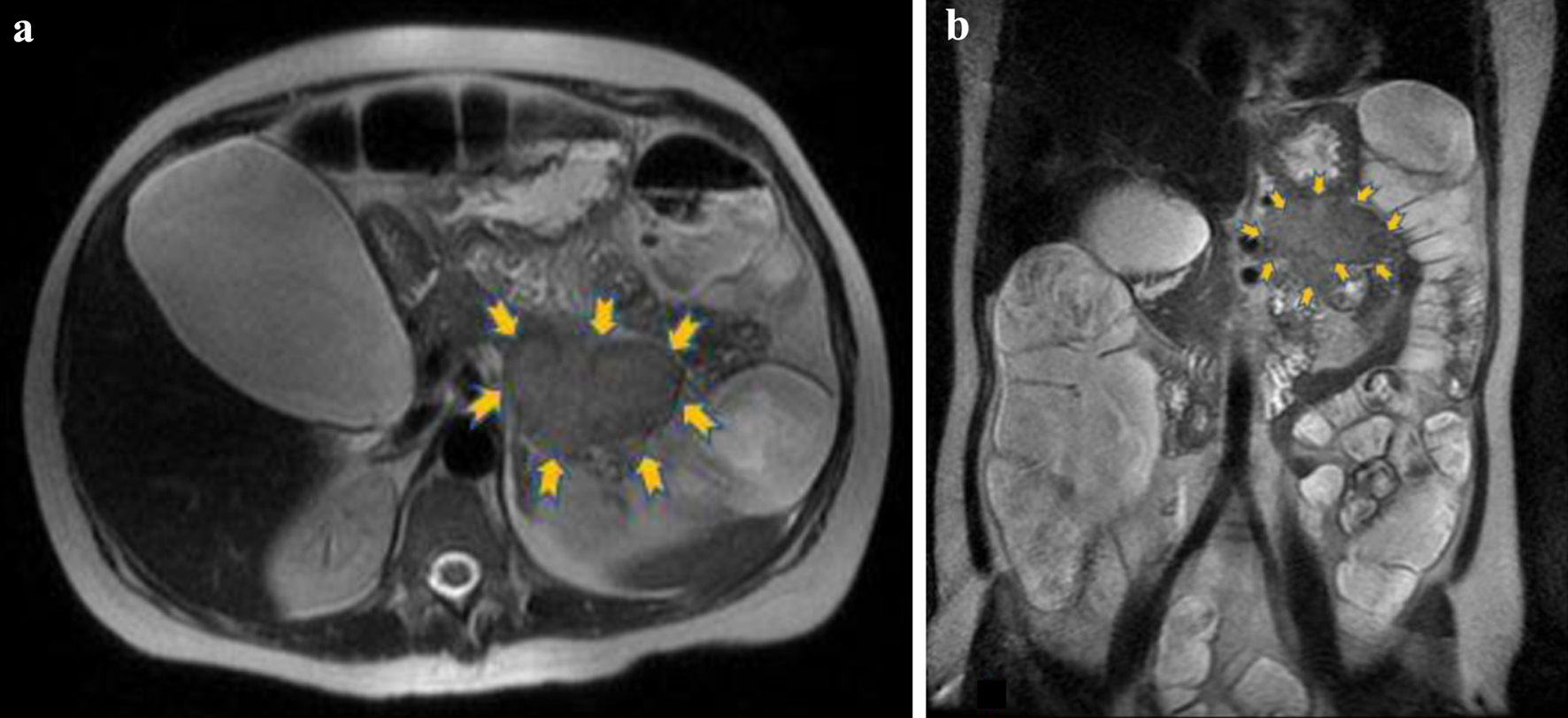
Figure 1. The lesion (6.3 × 5.1 cm) is located in the anatomic position of the pancreatic tail (yellow arrows) and presents intermediate signal intensity relative to pancreas. (a) Axial T2 and (b) coronal T2 magnetic resonance images.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 9-10, October 2023, pages 307-316
Pancreatic Vasoactive Intestinal Peptide-Producing Tumor as a Rare Cause of Acute Diarrhea and Severe Hypokalemia
Figures
Tables
| March 13, 2013 | Admission to the emergency department (ED) of our hospital with acute diarrhea and severe hypokalemia |
| March 19, 2013 | Diagnosis of tumor in the pancreatic tail with abdominal MRI |
| March 20, 2013 | Transfer of the patient to the Endocrinology Department of the collaborating oncology hospital |
| March 22, 2013 | Distal pancreatectomy with splenectomy |
| March 22, 2013 | Transfer to the intensive care unit (ICU) after surgical resection of the tumor |
| March 28, 2013 | Discharge from ICU and transfer to the Department of Surgery of the collaborating oncology hospital |
| April 3, 2013 | Hospital discharge of the patient from the oncology hospital |
| April 10, 2013 | Admission to the ED of our hospital with melena. Emergent esophagogastroduodenoscopy with endoscopic hemostasis of duodenal ulcer lesions. Computed tomography (CT) finding of cystic fluid collection in the retroperitoneal space. |
| April 11, 2013 | Transfer of the patient to the Department of Surgery of the collaborating oncology hospital |
| April 15 - 16, 2013 | Emergent esophagogastroduodenoscopy due to relapse of melena. Possible foci of hemorrhage from the major duodenal papilla (hemosuccus pancreaticus) |
| April 20, 2013 | Drainage of retroperitoneal cystic lesion |
| April 26, 2013 | Discharge from the Department of Surgery of the oncology hospital |
| May 17, 2013 | First clinical follow-up of the patient at the Endocrinology Department and Department of Surgery of the oncology hospital. Patient stable with no symptoms. |
| June 2013 | Second follow-up with abdominal magnetic resonance imaging (MRI), endocrine assessment and specific tumor markers |
| November 2013 | Follow-up with triple-phase abdominal CT |
| January 2014 | Follow-up with biochemical and specific tumor markers |
| June 2014 | Follow-up with specific tumor markers and abdominal CT |
| October 2014 | Octreotide scan negative for relapse of the disease or metastasis |
