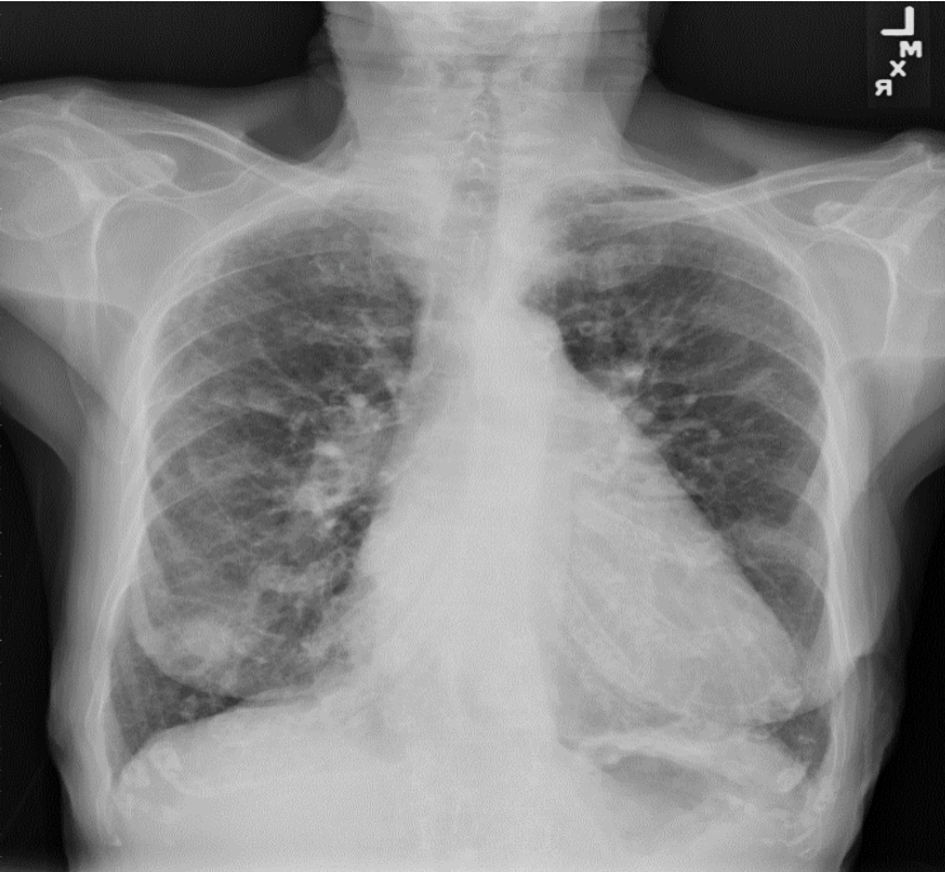
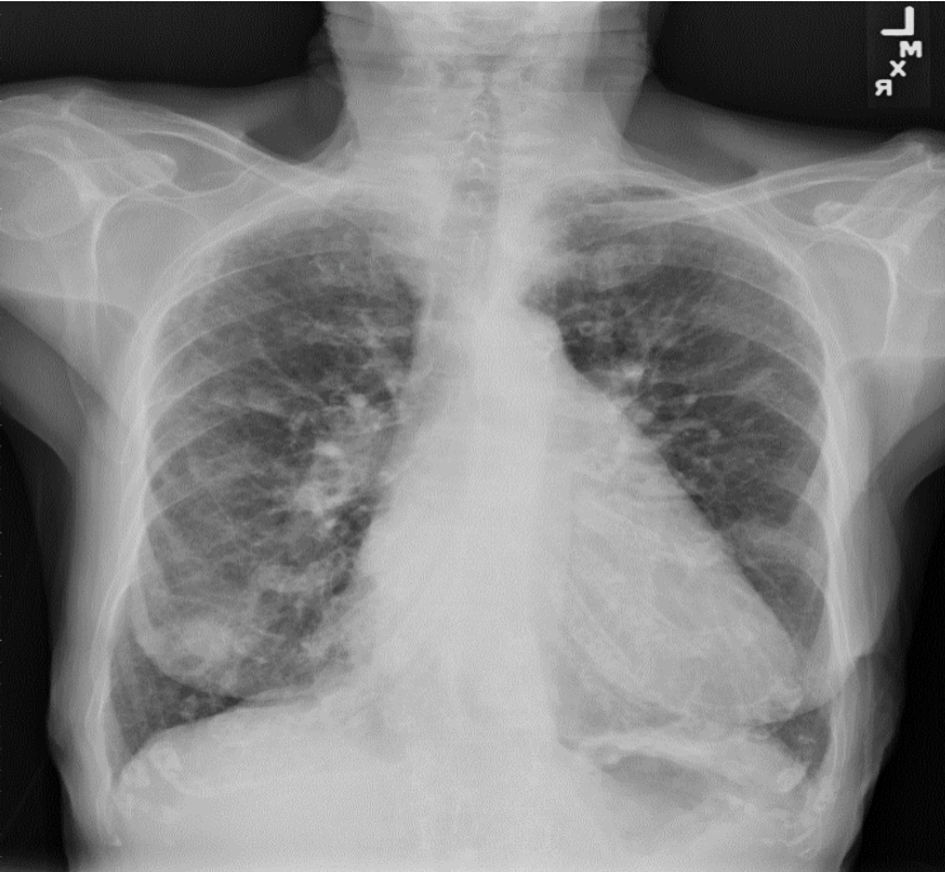
Figure 1. Chest X-ray showed extensive pulmonary nodulo- reticular shadowing at the peripheries signifying extensive fibrotic changes with scattered nodules.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 1, January 2023, pages 36-43
Uncommon Presentation of Undiagnosed B-Cell Lymphoproliferative Disorder as Nodular Pulmonary Amyloidosis
Figures

Table
| Study name and year | Age (years)/sex (M or F) | Presenting features | Primary tumor | Immunostaining profile in addition to pathologic diagnosis of amyloidosis | Treatment | Outcome |
|---|---|---|---|---|---|---|
| F: female; M: male; H. pylori: Helicobacter pylori; +: positive; MALT: mucosa-associated lymphoid tissue; RLL: right lower lobe; PMH: past medical history; CXR: chest X-ray; AL: immunoglobulin light chain amyloidosis; IgH: immunoglobulin heavy chain; UV: ultraviolet; CCL: centrocyte-like. | ||||||
| Core et al, 2017 [22] | 69/F | Progressive dyspnea, hypoxemia, dry cough, weight loss, bilateral crackles and wheezes upon auscultation, + respiratory distress | Extranodal marginal zone B cell lymphoma of MALT type with bilateral nodular pulmonary amyloidosis | Lymphocytic cells (CD20+) with scattered atypical plasma cells (kappa+, lambda+, CD138+) | RLL wedge resection by video-assisted thoracoscopic surgery, bortezomib, cyclophosphamide, dexamethasone, glucocorticoids, rituximab | Improved in the first 6 months; later worsened with acute on chronic respiratory failure |
| Xiang et al, 2015 [23] | 59/M | Asymptomatic | Pulmonary MALT lymphoma of the left lower lobe | Lymphocytes (+ for CD79a, CD20, CD138, bcl-2, lambda light chain, CD43) | Left lower lobectomy with mediastinal lymphadenectomy | No recurrence or metastasis reported 14 months after initial diagnosis |
