| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 14, Number 12, December 2023, pages 393-399
Anesthetic Care During Exploratory Laparotomy and Excision of a Fetus-in-Fetu With a Combined General-Regional Anesthetic Technique Using a Caudal Epidural Catheter
Amr Elhamrawya, c, Ahsan Syeda, b, Joseph D. Tobiasa, b
aDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
bDepartment of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
cCorresponding Author: Amr Elhamrawy, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 43205, USA
Manuscript submitted October 19, 2023, accepted November 20, 2023, published online November 28, 2023
Short title: Caudal Epidural Catheter in a Case of Fetus-in-Fetu
doi: https://doi.org/10.14740/jmc4164
| Abstract | ▴Top |
Fetus-in-fetu (FIF) is a rare, congenital anomaly involving the presence of one of a pair of twins within the body of the other. It is postulated that this pathology occurs during embryogenesis of a diamniotic-monochorionic twin pregnancy with unequal division of the blastocele, which results in monozygotic, monochorionic, and diamniotic twins of unequal sizes. Presentation as an abdominal mass during the neonatal period or infancy is most common, although late diagnosis during the adult years may also occur. We report a 1-day-old, full-term female neonate who presented for exploratory laparotomy and excision of a FIF. We present the use of a combined general-regional technique using caudal epidural anesthesia. The etiology, presentation, appropriate workup, and treatment of FIF are presented. Previous anecdotal reports of anesthetic care for excision of FIF are reviewed.
Keywords: Fetus-in-fetu; Congenital anomaly; Pediatric anesthesiology; Teratoma; Caudal epidural anesthesia
| Introduction | ▴Top |
Fetus-in-fetu (FIF) is a rare, congenital anomaly involving the presence of one of a pair of twins within the body of the other. The most common location involves the retroperitoneal area, although reports have included its presence in the sacrum, head, scrotum, and the oropharynx. Its incidence is estimated at 1 in 500,000 births with a male predominance. German anatomist Johann Friedrich Meckel was the first to describe FIF during the late 18th century [1]. There are two possible theories to explain the rare anatomic presentation of the pathophysiology of FIF including the parasitic twin or the highly differentiated teratoma theory. The twinning theory states that there is an abnormality in embryogenesis of a diamniotic-monochorionic twin pregnancy with unequal division of the blastocele, which results in monozygotic, monochorionic, and diamniotic twins of unequal sizes. Alternatively, it has been suggested that pathology is an example of a teratoma that is highly organized and differentiated. Although the majority of cases present during infancy, late presentation during the fourth or fifth decade of life has also been reported [2, 3].
We report a 1-day-old neonate who required anesthetic care during a FIF procedure which was discovered during a routine prenatal ultrasound. Potential etiologies for this rare congenital anomaly are presented, appropriate workup discussed, and previous anecdotal reports of anesthetic and surgery care reviewed.
| Case Report | ▴Top |
Investigations
Review of this case and presentation in this format followed the guidelines of the Institutional Review Board at Nationwide Children’s Hospital (Columbus, OH). A 1-day-old full-term female neonate presented for exploratory laparotomy and excision of a FIF, which had been diagnosed at 33 weeks of gestation. On physical examination, the patient was a 3,035-g term infant in no acute distress. Preoperative vital signs revealed temperature 37 °C (98.6 °F), pulse 146 beats/min (normal range: 100 - 160 beats/min), respiration 60 breaths/min (normal range: 30 - 60 breaths/min), blood pressure 73/38 mm Hg (normal range: 60 - 80/30 - 45 mm Hg), and oxygen saturation 100% (normal range: 95-100%). The airway, cardiac, and respiratory examinations were unremarkable. There was a palpable mass in the left upper quadrant of the abdomen. The female neonate was left with her mother for skin-to-skin care and breast feeding. She was transferred to the neonatal intensive care unit (NICU). The infant had emesis following birth and there was a concern for gastrointestinal tract obstruction due to the mass.