| 2015 - 2023 | Yearly follow-up with clinical, biochemical, endocrine and imaging reassessment of the patient. No signs of relapse of the disease or metastasis |
| At presentation | At seventh day | Normal range | |
|---|---|---|---|
| Hemoglobin (g/dL)/hematocrit (%) | 17.2/44.6 | 15.1/40.6 | (11.5 - 15.5 g/dL)/(37-47%) |
| Potassium (mEq/L) | 2.1 | 2.2 | 3.5 - 5.1 mEq/L |
| Calcium (mg/dL) | 11.1 | 12.2 | 8.5 - 10.5 mg/dL |
| Sodium (mEq/L) | 123 | 129 | 135 - 147 mEq/L |
| Chloride (mEq/L) | 89 | 100 | 96 - 108 mEq/L |
| Magnesium (mg/dL) | 2.6 | 2.4 | 1.8 - 2.4 mg/dL |
| Phosphorus (mg/dL) | 2.4 | 2.4 | 2.5 - 5 mg/dL |
| Glucose (mg/dL) | 159 | 108 | 70 - 110 mg/dL |
| Urea (mg/dL) | 221 | 50 | 12 - 42 mg/dL |
| Creatinine (mg/dL) | 4.2 | 0.7 | 0.6 - 1 mg/dL |
| Albumin (g/dL) | 4.7 | 3.3 | 3.5 - 5 g/dL |
| C-reactive protein (mg/dL) | 0.21 | 3.2 | < 0.5 mg/dL |
| pH of arterial blood sample | 7.25 | 7.31 | 7.35 - 7.45 |
| Potassium in 24-h urine sample (mmol/24 h) | - | 7.20 | 25 - 100 mmol/24 h |
| Infectious causes |
| Viruses: Rotavirus, Norovirus, Adenovirus, Cytomegalovirus |
| Bacteria: E. coli, Salmonella, Shigella dysenteriae, Campylobacter jejuni, Clostridium difficile, Yersinia, Vibrio cholerae |
| Parasites: Giardia intestinalis, Cryptosporidium parvum, Entamoeba histolytica |
| Non-infectious causes |
| Gastrointestinal causes: Inflammatory bowel disease, diverticulitis, ischemic colitis, short bowel syndrome, irritable bowel syndrome, etc. |
| Endocrinopathies: Hyperthyroidism, adrenal insufficiency, carcinoid tumors, etc. |
| Adverse effects of medications: Antibiotics, colchicine, antiarrhythmics, chemotherapeutic agents, etc. |
| Dietary causes: Food intolerance or food allergies |
| Malignancy: Colon cancer, intestinal lymphoma, etc. |
| Iatrogenic causes: Radiation therapy, gastrointestinal contrast agents, etc. |
| Blood marker | Laboratory values | Normal range |
|---|---|---|
| Carcinoembryonic antigen (ng/mL) | 0.97 | < 5.1 ng/mL |
| Calcitonin (pg/mL) | 759.2 | < 10 pg/mL |
| Chromogranin A (ng/mL) | 360.9 | 19.4 - 98.1 ng/mL |
| Neuron-specific enolase (ng/mL) | 0.47 | < 12.5 ng/mL |
| Intact parathormone (pg/mL) | 12 | 10 - 65 pg/mL |
| Thyroid-stimulating hormone (µIU/mL) | 1.28 | 0.30 - 4.0 µIU/mL |
| Free thyroxine (pg/mL) | 11.38 | 7.8 - 19.4 pg/mL |
| Adrenocorticotropic hormone (pg/mL) | 44.91 | 10 - 60 pg/mL |
| Morning cortisol (µg/dL) | 50.07 | 6.2 - 19.4 µg/dL |
| 24-h urine hydroxyindoleacetic acid (mg/24 h) | 9.6 | < 15 mg/24 h |
| Vasoactive intestinal peptide (pmol/L) | > 120 | < 30 pmol/L |