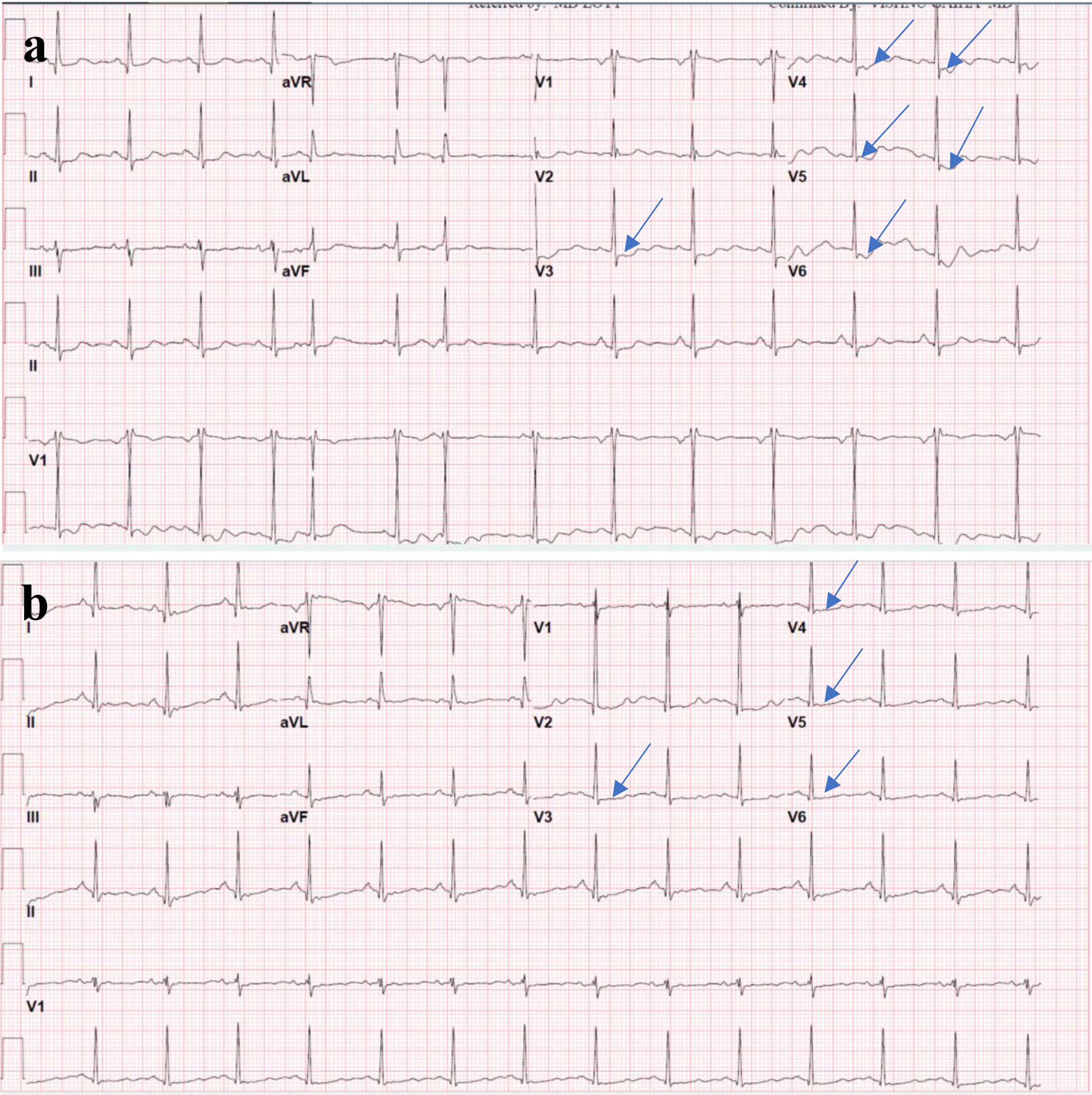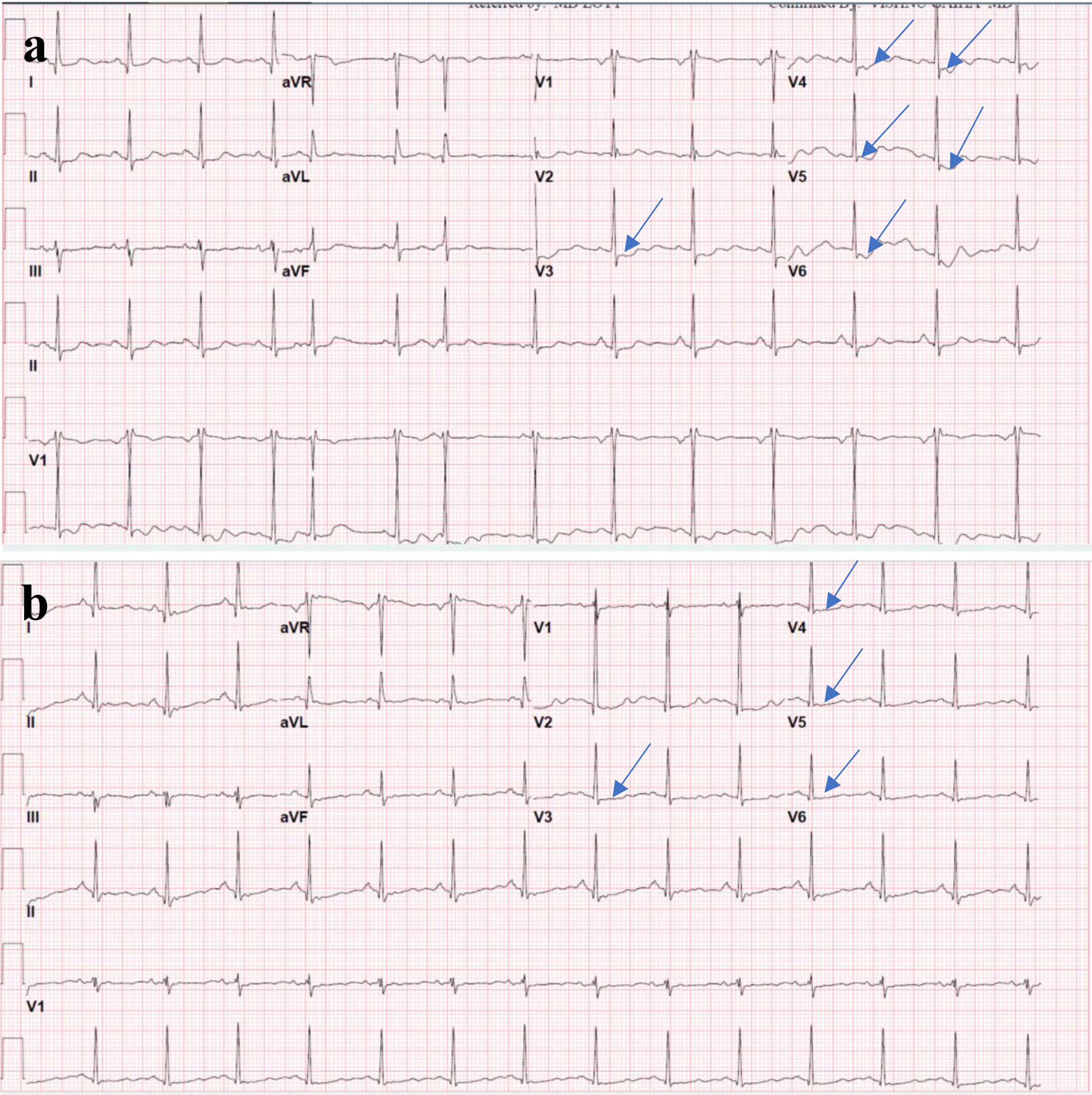
Figure 1. (a) ECG on presentation showing ST segment depression (arrows) in the anterolateral leads (V3-V6). (b) Repeat ECG on the next day showing improvement in the ST segment deviations noticed on the initial ECG. ECG: electrocardiogram.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 3, March 2023, pages 105-110
Subarachnoid Hemorrhage From Cavernous Malformation Masquerading as Myocardial Infarction
Figures