| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 8, August 2023, pages 293-298
A Case of Radiation-Associated Vertebral Compression Fracture Mimicking Solitary Bone Metastasis of Lung Cancer
Shoko Ikutaa, b, Nao Shoshiharaa, Seigo Minamia, c, g, Hironao Yasuokad, Keiko Takaharae, f, Yoshiaki Okamotoe
aDepartment of Respiratory Medicine, Osaka Police Hospital, Tennoji-ku, Osaka 543-0035, Japan
bDepartment of Respiratory Medicine and Clinical Immunology, Graduate School of Medicine, Osaka University, Suita 565-0871, Japan
cDepartment of Respiratory Medicine, National Hospital Organization, Osaka Medical Center, Chuo-Ku, Osaka City, Osaka 540-0006, Japan
dDiagnostic Pathology, Osaka Police Hospital, Tennoji-ku, Osaka 543-0035, Japan
eRadiation Oncology, Osaka Police Hospital, Tennoji-ku, Osaka 543-0035, Japan
fDepartment of Radiation Oncology, Osaka Breast Center, Fukushima-ku, Osaka City, Osaka 553-0007, Japan
gCorresponding Author: Seigo Minami, Department of Respiratory Medicine, National Hospital Organization, Osaka Medical Center, Chuo-Ku, Osaka City, Osaka 540-0006, Japan
Manuscript submitted June 16, 2023, accepted August 19, 2023, published online August 28, 2023
Short title: Radiation-Associated Vertebral Fracture
doi: https://doi.org/10.14740/jmc4133
| Abstract | ▴Top |
Radiation therapy plays an important role in the treatment of lung cancer. Although adverse effects of radiation are well known, they are sometimes difficult to be diagnosed. We report a case of a radiation-associated vertebral compression fracture which mimicked bone metastasis of lung cancer. The patient was a 57-year-old man diagnosed with lung squamous cell carcinoma (cT1aN2M0, c-stage IIIA). He received concurrent chemoradiotherapy (CRT) in combination with 6 weeks of weekly carboplatin plus paclitaxel and thoracic radiation of 60 Gy/30 fractions, followed by bi-weekly durvalumab for 12 months. On the last day of the 12-month durvalumab regimen, he complained of backache. Magnetic resonance imaging showed compression fracture of the seventh thoracic vertebra with the spinal cord compressed, and fluorine-18 fluorodeoxyglucose positron emission tomography and computed tomography demonstrated weak focal uptake only at the seventh thoracic vertebra. Although the fracture had been suspected to be bone metastasis, surgical biopsy revealed no evidence of malignancy. Since the seventh thoracic vertebra was included in the irradiation area, the patient was diagnosed with a radiation-associated fracture. Dual-energy X-ray absorptiometry of the lumbar vertebrae (L2 - 4) after the surgery revealed osteopenia. In conclusion, we successfully diagnosed the radiation-associated vertebral fracture caused by radical CRT. The fracture mimicked bone metastasis in preoperative imaging tests. Thus, surgical biopsy was useful for diagnosis.
Keywords: Radiation-associated fracture; Vertebral compression fracture; Radiation adverse effects; Locally advanced non-small cell lung cancer; Chemoradiotherapy; Immune-checkpoint inhibitor; Durvalumab consolidation; Bone metastasis
| Introduction | ▴Top |
Radiation therapy plays an important role in the treatment of lung cancer. It is used for a variety of purposes, including radical chemoradiotherapy (CRT), stereotactic body radiation therapy (SBRT), palliative irradiation, and control of brain metastases. Especially after the launch of durvalumab, an anti-programmed cell death protein 1 ligand (PD-L1) antibody, the importance of radical CRT in the treatment of unresectable stage III non-small-cell lung cancer (NSCLC) has been increasing. Consolidation durvalumab provided a survival rate of 66.3% at 24 months for patients with unresectable stage III NSCLC who have not progressed after CRT, compared with 50% for placebo [1, 2]. Late-onset adverse effects of radiation therapy may occur more frequently, as lung cancer patients survive longer. However, it is often difficult to distinguish adverse events from cancer progression when clinicians encounter unexpected events in cancer patients.