Diagnosis
A routine prenatal ultrasound revealed a well-circumscribed cystic mass with fetoid solid internal content in the left upper quadrant of the primary fetus, displacing the stomach anteriorly and the left kidney inferiorly consistent with a FIF. The cyst measured 58.5 × 36 × 46.8 mm. There were no signs of intracystic hemorrhage. The parasitic fetus was acardiac and acephalic. There were rudimentary incomplete extremities with long bones and a very rudimentary spine with distinct vertebrae. The parasitic fetus was attached to the wall of its sac through a vestigial cord vessel with forward arterial flow on color Doppler. The feeding vessel from the host was not definitively identified, but it was thought to most likely be the mesenteric artery. At 35 weeks of gestation, magnetic resonance imaging (MRI) showed a 6-cm mass in the left upper quadrant consistent with a FIF with mass effect on the surrounding structures. Vaginal delivery at 38 weeks was uneventful.
Treatment
The patient was held nil per os and scheduled for an elective exploratory laparotomy and resection of the mass. Preoperative laboratory evaluation including a complete blood count, electrolytes, and renal function was normal. The hemoglobin was 13.4 g/dL with a hematocrit of 38.2%. The echocardiogram showed mild dilatation of the sinu-tubular junction and a patent foramen ovale with a left-to-right atrial shunt. A preoperative radiograph revealed the presence of the FIF in the left upper quadrant (Fig. 1). The anesthesia plan included general anesthesia with a rapid sequence induction followed by caudal epidural catheter placement for intraoperative and postoperative pain management. She was transported to operating room where routine American Society of Anesthesiologists’ monitors were applied. Anesthesia was induced with propofol (10 mg), fentanyl (10 µg), rocuronium (6 mg), and atropine (0.1 mg) using a pre-existing intravenous (IV) line. The patient’s trachea was intubated with 3.0-mm cuffed endotracheal tube on the first attempt using a Miller 1 laryngoscope blade and direct laryngoscopy. A second peripheral 24-gauge peripheral venous cannula was placed in the left hand. Maintenance anesthesia included isoflurane (expired concentration 0.2-0.3%) in air and oxygen. The neonate was placed in the left lateral decubitus and a regional anesthetic time-out was performed. After the skin was cleaned with iodine, sterile towels were placed surrounding the insertion site of the Tuohy needle into the caudal space. After measuring the distance from the caudal inlet (sacrococcygeal ligament) to T9, the location of the sacral hiatus was identified. An 18-gauge Tuohy needle was inserted at a 45° to the skin and redirected when the posterior surface of the sacrum was contacted. After loss of resistance to identify the sacrococcygeal ligament, the caudal epidural catheter was threaded through the Touhy needle until its tip was seen at T9 under ultrasound guidance. After a negative test dose (0.3 mL of 1.5% lidocaine with epinephrine 1:200,000), the caudal catheter was tunneled and fixed to the skin. The insertion site was covered by a chlorhexidine gluconate dressing. A continuous infusion of epidural chloroprocaine 1.5% with clonidine 0.1 µg/mL was started at 2 mL/h. Antibiotics were administered for prophylaxis against a surgical site infection. Maintenance anesthesia was continued with isoflurane (expired concentration 0.2%) in air and oxygen. The procedure lasted 3.5 h. Additional intraoperative analgesic agents included IV fentanyl (2 µg) and a single dose of IV acetaminophen (22.5 mg). There was no hemodynamic response to surgical incision. No intraoperative concerns were encountered. Total fluid intake included 10% dextrose (53 mL), normal saline (66 mL), and 5% albumin (60 mL). Total urine output was 25 mL with minimal blood loss. At the completion of the procedure, residual neuromuscular blockade was reversed with sugammadex (15 mg), and the patient’s trachea was extubated. She was transferred to the NICU. Her postoperative pain management plan included IV acetaminophen 30 mg every 6 h, IV morphine 0.15 mg every 3 h as needed, and the continuous epidural chloroprocaine-clonidine infusion.