| Filippi et al, 2019 [24] | 50/M | Hemoptysis | Primary pulmonary MALT lymphoma with pulmonary amyloidosis | B cells (+ for CD79a, CD20, and lambda light chain) | Left upper lobectomy | No local recurrence or metastasis in 2-year follow-up period |
| Moriyama et al, 2000 [25] | 63/F | Asymptomatic | MALT lymphoma of the anterior mediastinum (thymus) with nodular pulmonary amyloidosis of the lung | Lobular structures within Hassall’s corpuscles (keratin+). Few plasma cells (+ for IgG and kappa light chain) along with medium CCL cells (B cell phenotype + for CD20 and CD79a) | Complete thymus resection by sternotomy, resection of lung nodules by left thoracotomy | No recurrence of lymphoma in 47-month follow-up period |
| Lantuejoul et al, 2007 [26] | 50/F | Asymptomatic with PMH of MALT-type gastric lymphoma due to H. pylori. CXR showed incidental multiple pulmonary nodules. | MALT-type marginal zone lymphoma involving gastrointestinal tract, bone marrow and lungs (stage IV) | Giant cells, crushed plasma cells with thioflavin T staining under UV light, small plasmacytoid lymphocytes, and large lymphocytes (CD20+) | Surgical resection of pulmonary nodules with adjuvant chemotherapy (rituximab), and bone marrow transplantation | No change in nodules and cysts on radiography during the 17-month follow-up period |
| Davis et al, 1991 [27] | 56/M | Left upper chest pain, hemoptysis, significant smoking history, wheezes over the left upper chest upon auscultation | Small cell non-Hodgkin’s left pulmonary lymphoma with bilateral lung nodules (nodular pulmonary amyloidosis) | Lymphocytic foci with plasma cells, and giant cells (+ for leukocyte common antigen). Both the lymphoma and the amyloidomas showed cells with kappa light chains. | Thoracotomy and wedge resection of two left upper lung lobe nodules, prednisone, chlorambucil | Hilar mass and amyloid pulmonary nodules decreased in size on radiography during follow-up |