Herein, we describe a patient with stage III NSCLC who had been diagnosed with vertebral compression fracture associated with radical CRT by a surgical biopsy.
| Case Report | ▴Top |
Investigations
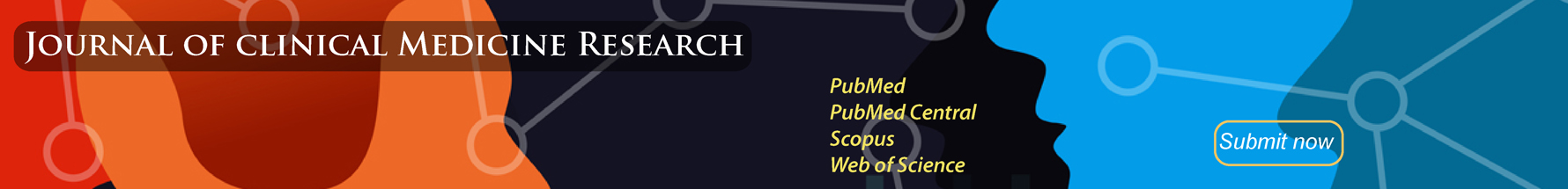
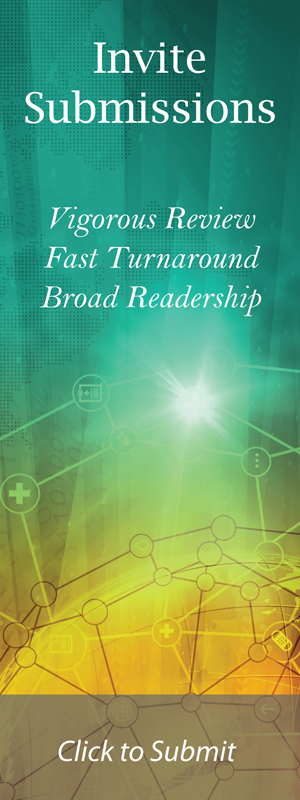
A 57-year-old Japanese man was referred to our department because of a tumor shadow in the right middle lung field on chest computed tomography (CT) scan (Fig. 1a). He had been regularly followed by chest CT because his pro-gastrin-releasing peptide (pro-GRP) had been above 90 pg/mL on his medical check-up and subsequent follow-up examinations for more than 3 years. He had no significant past medical history. He was an ex-smoker with smoking history of 2.5 packs of cigarettes per day for 35 years and drank two glasses of sake five times a week. His body mass index (BMI) was 21.5 kg/m2. He was diagnosed with lung squamous cell carcinoma by a bronchoscopic biopsy from a visible tumor in the right B4 (Figs. 1b, 2) and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) from the subcarinal lymph node. The tumor proportion score (TPS) of PD-L1 was 5-10% (22C3 pharmDx assay). Fluorine-18 fluorodeoxyglucose positron emission tomography (FDG-PET) and CT revealed mediastinal lymph node metastases with the maximum standardized uptake value (SUVmax) of 3.23 (Fig. 1c). However, FDG-PET/CT did not detect the primary tumor of the right middle lobe. The cancer was classified as c-stage IIIA, c-T1aN2M0, in the eighth edition staging system of Union for International Cancer Control (UICC)-TNM classification.
 Click for large image | Figure 1. Chest computed tomography (a), a bronchoscopic image of the right B4 (b) and fluorine-18 fluorodeoxyglucose positron emission tomography and computed tomography (c). Yellow arrowhead points to the primary lung cancer (a, b) and yellow arrows point to lymph node metastases (c). |
 Click for large image | Figure 2. Histology of bronchoscopial specimen from the tumor in the right B4 (H&E stain). H&E: hematoxylin and eosin. |
He received concurrent CRT. This treatment regimen included 6 weeks of weekly carboplatin (area under the plasma concentration time curve of 2 mg/mL/min) plus paclitaxel (40 mg/m2) with 22.6 mg of dexamethasone every week in combination of thoracic irradiation of 60 Gy/30 fractions to the lung and the mediastinum. Although the radiation was performed by intensity-modulated radiation therapy (IMRT), the irradiation area included the thoracic vertebrae (Fig. 3). After CRT, he received bi-weekly durvalumab (10 mg/kg) for 12 months. On the last day of the 12-month durvalumab consolidation, he complained of backache for several days. Contrast-enhanced CT scan revealed that the cancer was completely responded to the treatment and did not detect any additional abnormalities. Moreover, tumor markers such as squamous cell carcinoma antigen (SCC) and CYFRA 21-1 remained within the normal range. SCC and CYFRA 21-1 were 1.1 ng/mL and 5.1 ng/mL before the start of CRT, and then 0.8 ng/mL and 2.8 ng/mL when the fracture occurred, respectively. However, magnetic resonance imaging (MRI) showed a compression fracture of the seventh thoracic vertebra with the spinal cord compressed by growing soft tissue surrounding the fracture (Fig. 4a). Physical examination revealed increased tendon reflexes in the bilateral legs. Furthermore, FDG-PET/CT demonstrated weak but focal uptake only at the seventh thoracic vertebra with SUVmax of 1.55 (Fig. 4b).