 Click for large image | Figure 1. Preoperative radiograph showing the presence of the fetus-in-fetu with calcified bony structures. |
Follow-up and outcomes
On postoperative day (POD) 1, she received two doses of IV morphine and maintained pain scores of 0 - 3 on the FLACC (face, legs, activity, cry, consolability) scale. On POD 2, feeding (10 mL of breast milk every 3 h) was restarted and her (FLACC) behavioral pain scale was noted to be 0. A postoperative chest and abdomen radiograph revealed the enteric feeding tube with the tip within the left upper quadrant (stomach), a normal bowel gas pattern, and the epidural catheter tip at T12 (Fig. 2). Over the ensuing POD 3 - 4, feeds were gradually increased to full volumes. On POD 7, the patient was discharged home.
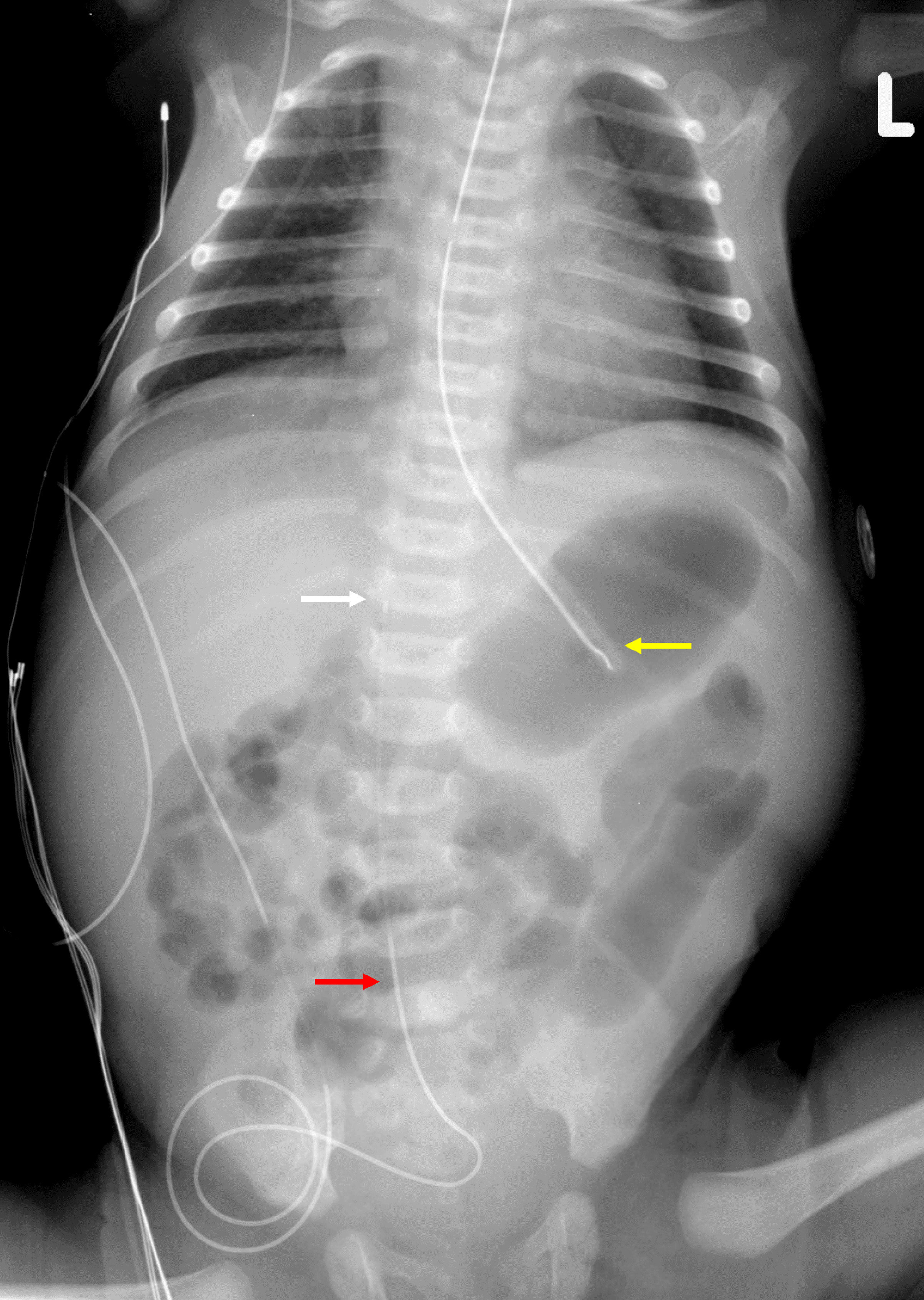 Click for large image | Figure 2. Postoperative radiograph showing the tip of the nasogastric tube (yellow arrow), the epidural catheter in the lumbar region (red arrow), and the tip of the epidural at T12 (white arrow). |
| Discussion | ▴Top |
FIF is one of the more uncommon conditions listed in the differential diagnosis of a neonatal abdominal mass with only approximately 200 cases reported in the published literature. It can be classified into either internal or external FIF. With the internal variant as occurred in our patient, the fetus is within the body of the larger twin and generally presents as an abdominal mass. FIF may present in the neonatal period as noted in our patient and is generally diagnosed at less than 2 years of age. FIF has also been reported in adolescents or adults, even as late as the fourth or fifth decade of life [4-7]. In the external type, the fetus is attached externally to the larger twin and is generally evident at birth. There is a male preponderance with a male to female ratio of 2 to 1. Although the usual presentation is usually a single FIF, multiple fetuses in one patient have been reported [8]. FIF most commonly presents in the retroperitoneal or intra-abdominal space; however, other locations throughout the body have been reported.
The clinical signs and symptoms vary based on location and the mass effect. Common signs and symptoms with an intra-abdominal location include feeding difficulties and vomiting as noted in our patient, abdominal distention, and failure to thrive. Alternatively, it may be noted during routine pre-natal obstetrical ultrasonography and confirmed in utero by MRI. In our case, both prenatal ultrasound and MRI led to the preoperative diagnosis and facilitated immediate excision during the neonatal period. These imaging modalities may be used following birth to confirm the diagnosis, identify the relationship to vital structures, and confirm the blood supply to guide surgical intervention.
