
Figure 1. Postoperative photograph of our patient showing the insertion site and tunneled trach with a purulent discharge that was noted on postoperative day 5.
| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 15, Number 1, January 2024, pages 7-14
Epidural Abscess Complicating Tunneled Caudal Epidural Catheter in an Infant for Postoperative Pain Management of Open Abdominal Surgery
Figures

Tables
| MRI: magnetic resonance imaging; POD: postoperative day. | |
| POD 0 | Epidural catheter placed for postoperative analgesia. |
| POD 4 | The epidural catheter was removed as it was no longer required for clinical care. |
| POD 5 | The tunneled insertion of the epidural catheter was noted to be erythematous with a purulent discharge. The patient had a new onset of fever to 38.2 °C. MRI was ordered and a beside ultrasound of the sacrum and spine was obtained. |
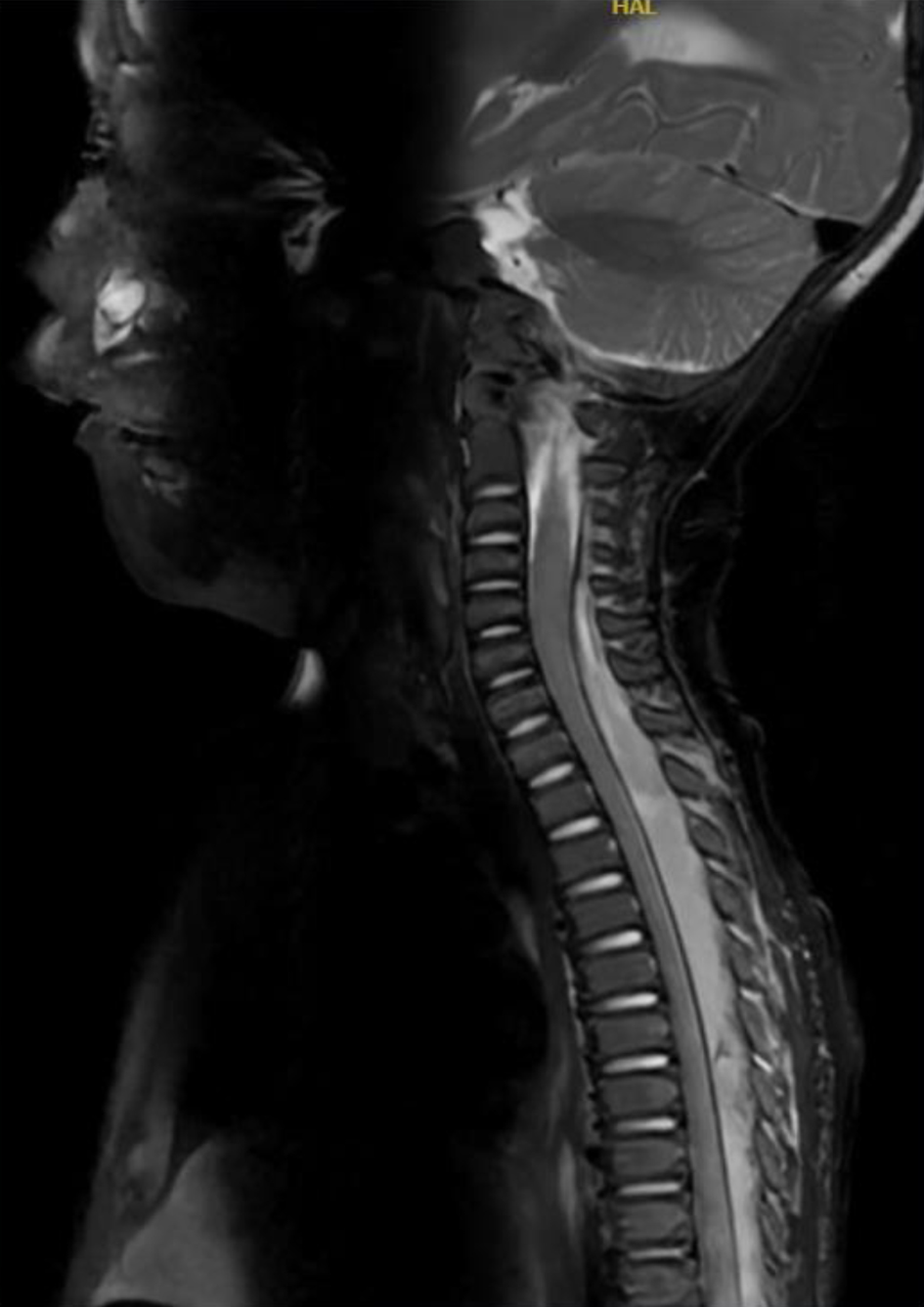
| POD 10 | Repeat MRI of the spine demonstrated persistence of a complex epidural fluid collection from C5 to the sacrum, which was concerning for an infectious process or abscess. The patient was taken to the operating room where a left T5-T6 hemilaminectomy was performed with evacuation of an epidural abscess and hematoma. |
| POD 53 | The patient was discharged home after completion of a 6-week course of intravenous antibiotics. |
| Author and reference | Study cohort | Clinical findings and outcome |
|---|---|---|
| PRAN: Pediatric Regional Anesthesia Network; CRPS I: complex regional pain syndrome type I; POD: postoperative day; CT: computed tomography; MRI: magnetic resonance imaging. | ||
| Polaner et al [5] | Prospective, multi-center reporting of regional anesthesia outcomes known as the PRAN. A cohort of 14,917 pediatric patients. | Total of 2,946 neuraxial catheters with 32 (1% incidence) local infections or inflammatory changes noted. Higher incidence in caudal versus lumbar epidural catheters. The majority were localized to the insertion site and treated by removal of the catheter. Antibiotics were prescribed for three patients. All cases resolved without complications. No cases of deep infection, abscess, or meningitis. Eight caudal catheters were removed because the dressings were soiled with fecal matter and 10 were removed because of fever without an identified source. |
| Walker et al [7] | Prospective, observational study from the PRAN database. A total of 91,701 pediatric patients and more than 100,000 regional blocks. | The incidence of cutaneous or localized infections was 0.5% (n = 92). One epidural abscess was reported in a 2-month-old infant who had a lumbar epidural catheter that was removed on postoperative day 4. Purulent drainage from the insertion site was noted the day following removal. A lumbar laminectomy with abscess drainage was performed and the child recovered uneventfully with no neurological deficit. |