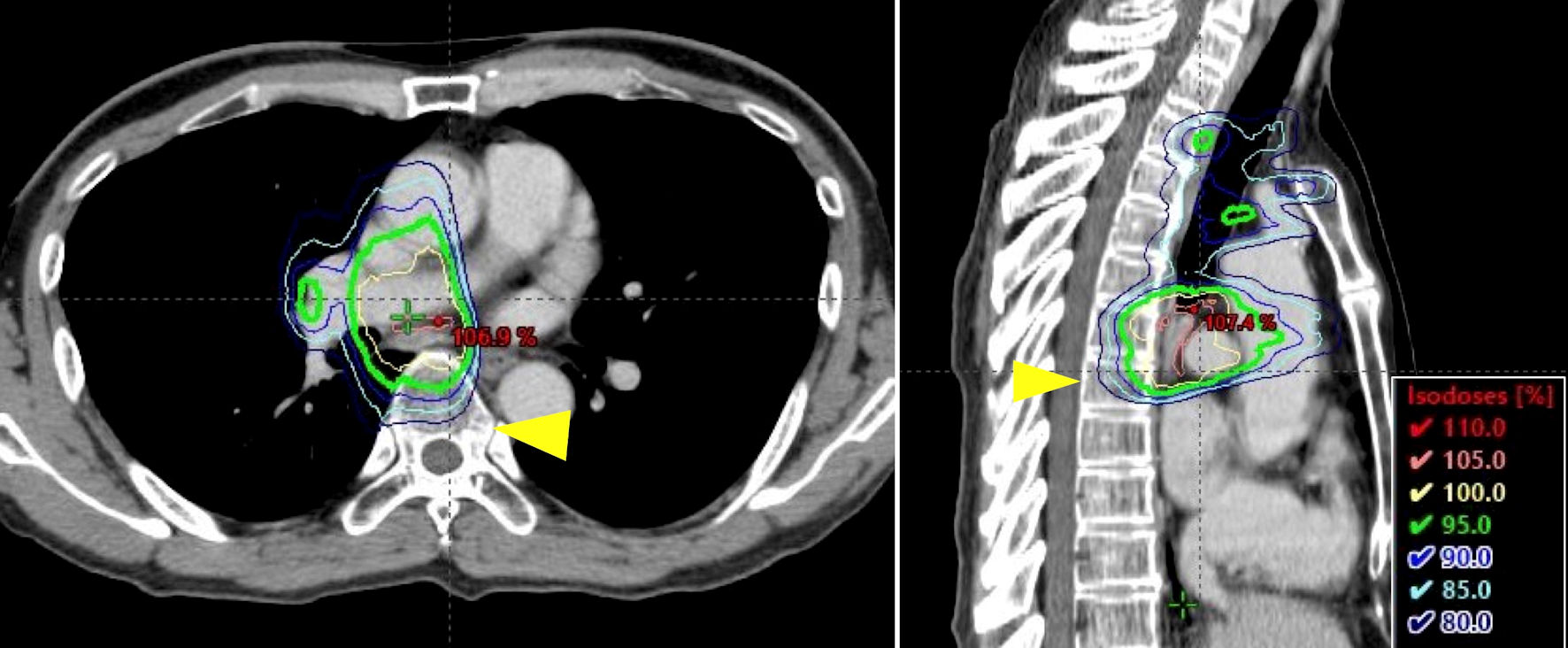 Click for large image | Figure 3. Radiation dose distribution and planning design images of chest computed tomography before chemoradiotherapy. Yellow arrowheads point to the seventh thoracic vertebra. The lines represent the irradiation area. |
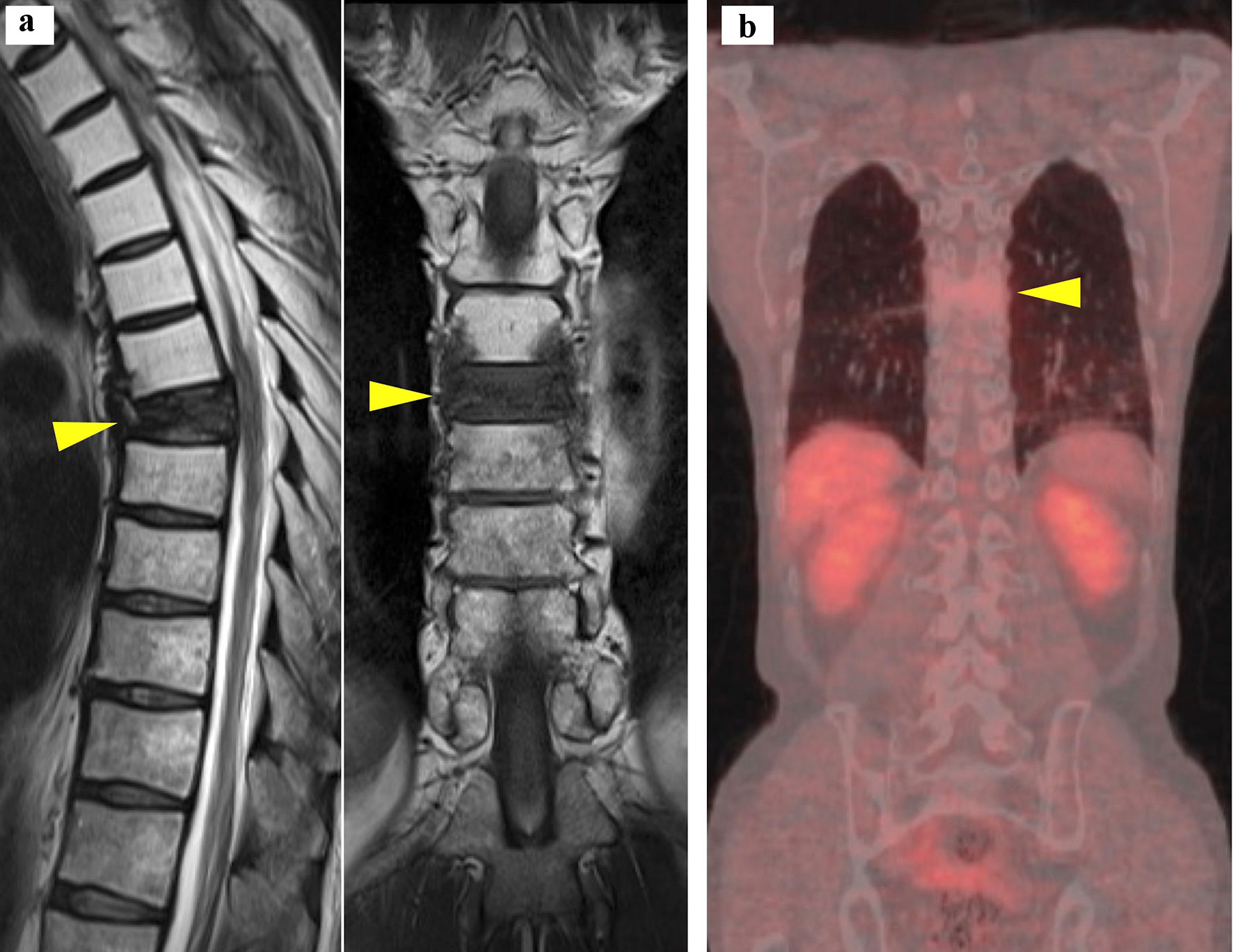 Click for large image | Figure 4. Sagittal (left) and coronal (right) views of magnetic resonance imaging of the spine (a), and coronal view of fused imaging of fluorine-18 fluorodeoxyglucose positron emission tomography and computed tomography (b). Yellow arrowheads point to the fractured seventh thoracic vertebra. |
Diagnosis
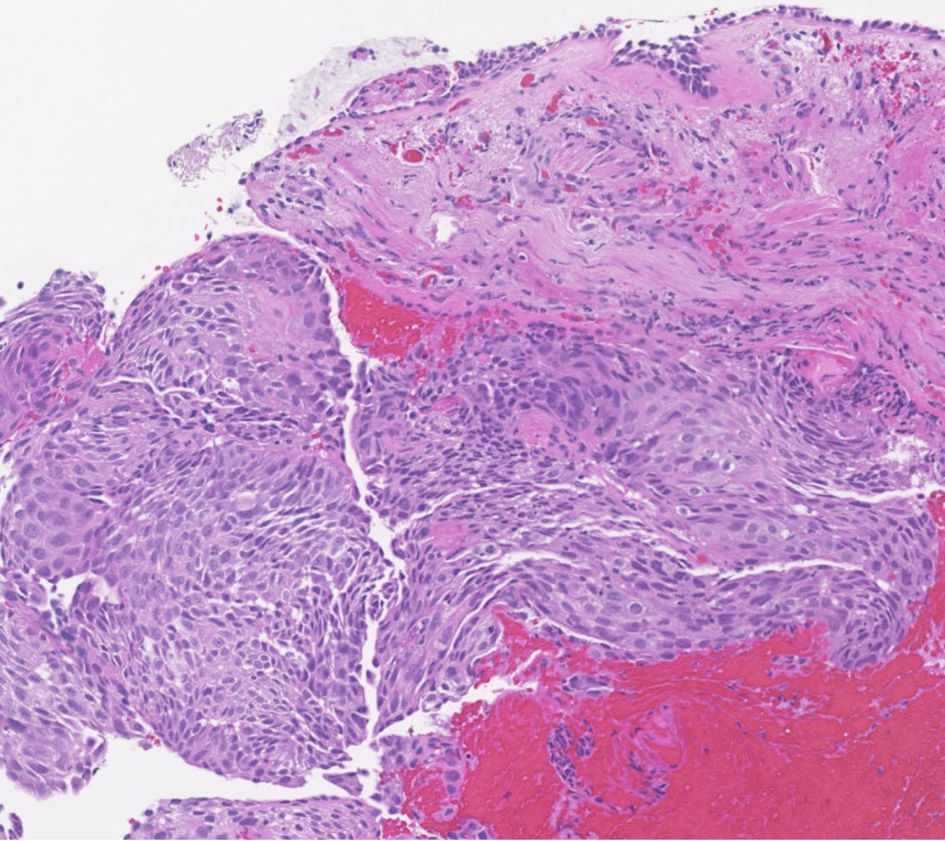