One of the main pathologic conditions in the differential diagnosis is teratoma. A teratoma is a neoplasm containing tissue from the three germ layers, endoderm, mesoderm, and ectoderm. It can affect individuals at any age with variable location and clinical presentation. The most common sites for teratomas are the ovary, testes, posterior peritoneum, and the sacrococcygeal region. Cartilage, hair, teeth, single or multiple cysts can be seen within mature teratomas along with either sebum or mucus [9]. Teratomas are classified into three categories: classical, fetiform, and malignant. Fetiform teratomas may develop a high grade of differentiation and organization with a primitive brain and spinal cord similar to that seen in FIF [10]. The primary anatomical differentiating point between FIF and teratoma is the presence or absence of axial skeleton (limbs or vertebral bodies) inside the mass. Visualization of a non-homogenous mass with bones especially vertebrae is considered pathognomonic of FIF. Other differentiating features include normal levels of α-fetoprotein in FIF [11]. Using these differentiating features, our case matched the pathognomonic criteria for FIFs, as there were rudimentary incomplete extremities with long bones and a very rudimentary spine with distinct vertebrae. Additional considerations in the differential diagnosis include other conditions which result in an intra-abdominal mass in neonates and infants including Wilm’s tumor, neuroblastoma, hydronephrotic kidney, and meconium pseudocyst.
The primary therapeutic management is complete surgical excision of the fetus including its capsule to avoid increasing size with a local mass effect on adjacent organs or hemorrhage. Residual membranes or any portion of a FIF increases the possibility of local recurrence or even metastatic dissemination. Although FIF is most commonly a benign congenital anomaly, there is a possibility of an associated teratoma, which has a significant risk of malignant transformation (10%) if left untreated [12]. Hopkins et al reported a 4-month-old neonate who presented with a recurrent malignant right-sided abdominal mass after FIF resection [3]. During excision of the FIF, although the mass was removed, the sac was left in place as it was adherent to the inferior vena cava, ureter, and right renal pedicle.
