| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 4, April 2013, pages 218-220
Chronic Gastric Volvulus in Traumatic Hiatus Hernia Managed by Gastrostomy
Nikolaos Andromanakosa, d, Nikolaos Roukounakisb, Ilias Karantonisc, Vasilios Mouziourasa, Antonios Diamantopoulosa, Maria Melab, Ageliki Christidoub, Alkiviadis Kostakisc
aDepartment of General Surgery, Athens “Polykliniki” General Hospital, Athens, Greece
bDepartment of Gastroenterology, Athens “Polykliniki” General Hospital, Athens, Greece
cSecond Department of Propedeutic Surgery, Athens University Medical School, Laiko General Hospital, Athens, Greece
dCorresponding author: Nikolaos Andromanakos, 10A Glafkis str., GR-15232 Halandri, Athens, Greece
Manuscript accepted for publication January 2, 2013
Short title: Chronic Gastric Volvulus
doi: https://doi.org/10.4021/jmc1041w
| Abstract | ▴Top |
Gastric volvulus is a rare entity. It occurs more frequently in the elderly with a hiatus hernia and only in 10-20% in infants and children. We report a rare case of an elderly patient with chronic gastric volvulus in traumatic hiatus hernia after a severe injury of the chest. He had a medical history of diabetes mellitus, severe cardiopathy with pacemaker, chronic respiratory disease and six months ago a road accident with a severe injury of the chest. Gastric volvulus was diagnosed endoscopically, confirmed radiologically and managed operatively with fixation of the stomach by gastrostomy. The patient during the diagnostic approach and until the surgical procedure was managed by nasogastric tube without bilious backflow, intravenous fluid administration, balance of electrolyte and parenteral nutrition. The successful treatment of the gastric volvulus with a simple fixation of the stomach on the anterior abdominal wall justifies the decision to avoid an attempt of hiatus hernia repair particularly in an elderly patient with a high operative risk. However, a delayed diagnosis may be threatening to the patient’s life and what should be highlighted is the difficulty of the diagnosis and the management in rare cases, such as chronic volvulus of the stomach.
Keywords: Stomach; Volvulus; Torsion; Hiatus hernia
| Introduction | ▴Top |
Gastric volvulus is a rare entity. It is torsion of the stomach anteriorly or posteriorly around its longitudinal or horizontal axis [1]. The symptoms may be incomplete or periodic obstruction with dysphagia and regurgitation or vomiting. Acute volvulus is manifested as an acute upper gastrointestinal obstruction and rarely, if there is vascular obstruction and necrosis, as an acute abdominal emergency [2]. Gastric volvulus occurs most frequently in the elderly and only in 10-20% in infants and children [3]. In the elderly patient, gastric volvulus is usually associated with a hiatus hernia. It relates to displacement of the stomach through the hiatus into the chest that produces vigorous peristalsis and antiperistalsis predisposing to volvulus [4]. We report a rare case of an elderly patient with chronic volvulus of the stomach in traumatic hiatus hernia after a severe injury of the chest by a road accident which was diagnosed endoscopically, documented radiologically and managed operatively by a successful gastrostomy. However, a delayed diagnosis may be threatening to the patient’s life and what should be highlighted is the difficulty of the diagnosis and the management in rare cases, such as chronic volvulus of the stomach.
| Case Report | ▴Top |
An 84-year-old man admitted to our hospital with a 2 months history of dyspepsia and intermittent non-bilious vomiting. He had a medical history of diabetes mellitus, severe cardiopathy with pacemaker, chronic respiratory disease and six months ago a road accident with a severe injury of the chest. Physical examination revealed a heavily ill patient with Hippocratic face and malnutrition. The pathological findings from the abdomen and respiratory system were succussion splash of the stomach and decrease of respiratory murmur in the left lung. Laboratory data besides an anemia, hypoproteinemia and electrolyte disorders, the other blood investigations, as well as tumor markers, were within normal limits. Gastroscopy revealed a hiatus hernia and ulcerative lesions of the gastric mucosa close to the gastro-esophageal area, the fundus and the posterior surface of the body. Biopsies from the edges were obtained four times, which showed no evidence of malignancy. Furthermore, it posed the suspicion of the gastric volvulus because gastroscopy failed to enter in the distal stomach, the lumen appeared to narrow to a point through which the endoscope could not be passed. Chest and Abdomen x-ray showed a high left hemidiaphragm with a large air bubble above a fluid level in dilated stomach. Abdominal and Thorax CT scan showed rupture of the left hemidiaphragm and old ribs fractures of the left hemithorax. However, barium meal (Fig. 1) confirmed, apart from hiatus hernia, the diagnosis of the gastric volvulus. The final diagnosis of the severely ill patient was traumatic hiatus hernia and gastric volvulus, which led us to reach a decision of surgical treatment. The preoperative preparation was supplemented by a detailed examination of the heart and the respiratory system, arterial blood gases as well as spirometry test. He was of high perioperative risk because of the severe concomitant diseases and his malnutrition. The patient during the diagnostic approach and until the surgical procedure was managed by nasogastric tube without bilious backflow, intravenous fluid administration, adjustment of electrolyte and parenteral nutrition. Laparotomy was carried out through a midline incision. The stomach was found to be almost throughout, about 2/3 of it, into the thorax through a large hiatus of the diaphragm. It was in incomplete anterior torsion around the horizontal axis and the pylorus and duodenum were elongated and stretched. In addition, it was fixed in the thorax posteriorly at the cardiac portion and part of the fundus. Consequently, it was reduced partially after pull and sufficient mobilization of the greater and the lesser curvature. However, the high operative risk of the patient did not permit a major procedure of hiatus hernia repair. Thereby, it was decided that the fixation of the stomach would be simplest and safest procedure to prevent displacement and rotation. The fixation was performed by gastrostomy drainage at the level of the antrum. The stomach wall was sutured by the anterior abdominal wall at the gastrostomy exit using 0 vicryl sutures. The abdomen was then closed without peritoneal drainage. Postoperative course of the patient was with no complications. He was able to drink on the 3rd postoperative day and the gastrostomy tube was clamped. A barium meal examination was done on the 5th postoperative day (Fig. 2) and the gastrostomy tube was removed uneventfully on the 12th postoperative day. After that, he discharged on the 14th postoperative day and he remains well since.