Considering that the patient was still young and had no history of osteoporosis or fractures, these findings suggested a thoracic vertebral metastasis of lung cancer. Because the growing tissue at the fracture was compressing the spinal cord and causing abnormal tendon reflex, we selected spinal decompression surgery instead of SBRT to the vertebra. Pedicle screw fixation, laminectomy, resection of the intraspinal tumor and vertebral biopsy were performed by orthopedic surgeons. During the surgery, thickened yellow ligaments and proliferated fatty tissue were observed to compress the dura mater. The surgical biopsy revealed that the proliferated tissue in the spinal canal consisted of fatty tissue and fibrotic tissue with partial vascularization, and that the seventh thoracic vertebral bone contained granulation tissue, fibrosis and lamellar bone fragmentation with osteoblast proliferation. Unexpectedly, the surgical specimen contained neither malignant cells nor abnormal active inflammation such as excessive infiltration of lymphocytes (Fig. 5). These histopathological findings demonstrated that the fracture was caused not by cancer relapse or immune-mediated adverse events (imAEs), but by a simple bone fragility. The seventh thoracic vertebra was partially included in the irradiation field (Fig. 3). The percentage of the seventh thoracic vertebral volume irradiated 20 Gy (V20) and V30 were 98.8% and 87.1%, respectively. Bone fragmentation and fibrosis suggested radiation-associated changes. Therefore, the fracture was diagnosed as a radiation-associated complication.