| Wieker et al, 2002 [28] | 63/F | Significant PMH of MALT-type lymphoma of right upper eyelid | MALT-type lymphoma (low grade) of the right upper eyelid with AL amyloid deposits | Lymphocytic cell infiltrated with plasma cells (+ for Ki-B3, CD20, CD79a, IgM and h-light chain) | Cyclophosphamide, doxorubicin, hydroxydaunorubicin, oncovin and prednisone | No change in number and size of the pulmonary nodules at 6 months and 18 months follow-up |
| Kawashima et al, 2005 [29] | 75/F | Asymptomatic | Non-Hodgkin’s primary pulmonary MALT-type lymphoma of the right lung with nodular pulmonary amyloidosis | B lymphocytes (+ for L26 and CD79) | Partial resection and enucleation of right middle lobe nodules with lobectomy of the right middle and lower lobes | No recurrence of MALT lymphoma at 4-year follow-up |
| Ihling et al, 1996 [30] | 67/M | Asymptomatic with PMH of lymphoplasmacytic immunocytoma in the lung and an abnormal lymphoid infiltrate in the bone marrow | Primary extranodal lymphoplasmacytic immunocytomas of the lung or the bronchus-associated lymphatic tissue with intrafocal tumor-like amyloidosis | Plasma cells between amyloid deposits (+ for lambda light chains), lymphocytes and plasma cells surrounding amyloid tumor (+ for kappa and lambda light chains), amplification of the IgH gene with sharp bands | No treatment as hematopoiesis was not affected | - |
| Ihling et al. 1996 [30] | 66/M | Asymptomatic with tumorous growths in the right lower and left lower lobes on chest X-ray | Primary extranodal lymphoplasmacytic immunocytomas of the lung or the bronchus-associated lymphatic tissue with intrafocal tumor-like amyloidosis | Plasma cells (+ for lambda and kappa light chains in equal frequency), lymphocytes from lung biopsy (CD20-reactive B-lymphocytes and CD3-reactive T-lymphocytes), amplification of the IgH with sharp bands | Removal of right lower lobe and mediastinal lymphadenectomy | - |