Table 1 outlines illustrative cases from the literature regarding anesthetic and surgical management during excision of FIF [3, 12-27]. In general, the anesthetic plan will depend on the location of the FIF and the effect of the mass on the patient. Although retroperitoneal and intra-abdominal locations are most common, FIF has also been reported intracranially, within the oropharynx or airway, near the perineum, and within the sacrum. Although there are several case reports of general anesthesia for these patients during excision of the FIF, our review revealed only two previous reports in neonates and infants outlining the use of a combined general-regional anesthetic technique during excision of a FIF [26, 27]. Khatavkar et al reported a 9-kg infant, who presented with a painless abdominal mass present with birth as well as constipation and urinary difficulties [26]. After confirming the diagnosis of FIF using MRI, FIF excision was performed under a combined general-regional technique using epidural anesthesia. Following the induction of general anesthesia, an epidural catheter was placed at L1-2 and an infusion of 0.2% ropivacaine administered at 2 mL/h. After a 5-h surgical procedure, the infant’s trachea was extubated, and the epidural infusion was used to provide postoperative analgesia. Similarly, Agavelyan et al reported the use of a combined general-regional anesthetic technique during FIF excision (epigastrium) with repair of an omphalocele [27]. While still under general anesthesia, an epidural catheter was placed at the L1-2 interspace and threaded up to T9-10 following the surgical procedure to provide postoperative analgesia. On day of life 8, the patient returned to the operating room for repair of a congenital diaphragmatic hernia (CDH). The child died of multisystem organ failure at 25 days of life.
 Click to view | Table 1. Anecdotal Reports of Fetus-in-Fetu in Pediatric-Aged Patients Including Anesthetic Technique as Available |
In our patient, following our usual clinical practice, an epidural catheter was advanced from the caudal epidural space to the desired location using ultrasonography after the induction of general anesthesia and endotracheal intubation [28, 29]. The location of the tip of the catheter was then confirmed on the postoperative abdominal radiograph (Fig. 2). By using a combined general-regional anesthetic technique, we were able to limit the intraoperative requirements for volatile agents and opioids and thereby facilitated tracheal extubation in the operating room. Additionally, the epidural catheter was used postoperatively to provide analgesia by an infusion of chloroprocaine and clonidine [29]. Although not present in our patient, there may be relative and absolute contraindications to regional anesthesia including local infection at the puncture site infection, coagulation disturbances, the administration of therapeutic anticoagulation, severe hypovolemia and hemodynamic dysfunction, degenerative axon and central nervous system diseases, anatomical abnormalities of the vertebral body and spinal cord such as a tethered cord, and increased intracranial pressure (ICP). Additionally, although generally safe and effective, specific adverse effects may occur related to regional anesthesia related to needle and catheter placement as bleeding/hematoma, epidural abscess, inadvertent dural puncture, and injury to the spinal cord. In addition, local anesthetic toxicity (LAST) and block failure can occur [30-32]. Given these concerns, an appropriate pre-block evaluation is indicated to rule out relative and absolute contraindications as well as ongoing monitoring of the patient’s status during the use of regional anesthesia.
Learning points
When considering anesthetic care for FIF procedures, considerations include the location of the mass and its effect on the patient, as well as the implications of providing anesthetic care for a neonate during an exploratory laparotomy. In our patient, we found that our usual practice of a combined general-regional technique with caudal epidural anesthesia facilitated early tracheal extubation in the operating room. Given the intra-abdominal location of the mass in our patient and its compression of the stomach, we chose to use a rapid sequence induction technique to minimize aspiration risk. Other precarious locations of these FIFs have included intracranial with the potential to alter intracranial compliance and increase ICP as well as locations within the airway and a resultant difficult airway with the potential for a “cannot intubate - cannot ventilate scenario”.