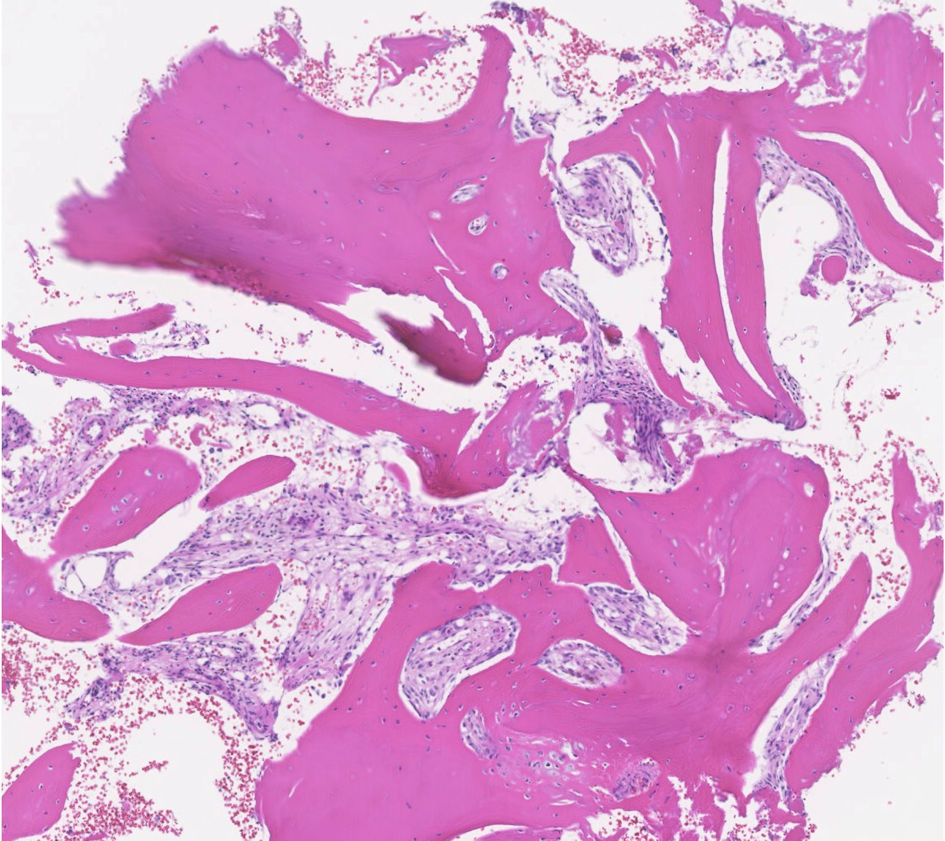 Click for large image | Figure 5. Histology of the seventh thoracic vertebral specimen (H&E stain). H&E: hematoxylin and eosin. |
Treatment
The fracture site was surgically controlled. After the surgery, dual-energy X-ray absorptiometry (DXA) of the lumbar vertebrae (L2 - 4) revealed osteopenia with 74% of young adult mean (YAM), and DXA of the femur showed 83% of YAM. His biochemical evaluation revealed vitamin D deficiency (25-OH-vitamin D 8.8 ng/mL, 1,25-OH vitamin D3 55.7 pg/mL) and elevated bone resorption markers (N-telopeptide of type 1 collagen (NTx) 28.3 nmol bone collagen equivalents (BCE)/nmol, urinary NTx 61.9 nmol BCE/nmol Cre). Neither endocrine abnormalities (albumin-adjusted calcium 9.2 mg/dL, parathyroid hormone (PTH) 64 pg/mL, PTH-related protein (PTHrP) undetectable) nor alkaline phosphatase (ALP) abnormalities (ALP 96 U/L, bone ALP (BAP) 18.4 µg/L) were observed. Daily subcutaneous injection of abaloparatide acetate was initiated by the orthopedic surgeon.
Follow-up and outcomes
The lung cancer was controlled by the CRT and durvalumab, and he was alive without relapse 3 months after the surgery.
| Discussion | ▴Top |
Radiation-associated fracture is a well-known adverse event of radiation therapy. Rib fractures due to SBRT for early-stage NSCLC are common in lung cancer treatment [3]. On the contrary, fractures due to radical CRT for unresectable stage III lung cancer are rare and poorly documented. To our knowledge, this is the first report of a vertebral compression fracture associated with radical CRT followed by durvalumab consolidation for locally advanced lung cancer.
