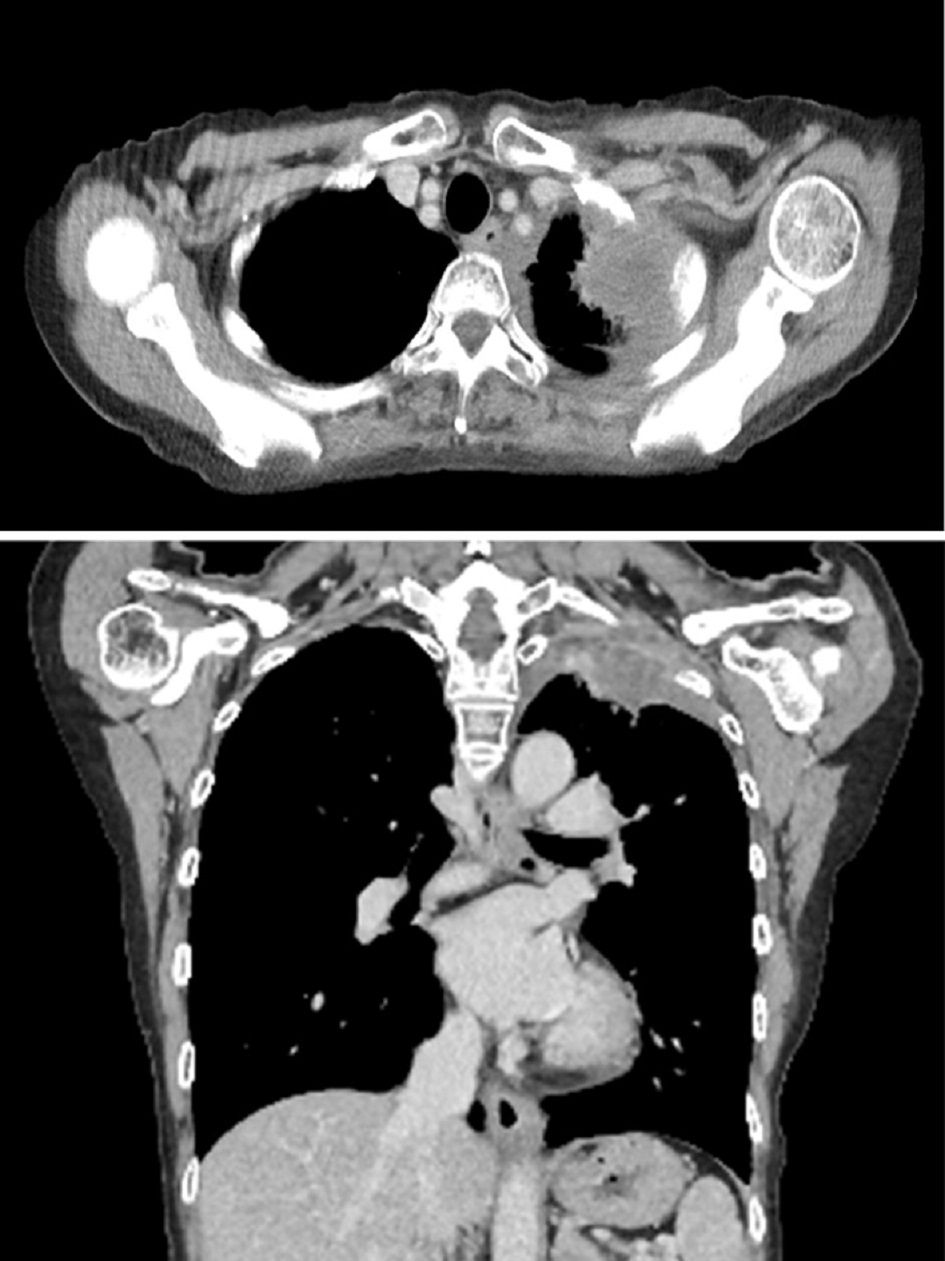
Figure 1. Contrast-enhanced computed tomography of the chest on admission. A 65 × 45 mm lesion with a heterogeneous contrast effect in S1+2 in the left upper lobe was observed. Tumor invasion was observed in the chest wall.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 4, April 2023, pages 111-117
Primary Squamous Cell Lung Cancer With Frequent Episodes of Sustained Ventricular Tachycardia due to Myocardial Metastasis
Figures
Table
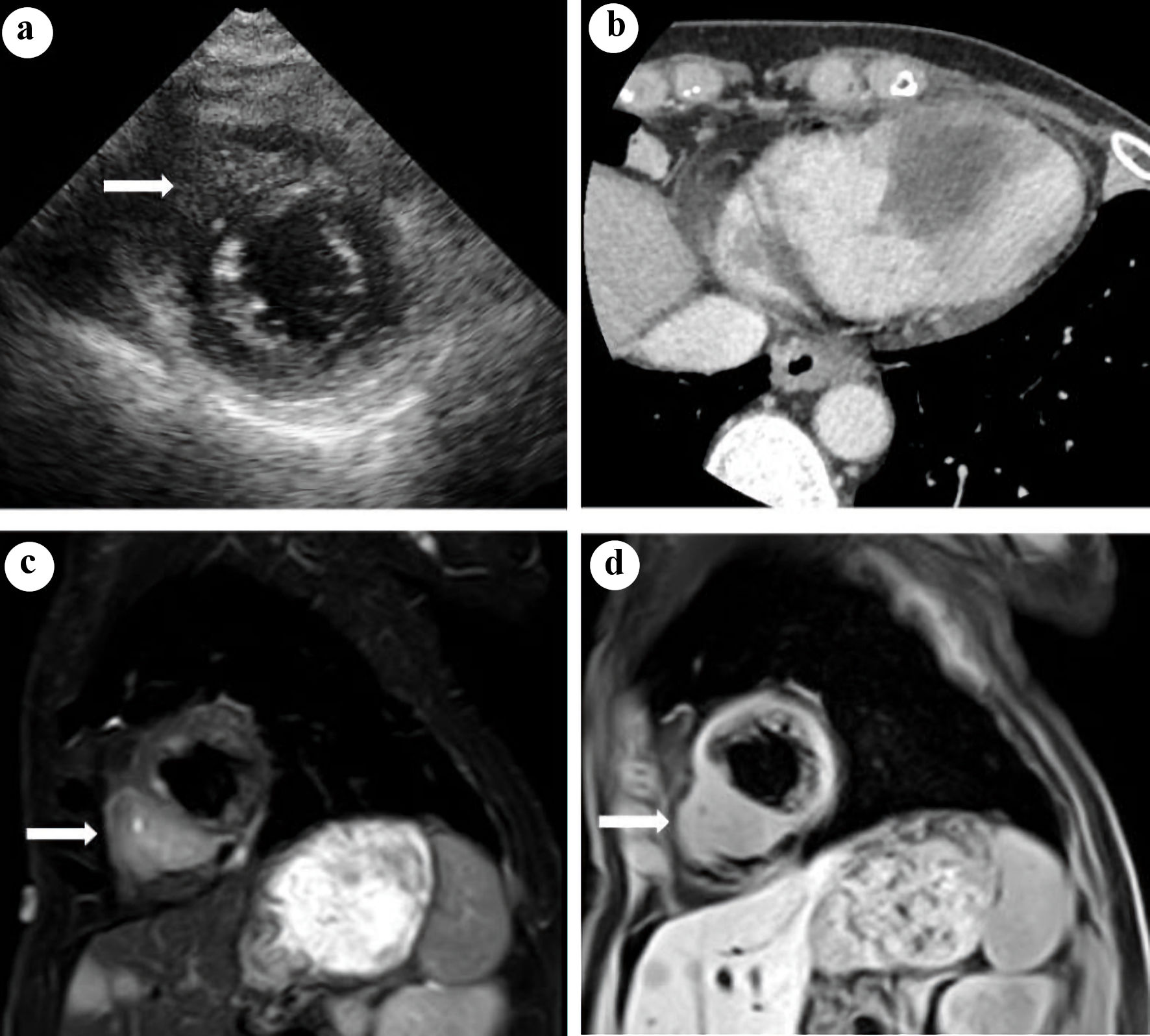
| No. | Age/gender | Histology | Location | PE | Diagnostic procedure | Distant metastasis | Treatment | Survival time from the diagnosis of VT | Reference |
|---|---|---|---|---|---|---|---|---|---|
| M: male; F: female; Sq: squamous cell carcinoma; Adsq: adenosquamous carcinoma; Ad: adenocarcinoma; RV: right ventricle; LV: left ventricle; PE: pericardial effusion; TTE: transthoracic echocardiography; CT: computed tomography; MRI: magnetic resonance imaging; FDG-PET: 18-fluorodeoxyglucose positron emission tomography; ADR: adrenal gland; RT: radiotherapy; VT: ventricular tachycardia. | |||||||||
| 1 | 66/M | Sq | RV | - | TTE, CT | Brain | Amiodarone, RT | 2 months | [16] |
| 2 | 49/F | Adsq | LV | + | TTE, MRI | Lung | Cardioversion, amiodarone | 18 months | [17] |
| 3 | 67/F | Sq | RV | + | TTE, MRI | Brain, bone | Amiodarone | 5 months | [18] |
| 4 | 66/F | Ad | LV | - | MRI, FDG-PET | - | Propranolol, RT | 18 months (alive) | [19] |
| 5 | 56/F | Sq | LV | - | TTE, CT, MRI | Bone, ADR lung, liver | Cardioversion | 3 weeks | Present case |