| Pula et al [17] | Prospective study of 200 patients, 0 - 18 years of age (154 males, 46 females). | Incidence of 0.5% (1 in 200) for infectious complications. Localized infection in one patient who had an epidural catheter in for more than 3 days. Culture and sensitivity identified methicillin-sensitive Staphylococcus aureus. No neurological deficits were noted. |
| Pietropaoli et al [18] | Prospective study of 174 children, from 1 day to 17 years old (105 males, 69 females). | One epidural abscess was reported in a 13-year-old girl admitted in acute progressive respiratory distress. She was empirically started on methylprednisolone. A thoracic epidural catheter was inserted for postoperative pain control and remained in place for 3 days. She did not receive any preoperative antibiotics for her procedure. She was discharged home on POD 7. She returned 2 days later with severe back pain secondary to a coagulase-positive Staphylococcus aureus epidural abscess. This was drained and the patient recovered uneventfully. |
| Meunier et al [19] | 10 and 7-week-old male infants, 5.4 and 4 kg, respectively. | Kasai procedure for biliary atresia. Lumbar epidural catheter in both patients via the fifth lumbar interspace. The epidural catheters were removed on POD 2-3. On POD 5, an erythematous, indurated region with a pustule was noted at the catheter entry site. Treatment consisted of manual evacuation of purulent material. For the first infant, no organism was cultured from the wound site exudate. No antibiotics were administered. Recovery was complete in a few days. For the second infant, culture was positive for Staphylococcus aureus, which was treated with a 10-day course of antibiotics. Recovery was complete in both patients. |
| Larsson et al [20] | One-year-old infant. | Multiple epidural catheters to treat severe visceral abdominal pain. Tender swelling was detected at the entry site of the third epidural catheter (L1-2), 12 days after placement. The catheter was immediately removed. CT and MRI confirmed the presence of an epidural abscess from T5 to L5 without neurological symptoms. Antibiotic therapy was initiated, and the culture grew Pseudomonas aeruginosa. Treated with antibiotics and no neurosurgical intervention. |
| Ingelmo et al [21] | 13-year-old adolescent male. | On the fifth post-insertion day of a lumbar epidural catheter for CRPS I, the patient complained of back pain. Insertion site revealed erythema, swelling and tenderness. Epidural catheter was removed. On physical examination, there was purulent discharge from the insertion site. CT revealed subcutaneous fluid. Antibiotics were started and surgical drainage performed. Cultures were positive for Staphylococcus aureus. Recovery was complete after 15 days of antibiotic therapy. |
| Emmanuel et al [22] | A 4-year-old boy, 15.6 kg. | Caudal epidural catheter for perioperative analgesia. The catheter was removed 29 h after the operation. Ten days after the operation, a skin pustule was noted at the catheter insertion site. The site of the pustule and catheter tract were explored. No growth occurred from the specimen. Antibiotics for 12 days after drainage. No neurological deficits. |
