yes | No | Do not know | Score |
|---|---|---|---|---|
| Total score ≥ 9: definite. 5 - 8: probable. 1 - 4: possible. ≤ 0: doubtful. | ||||
| 1. Are there previous conclusive reports on this reaction? | +1 | 0 | 0 | +1 |
| 2. Did the adverse event appear after the suspected drug was administered? | +2 | -1 | 0 | +2 |
| 3. Did the adverse reaction improve when the drug was discontinued or a specific antagonist was administered? | +1 | 0 | 0 | +1 |
| 4. Did the adverse event reappear when the drug was re-administered? | +2 | -1 | 0 | 0 |
| 5. Are there alternative causes (other than the drug) that could on their own have caused the reaction? | -1 | +2 | 0 | +2 |
| 6. Did the reaction reappear when a placebo was given? | -1 | +1 | 0 | +1 |
| 7. Was the drug detected in blood (or other fluids) in concentrations known to be toxic? | +1 | 0 | 0 | 0 |
| 8. Was the reaction more severe when the dose was increased or less severe when the dose was decreased? | +1 | 0 | 0 | 0 |
| 9. Did the patient have a similar reaction to the same or similar drugs in any previous exposure? | +1 | 0 | 0 | 0 |
| 10. Was the adverse event confirmed by any objective evidence? | +1 | 0 | 0 | 0 |
| Total score | +7 | |||