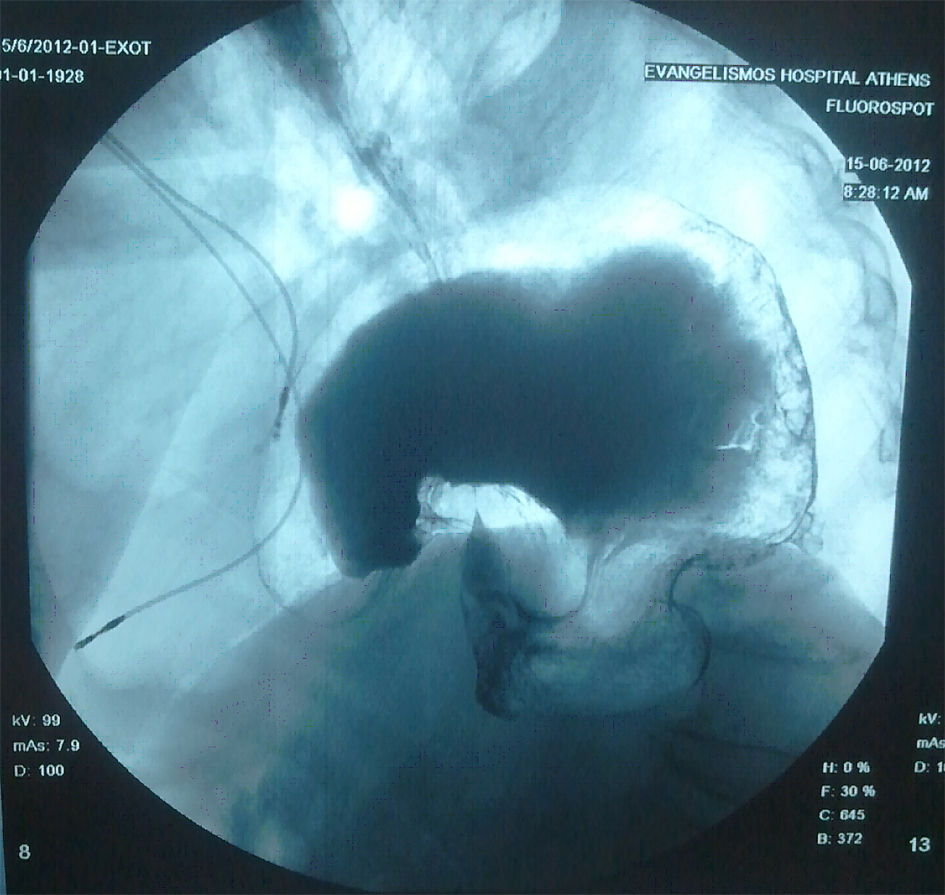 Click for large image | Figure 1. X-ray of barium meal examination: gastric volvulus, in anterior torsion at the horizontal axis. |
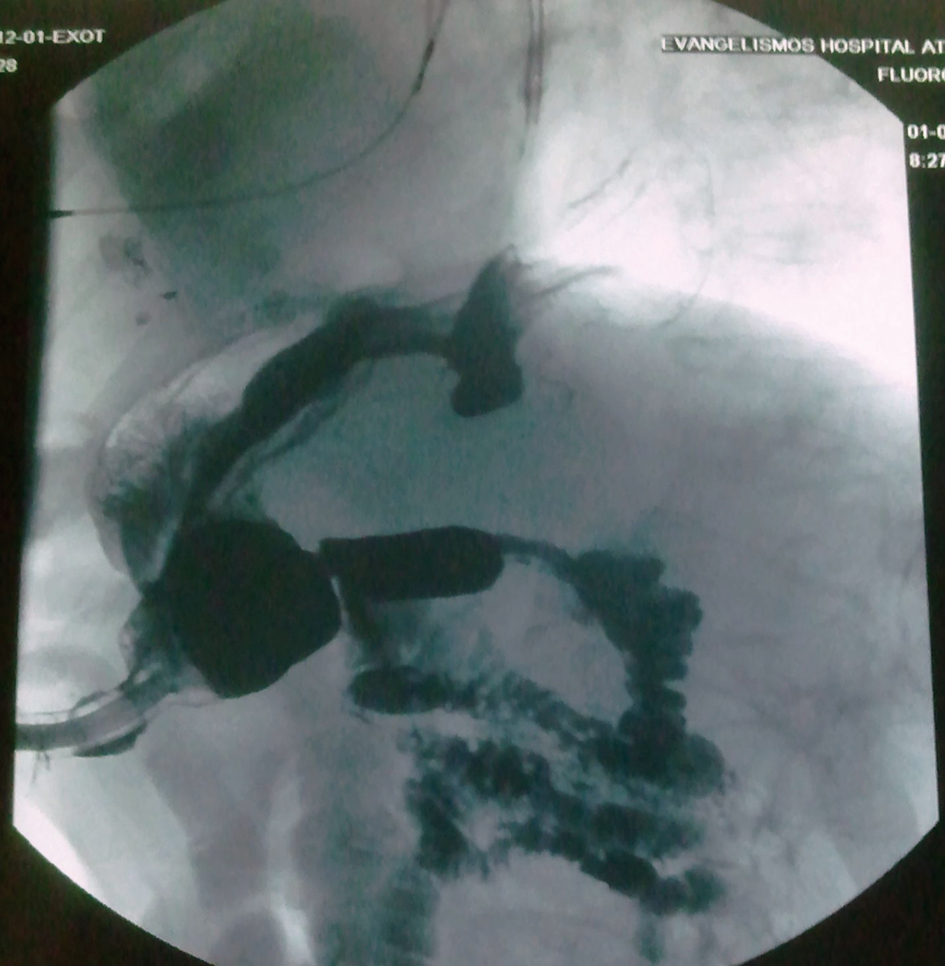 Click for large image | Figure 2. X-ray of barium meal examination on the 5th postoperative day: gastrostomy and gastric volvulus reduction |
| Discussion | ▴Top |
A detailed description of the anatomic and functional disorders which may predispose to gastric volvulus was reported by Tanner in 1968 [4]. In our patient the cause of the gastric volvulus was apparently secondary. It was a diaphragm rupture after a severe injury of the thorax by a road accident that favoured the displacement of the stomach into the chest. Thereby, a traumatic hiatus hernia had been produced which led to the gastric volvulus. Here, it should be emphasized the difficulty to differentiate the ischemic ulcerative lesions of the gastric mucosa by the torsion from the malignancy, which was excluded by successive biopsies. After final diagnosis there has been a great problem, what we could do therapeutically in our patient who was elderly with a high operative risk. The complete rehabilitation of the gastrointestinal function after fixation of the stomach on the anterior abdominal wall by gastrostomy justifies the decision to avoid an attempt to repair the hiatus hernia which could threaten the patient’s life. However, the success of the simple fixation of the gastric volvulus could