First, in our case, the radiation-associated vertebral fragility fracture mimicked a solitary bone metastasis. Bone is one of the most frequently observed metastatic sites of lung cancer [4]. Although imaging tests are effective to reveal the cause of a fracture, neither MRI nor FDG-PET/CT always differentiate between bone metastases and post-radiation adverse effects [5]. Posterior cortical bulging, epidural mass formation and pedicle enhancement with gadolinium-enhanced MRI were more frequently seen in vertebral compression fractures caused by malignancy than in benign fractures. SUVmax of FDG-PET/CT were significantly higher in malignancy with the most reliable threshold for SUVmax of 4.25. However, these MRI findings and FDG-PET/CT uptake were often seen in benign fractures: the three MRI findings aligned in 17% of benign cases (64% in malignancy), and FDG-PET/CT uptake was seen in 71% of benign cases (100% in malignancy) [6]. Taken together, these imaging tests are useful but also have limitations. In our case, MRI and FDG-PET/CT could not deny bone metastasis because MRI showed that the vertebral fracture site was surrounded by abnormal tissue compressing the dura mater, and FDG-PET/CT revealed that the fracture had weak but focal FDG uptake. Clinicians should not hesitate invasive specimen collection, with the limitations of imaging tests in mind.
Second, thoracic irradiation caused a vertebral compression fracture. Although some studies have shown risk of fractures due to SBRT [3, 7], there have been few reports about radiation-associated fractures due to radical CRT. The frequency of rib fractures was 5.27% after SBRT for early-stage NSCLC, and high chest wall V30 was an important predictor [3]. As for spine SBRT, dose per fraction of 20 Gy or greater was a significant predictor of vertebral fractures [7]. However, those parameters of SBRT do not apply to radical CRT, because biological effects of radiation depend not only on dose but also on fractions. In general, the biological effects of the same radiation dose are enhanced when the fractions are smaller [8]. The rarity of fractures after radical CRT might be explained by the lower per-dose and higher fraction of radiation than SBRT. A single radiation dose of SBRT for early-stage NSCLC is high, for example, 48 Gy/4 fractions or 54 Gy/3 fractions [9, 10], whereas that of radical CRT for unresectable stage III NSCLC is low, for example, 60 Gy/30 fractions [11]. Radiation to bone reduces bone density by disruption of a vascular supply, osteoblasts reduction and activation of osteoclasts. Trabecular bone turnover is greater than cortical bone turnover, and thus vertebrae, which contain a high ratio of trabecular bone, are sensitive to radiation. Typically, insufficiency fractures occur after a period of radiation, when physical stress is applied to a weakened bone. Thus, insufficiency fractures can occur months or years later after radiation therapy [12]. When a patient who has previously received radiotherapy develops a fracture, clinicians should check the past irradiation field. Furthermore, as for CRT, prophylactic steroids used in combination with chemotherapy might be a risk factor for osteoporosis. Smoking, advanced age, excessive alcohol consumption and low BMI are also risk factors for osteoporosis [13]. These predispositions are often observed in lung cancer patients. In addition, high prevalence of vitamin D deficiency, an important risk of osteoporosis, has been reported in lung cancer patients [14]. Therefore, clinicians should be careful of an underlying risk of fractures, even if patients do not have past history of osteoporosis before radiation therapy. In our speculation, radiation therapy was the main cause of the fracture in our patient who had been prone to osteopenia by his smoking history, drinking habits, steroids and vitamin D deficiency.
Third, in this case, the vertebral biopsy did not detect any active inflammation which indicated imAEs due to durvalumab. A few reports suggested that immune checkpoint inhibitors (ICIs) might cause inflammatory toxicities on bone or bone turnover abnormalities [15, 16]. However, none of these reports proved bone toxicities due to ICIs pathophysiologically. Although it is still unclear whether ICIs induce the imAE of osteoporosis, our case did not pathologically detect any trace of imAEs after durvalumab.
In conclusion, we successfully diagnosed the radiation-associated vertebral fracture caused by radical CRT for NSCLC. Since the fracture mimicked bone metastasis in imaging tests, surgical biopsy was useful for diagnosis.
Learning points
The main take-away point is that radiation-associated fractures are difficult to diagnose because adequate imaging tests, including MRI and FDG-PET/CT, do not always distinguish them from bone metastases. Therefore, clinicians should consider specimen collection and histological analysis. It is also important to note that although radical CRT for lung cancer has lower radiation dose per fraction than SBRT, it may cause a vertebral fracture. Since lung cancer patients often have risks of osteoporosis, clinicians should pay attention to fractures after radiation therapy and check the previous irradiation field when a patient complains of pain.
Acknowledgments
The authors are grateful to Kazuya Ohshima for his surgery, and to Shoichi Ihara and Kanako Nishimatsu for their treatment.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
The patient has given written informed consent for publication of this case report, including the accompanying images.