Conclusions
Because of advancements in imaging technology, rare congenital anomalies such as FIF may be identified in utero thereby resulting in early excision during the neonatal period. Clinical consequences related to FIF are generally related to its location and the potential for mass effect. Total surgical excision is indicated due to the rare risk of malignant transformation. Implications for anesthetic care relate primarily to the concerns of providing intraoperative care for a neonate during exploratory laparotomy in addition to the consequences related to the location of the FIF. In our patient, we found that our usual practice of a combined general-regional technique with caudal epidural anesthesia facilitated early tracheal extubation in the operating room.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Review of this case and presentation in this format followed the guidelines of the Institutional Review Board of Nationwide Children’s Hospital (Columbus, OH). Informed consent was obtained for use of deidentified information for publication.
Author Contributions
AE provided patient care, case review and preparation of the manuscript including drafts and final version. AS provided intraoperative care of the patient and review of the final manuscript. JDT contributed to manuscript preparation, review, and editing.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Lewis RH. Foetus in foetu and the retroperitoneal teratoma. Arch Dis Child. 1961;36(186):220-226.
doi pubmed pmc - Sutthiwan P, Sutthiwan I, Tree-trakan T. Fetus in fetu. J Pediatr Surg. 1983;18(3):290-292.
doi pubmed - Hopkins KL, Dickson PK, Ball TI, Ricketts RR, O'Shea PA, Abramowsky CR. Fetus-in-fetu with malignant recurrence. J Pediatr Surg. 1997;32(10):1476-1479.
doi pubmed - He Y, Ji Y, Xie G, Wang A. Retroperitoneal fetus in fetu presenting in a male infant: A case report and literature review. Radiol Case Rep. 2022;17(7):2408-2415.
doi pubmed pmc - Dagradi AD, Mangiante GL, Serio GE, Musajo FG, Menestrina FV. Fetus in fetu removal in a 47-year-old man. Surgery. 1992;112(3):598-602.
pubmed - Kumar A, Paswan SS, Kumar B, Kumar P. Fetus in fetu in an adult woman. BMJ Case Rep. 2019;12(8):e230835.
doi pubmed pmc - Sharma S, Gupta PK, Regmi B, Gupta A, Lamichhane U. Fetus in fetu in an adult female and brief review of literature. Case Rep Radiol. 2021;2021:6660277.
doi pubmed pmc - Kimmel DL, Moyer EK, et al. A cerebral tumor containing five human fetuses; a case of fetus in fetu. Anat Rec. 1950;106(2):141-165.
doi pubmed - Xiaowen M, Lingxi C, Song L, Shengbao P, Xiaohong Y, Xinghai Y. Rare fetus-in-fetu: experience from a large tertiary pediatric referral center. Front Pediatr. 2021;9:678479.
doi pubmed pmc - Weiss JR, Burgess JR, Kaplan KJ. Fetiform teratoma (homunculus). Arch Pathol Lab Med. 2006;130(10):1552-1556.
doi pubmed - Rahman GA, Abdulkadir AY. Fetus in Fetu: A Rare presentation in an Adult female. Oman Med J. 2011;26(1):66.
doi pubmed pmc - Ji Y, Chen S, Zhong L, Jiang X, Jin S, Kong F, Wang Q, et al. Fetus in fetu: two case reports and literature review. BMC Pediatr. 2014;14:88.
doi pubmed pmc - Traisrisilp K, Srisupundit K, Suwansirikul S, Norasetthada T, Kosarat S, Tongsong T. Intracranial fetus-in-fetu with numerous fully developed organs. J Clin Ultrasound. 2018;46(7):487-493.
doi pubmed - Afshar F, King TT, Berry CL. Intraventricular fetus-in-fetu. Case report. J Neurosurg. 1982;56(6):845-849.
doi pubmed - Runggaldier D, Reinehr M, Friedrich H, Henze G, Good D, Gysin C. Case report and review of the literature: rare fetus-in-fetu presenting as oropharyngeal epignathus. Front Surg. 2023;10:1122327.
doi pubmed pmc - Yu YR, Espinoza J, Mehta DK, Keswani SG, Lee TC. Perinatal diagnosis and management of oropharyngeal fetus in fetu: A case report. J Clin Ultrasound. 2018;46(4):286-291.