| Llewellyn et al [23] | Prospective audit of 10,633 epidural catheters, newborn to 18 years of age. | Twenty-five cases of local skin infection, one patient with meningeal signs, and two epidural abscesses. The surgical procedure for both patients with epidural abscess was Nissen fundoplication. The first patient was 4.1 kg, 7 months old, who developed an epidural abscess 22 h after a lumbar epidural catheter. Although there was no documentation to suggest that the child was febrile, the child was irritable and reluctant to lie supine. The infective organism was Staphylococcus aureus. The child returned to the country of origin and has had no further follow-up in the United Kingdom. The second patient was a 21 kg, 6-year-old child who developed an entry-site skin infection 115 h after a thoracic epidural catheter. The child was afebrile at the time of catheter removal; however, the insertion site was erythematous. Methicillin-resistant Staphylococcus aureus was cultured from the insertion site and the child was treated with intravenous antibiotics for 3 days. Ultrasound of the epidural space was negative, and the child was discharged home on oral antibiotics. The child was readmitted 5 days later, febrile and complaining of back pain but with no neurological signs. MRI demonstrated an epidural abscess from T2 to L3. The child was treated with antibiotics for 4 weeks until full resolution. |
| Aram et al [24] | Retrospective study of 25 patients, 1 day to 36 years of age. | Two cases of possible infections. The first patient had a fever on POD 8, during which all indwelling catheters including an epidural catheter were removed. A second patient developed catheter exit site’s cellulitis and complained of both tenderness and erythema on POD 4. Empirical antibiotic (cephalexin) was prescribed until culture’s result became negative. Epidural catheters remained in place for a median of 11 days. |
| Sethna et al [25] | Observation study of 7,792 children, newborn to 18 years of age. | A cohort of 10,653 epidural catheters. Thirteen (0.12%) infectious complications including nine cellulitis, two paravertebral muscle infections, one epidural inflammation, and one epidural abscess. The incidence was higher in patients treated for chronic pain (3.2%) compared with postoperative pain (0.06%). Surgical drainage of subcutaneous abscess was performed in three patients, and medical therapy was administered in the remainder of patients. All patients recovered without sequelae. The epidural abscess was reported in a 12-year-old child, who presented with back pain without local cellulitis, 4 days after catheter removal. An initial MRI of the thoracic and lumbar spine revealed only deep paraspinal muscle inflammation. Antibiotic therapy was initiated, and the patient was discharged home. Two days later, the child was readmitted for worsening back pain, pyrexia, and difficult ambulation. A repeat MRI demonstrated an epidural abscess. The patient was treated with antibiotics for 4 weeks. |