Author Contributions
S. Ikuta was involved in chemoradiotherapy, immunotherapy and outpatient follow-up. S. Minami and N. Shoshihara were involved in outpatient follow-up. H. Yasuoka made pathological diagnosis. K. Takahara and Y. Okamoto performed radiotherapy. All authors critically revised the report and approved the final version.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, Yokoi T, et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med. 2017;377(20):1919-1929.
doi pubmed - Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, Kurata T, et al. Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N Engl J Med. 2018;379(24):2342-2350.
doi pubmed - Voruganti IS, Donovan E, Walker-Dilks C, Swaminath A. Chest wall toxicity after stereotactic radiation in early lung cancer: a systematic review. Curr Oncol. 2020;27(4):179-189.
doi pubmed pmc - Riihimaki M, Hemminki A, Fallah M, Thomsen H, Sundquist K, Sundquist J, Hemminki K. Metastatic sites and survival in lung cancer. Lung Cancer. 2014;86(1):78-84.
doi pubmed - Al-Omair A, Smith R, Kiehl TR, Lao L, Yu E, Massicotte EM, Keith J, et al. Radiation-induced vertebral compression fracture following spine stereotactic radiosurgery: clinicopathological correlation. J Neurosurg Spine. 2013;18(5):430-435.
doi pubmed - Cho WI, Chang UK. Comparison of MR imaging and FDG-PET/CT in the differential diagnosis of benign and malignant vertebral compression fractures. J Neurosurg Spine. 2011;14(2):177-183.
doi pubmed - Cunha MV, Al-Omair A, Atenafu EG, Masucci GL, Letourneau D, Korol R, Yu E, et al. Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT): analysis of predictive factors. Int J Radiat Oncol Biol Phys. 2012;84(3):e343-349.
doi pubmed - Brenner DJ. The linear-quadratic model is an appropriate methodology for determining isoeffective doses at large doses per fraction. Semin Radiat Oncol. 2008;18(4):234-239.
doi pubmed pmc - Nagata Y, Hiraoka M, Shibata T, Onishi H, Kokubo M, Karasawa K, Shioyama Y, et al. Prospective trial of stereotactic body radiation therapy for both operable and inoperable T1N0M0 non-small cell lung cancer: Japan Clinical Oncology Group Study JCOG0403. Int J Radiat Oncol Biol Phys. 2015;93(5):989-996.
doi pubmed - Ball D, Mai GT, Vinod S, Babington S, Ruben J, Kron T, Chesson B, et al. Stereotactic ablative radiotherapy versus standard radiotherapy in stage 1 non-small-cell lung cancer (TROG 09.02 CHISEL): a phase 3, open-label, randomised controlled trial. Lancet Oncol. 2019;20(4):494-503.
doi pubmed - Yamamoto N, Nakagawa K, Nishimura Y, Tsujino K, Satouchi M, Kudo S, Hida T, et al. Phase III study comparing second- and third-generation regimens with concurrent thoracic radiotherapy in patients with unresectable stage III non-small-cell lung cancer: West Japan Thoracic Oncology Group WJTOG0105. J Clin Oncol. 2010;28(23):3739-3745.
doi pubmed - Pacheco R, Stock H. Effects of radiation on bone. Curr Osteoporos Rep. 2013;11(4):299-304.
doi pubmed - Kanis JA. Diagnosis of osteoporosis and assessment of fracture risk. Lancet. 2002;359(9321):1929-1936.
doi pubmed - Aguirre M, Manzano N, Salas Y, Angel M, Diaz-Couselo FA, Zylberman M. Vitamin D deficiency in patients admitted to the general ward with breast, lung, and colorectal cancer in Buenos Aires, Argentina. Arch Osteoporos. 2016;11:4.
doi pubmed - Moseley KF, Naidoo J, Bingham CO, Carducci MA, Forde PM, Gibney GT, Lipson EJ, et al. Immune-related adverse events with immune checkpoint inhibitors affecting the skeleton: a seminal case series. J Immunother Cancer. 2018;6(1):104.
doi pubmed pmc - Pantano F, Tramontana F, Iuliani M, Leanza G, Simonetti S, Piccoli A, Paviglianiti A, et al. Changes in bone turnover markers in patients without bone metastases receiving immune checkpoint inhibitors: An exploratory analysis. J Bone Oncol. 2022;37:100459.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.