doi pubmed - Woodard TD, Yong S, Hotaling AJ. The Ex Utero Intrapartum Treatment (EXIT) procedure used for airway control in a newborn with cervical fetus in fetu: a rare case. Int J Pediatr Otorhinolaryngol. 2006;70(11):1989-1994.
doi pubmed - Derniaux E, Zachar D, Bory JP, Gaillard D, Favre R, Graesslin O. Detection of a prenatal mature tumor arising from the external genitalia in a female fetus: fetus-in-fetu or teratoma? Prenat Diagn. 2010;30(11):1110-1111.
doi pubmed - Gangopadhyay AN, Srivastava A, Srivastava P, Gupta DK, Sharma SP, Kumar V. Twin fetus in fetu in a child: a case report and review of the literature. J Med Case Rep. 2010;4:96.
doi pubmed pmc - Karaman I, Erdogan D, Ozalevli S, Karaman A, Cavusoglu YH, Aslan MK, Cakmak O. Fetus in fetu: A report of two cases. J Indian Assoc Pediatr Surg. 2008;13(1):30-32.
doi pubmed pmc - Coolen J, Bradshaw B, Bhargava R, Lees G, Demianczuk N. Fetus-in-fetu: confirmation of prenatal diagnosis with MRI. Prenat Diagn. 2007;27(1):73-76.
doi pubmed - Gerber RE, Kamaya A, Miller SS, Madan A, Cronin DM, Dwyer B, Chueh J, et al. Fetus in fetu: 11 fetoid forms in a single fetus: review of the literature and imaging. J Ultrasound Med. 2008;27(9):1381-1387.
doi pubmed - Santos H, Furtado A, Tavares HB, Joao A, Ferraz L, Ferreira G, Nogueira R, et al. [Pre-natal retroperitoneal mass: teratoma or fetus in fetu?]. Cir Pediatr. 2008;21(3):185-187.
pubmed - Joshi M, Parelkar S, Shah H, Agrawal A, Mishra P. Foetus in fetu with common bile duct injury: a case report and review of literature. ANZ J Surg. 2009;79(9):651-652.
doi pubmed - Sharma A, Goyal A, Sharma S. Fetus in fetu: A rare case report. J Res Med Sci. 2012;17(5):491-494.
pubmed pmc - Khatavkar SS, Kabeer W, Ghodake AP, Shah KS. Anaesthetic management of foetus in foetu: A rare entity. Indian J Anaesth. 2023;67(Suppl 1):S68-S69.
doi pubmed pmc - Agavelyan EG, Svarinskaya EM, Ovchinnikov SV. [Anesthesia during the separation of the fetus in fetu in a 2 days-life child with accompanying non-corrected critical congenital heart disease (Chd)]. Anesteziol Reanimatol. 2016;61(1):47-51.
pubmed - Goeller JK, Bhalla T, Tobias JD. Combined use of neuraxial and general anesthesia during major abdominal procedures in neonates and infants. Paediatr Anaesth. 2014;24(6):553-560.
doi pubmed - Veneziano G, Tobias JD. Chloroprocaine for epidural anesthesia in infants and children. Paediatr Anaesth. 2017;27(6):581-590.
doi pubmed - Rios-Medina AM, Caicedo-Salazar J, Vasquez-Sadder MI, Aguirre-Ospina OD, Gonzalez MP. Regional anesthesia in pediatrics - Non-systematic literature review. Col J Anesthesiology. 2015;43(3):204-213.
- Walker BJ, Long JB, Sathyamoorthy M, Birstler J, Wolf C, Bosenberg AT, Flack SH, et al. Complications in pediatric regional anesthesia: an analysis of more than 100,000 blocks from the pediatric regional anesthesia network. Anesthesiology. 2018;129(4):721-732.
doi pubmed - Ecoffey C, Lacroix F, Giaufre E, Orliaguet G, Courreges P, Association des Anesthesistes Reanimateurs Pediatriques d'Expression F. Epidemiology and morbidity of regional anesthesia in children: a follow-up one-year prospective survey of the French-Language Society of Paediatric Anaesthesiologists (ADARPEF). Paediatr Anaesth. 2010;20(12):1061-1069.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.