also be achieved by a minimally invasion technique, such as endoscopic or laparoscopic [5], except a case of gastric volvulus, as in our patient, which may be the result of a traumatic hiatus hernia after a severe injury of the thorax.
Conclusion
The successful treatment of the gastric volvulus with a simple fixation of the stomach by gastrostomy justifies the decision to avoid an attempt of major procedure, which could threaten the patient’s life, particularly in an elderly patient with a high operative risk.
Conflict of Interest
The authors declare that there is no conflict of interest.
| References | ▴Top |
- Wastell C, Ellis H. Volvulus of the stomach. A review with a report of 8 cases. Br J Surg. 1971;58(8):557-562.
doi - Laurent S, Grayet D, Lavigne Ch M. Acute and chronic gastric volvulus: radical different prognosis and management. Case report. Acta Chir Belg. 2010;110(1):76-79.
pubmed - Harford WV, McArthur KE. Diverticula, hernias, volvulus, and rupture. In: Sleisenger MH, Fordtran JS, eds. Gastrointestinal Disease: Pathophysiology, Diagnosis, Management. Philadelphia, MB Saunders, 1993: 481-483.
- Tanner NC. Chronic and recurrent volvulus of the stomach with late results of "colonic displacement". Am J Surg. 1968;115(4):505-515.
doi - Rashid F, Thangarajah T, Mulvey D, Larvin M, Iftikhar SY. A review article on gastric volvulus: a challenge to diagnosis and management. Int J Surg. 2010;8(1):18-24.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


