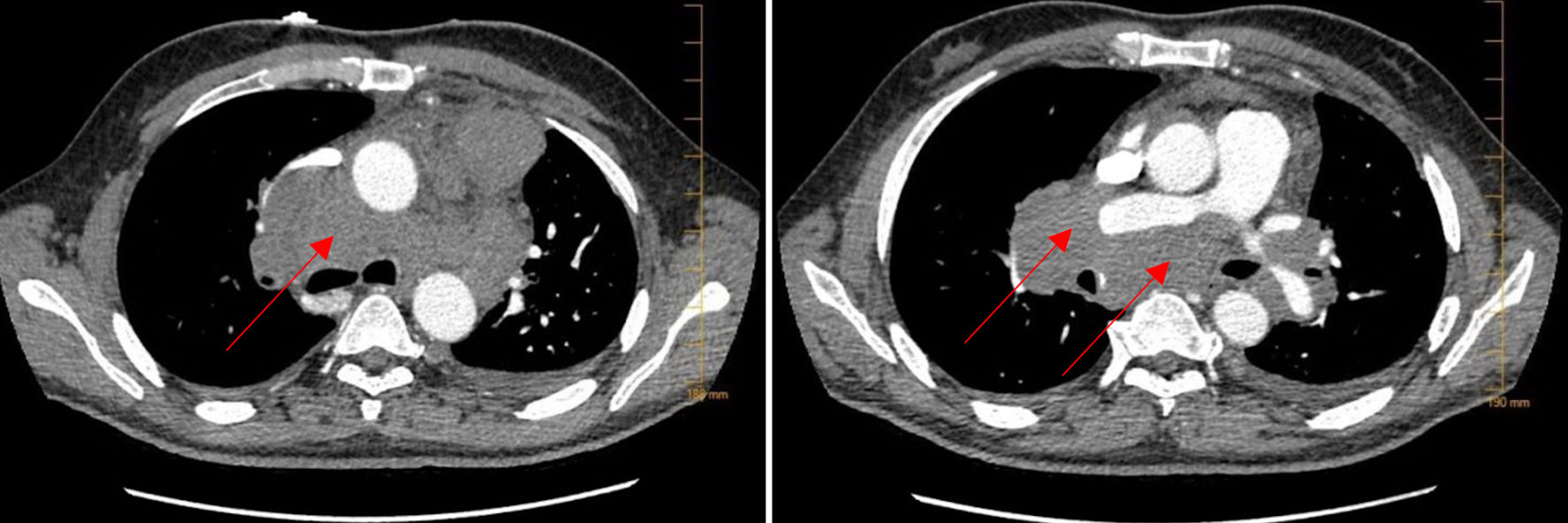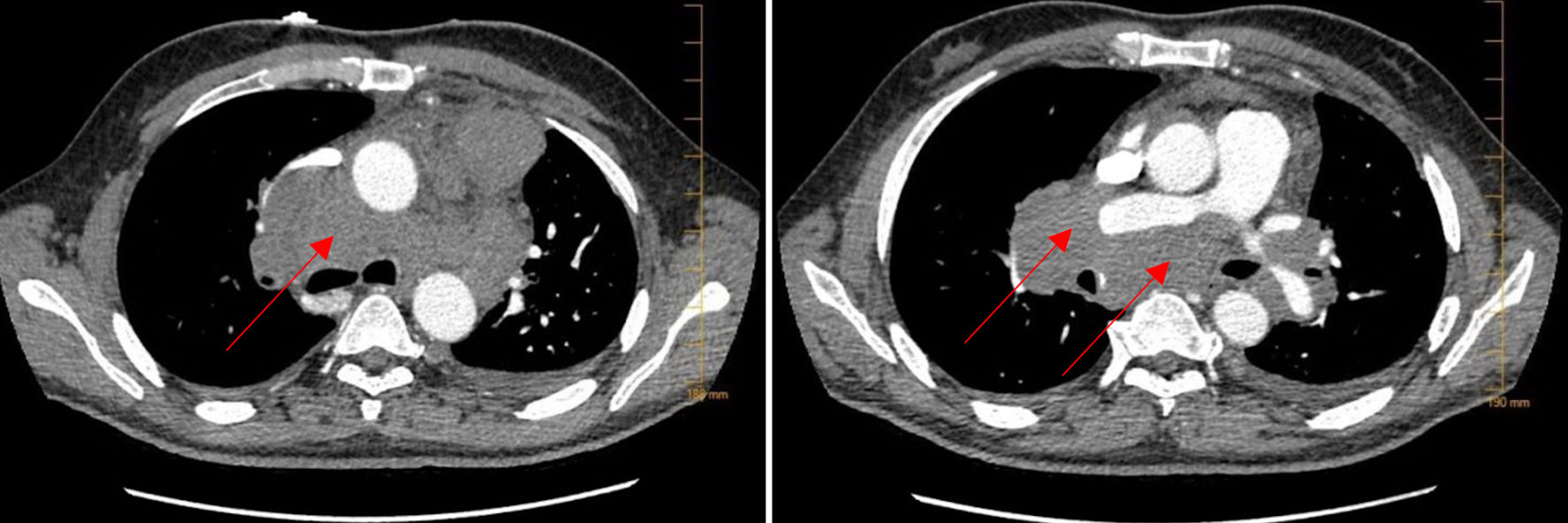
Figure 1. CTA of the lungs. CTA of the lungs on admission showed extensive bulky mediastinal and hilar lymphadenopathy with encasement of the pulmonary artery (arrows). CTA: computed tomography angiography.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 5, May 2023, pages 162-168
Vanishing Bile Duct Syndrome in a Patient With Recurrent Hodgkin Lymphoma
Figures