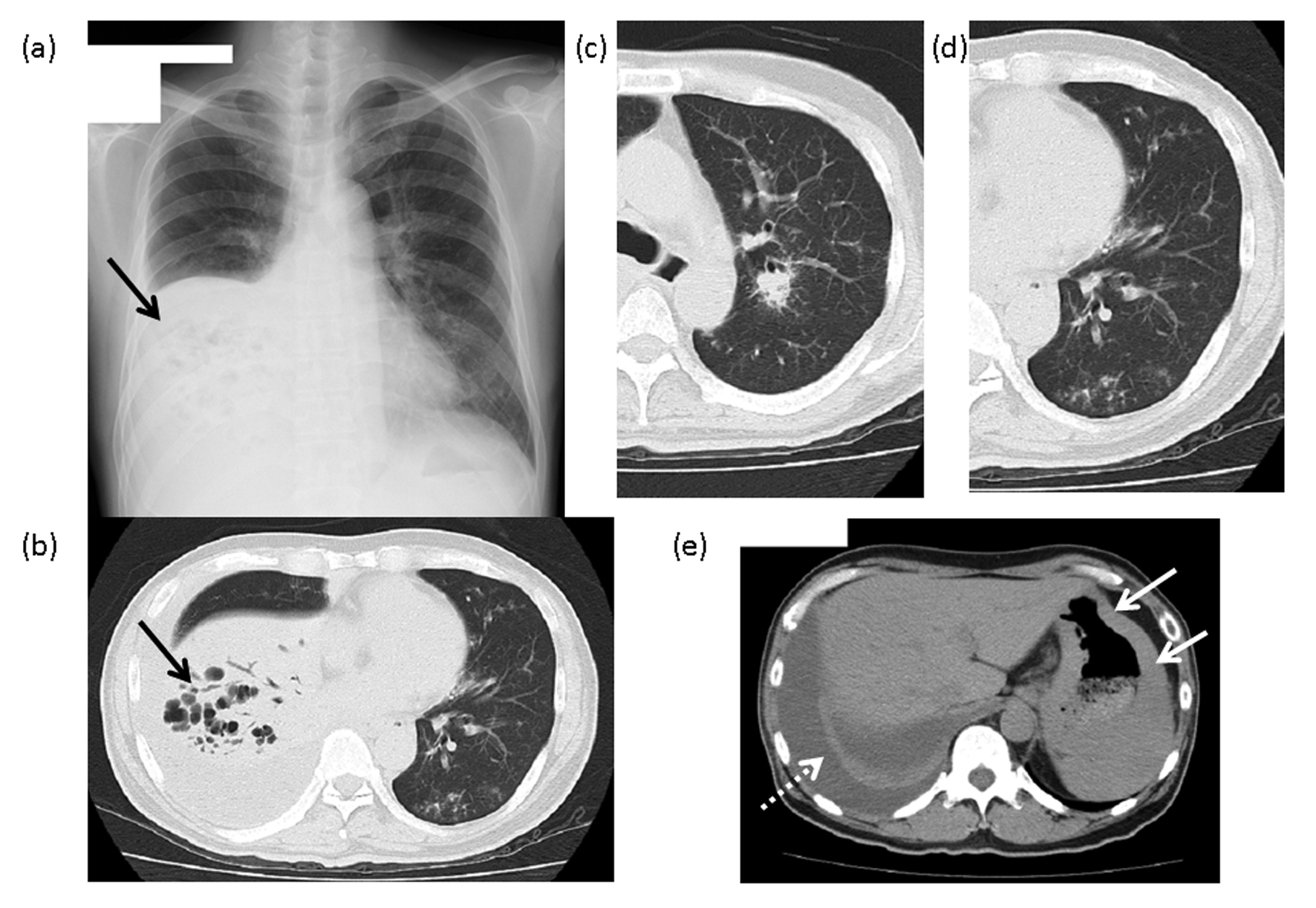
Figure 1. The findings of chest X-ray and computed tomography (CT). (a) Chest X-ray: An area of reduced permeability, with multiple cysts, is visible in the lower right lobe (arrow). (b) Chest CT: An infiltrative shadow with manifest bronchiectasis can be seen in the right lower lobe (arrow). (c) A nodular lesion with an air bronchogram is visible around the center side of the bronchus of the right upper lobe. (d) Multiple ground-glass opacities and granular lesions are visible around the bronchus on the periphery of the left lower lobe. (e) A right pleural effusion (dashed line arrow) and the gastric wall with manifest thickening (arrow) can be seen on this image.