| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 4, April 2013, pages 259-261
Isolated Fracture of the Lesser Trochanter as a First Manifestation of Metastatic Lung Carcinoma
Diego Reategui-Villegasa, b, Pilar Camacho Carrascoa, Alonso Zumbado Dijeresa, Jose Ballesteros Betancourta
aOrthopaedic Department, Hospital Clinic Barcelonam, Spain
bCorresponding author: Diego Reategui-Villegas, Orthopaedic Department, Hospital Clinic de Barcelona, Escalera 12, 4aplanta. C/ Villarroel 170. 08036. Barcelona, Spain
Manuscript accepted for publication January 22, 2013
Short title: Isolated Fracture of the Lesser Trochanter
doi: https://doi.org/10.4021/jmc1077w
| Abstract | ▴Top |
Isolated fractures of the lesser femoral trochanter in adults without previous trauma, are rare, so an underlying pathology should be suspected. As a first option, a neoplastic process must be taken into account. Because the most frequent neoplastic pathology is metastases, a thorough medical history has to be taken and additional test must be done to diagnose the primary lesion. We report a case of a patient who presented with an isolated fracture of the lesser trochanter as the first manifestation of primary lung carcinoma.
Keywords: Lesser trochanter; Metastasis; Cancer
| Introduction | ▴Top |
Isolated fractures of the lesser trochanter are uncommon at any age. Those that occur in children or young people, are caused by vigorous activity [1, 2], usually in the context of contact sport and as a result of sudden contraction of the iliopsoas muscle [3]. However, those seen in adults in the absence of previous trauma, should raise the suspicion of a neoplastic process [1-4]. We present the case of a patient who presented an isolated fracture of the femoral lesser trochanter as the first manifestation of metastatic lung cancer.
| Case Report | ▴Top |
Sixty-nine year old male patient, smoker (55 packs/year), with a history of diabetes mellitus and a surgically treated right lumbar disc herniation 10 years before admission, who walked with a cane because of weakness in right leg. He presented in the emergency department of our hospital with moderate intensity pain at the right hip that worsened at night and had started two months before consultation.
Physical examination showed tenderness in the right greater trochanter area, preserved active and passive mobility of hip though painful in the entire range of motion. Examination of the respiratory system showed hypophonesis in left hemithorax. Complete blood count had leukocytosis with neutrophilia and hyperglycaemia. Hip X ray revealed a displaced isolated right lesser trochanter fracture (Fig. 1A, B). Chest radiograph showed the presence of a collapsed right lung and left pulmonary hilum tumor (Fig. 1C).
 Click for large image | Figure 1. A) Anteroposterior radiograph of the pelvis with avulsion fracture of right lesser femoral trochanter. B) Axial radiograph of right hip with isolated lesser trochanter fracture and no other associated bone lesions. C) Anteroposterior chest radiograph shows massive atelectasis of the right lung and left lung hilum tumor. |
On suspicion of lung cancer with bone metastasis and pathological fracture of the lesser trochanter, hospitalization at the Department of Pneumology was decided. During hospitalization tumor markers analysis (CA 125, CYFRA 21.1, SCC, neuron-specific enolase) were performed and bronchoscopy revealed non-small cell lung carcinoma. Bone scintigraphy with technetium 99, showed lytic lesions in the left iliac crest, rib cage, 5th lumbar vertebrae, and an irregular captation site at the right proximal femur region corresponding to fracture (Fig. 2A). The CT scan demonstrated enlarged mediastinal lymph nodes, rib and vertebral metastases. (Fig. 2B).
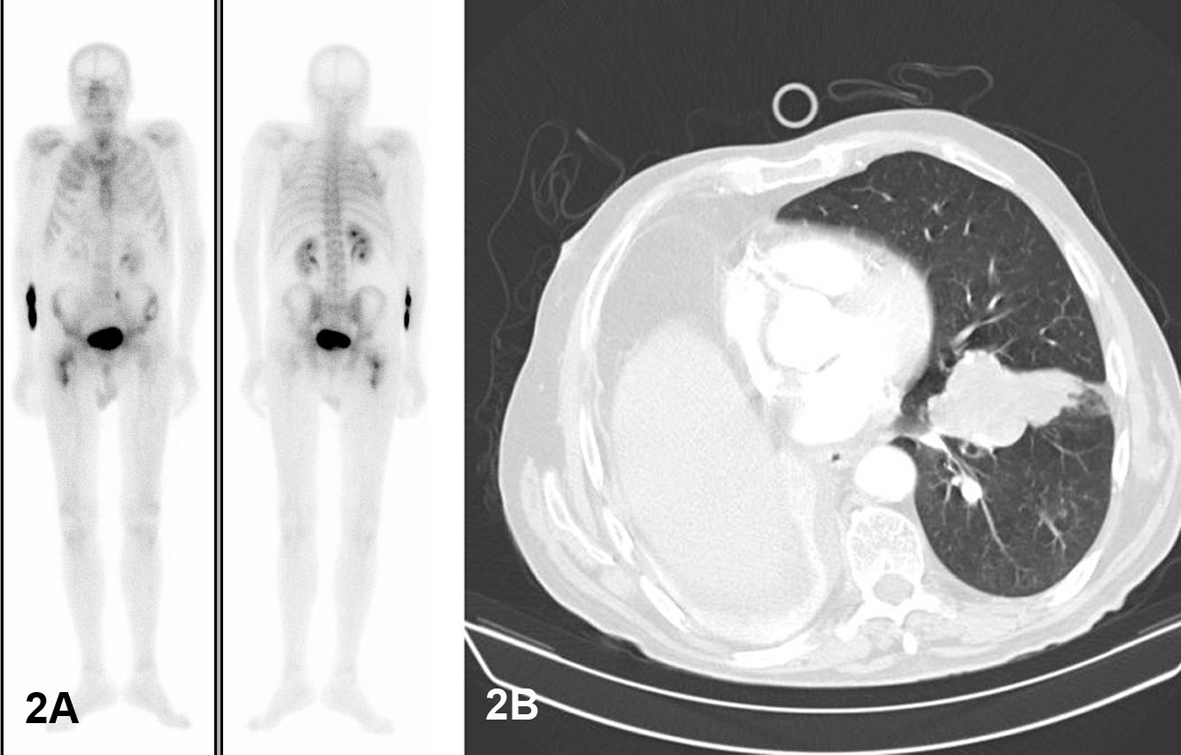 Click for large image | Figure 2. A) Tc 99 Bone scintigraphy: Vascular phase: hyperemia in the right proximal femur and left iliac crest. In the bone phase (two hours after the injection of TC99): lytic lesion in the left iliac crest and irregular hyperemia consistent with that observed in the right proximal femur. B) Chest CT: Massive atelectasis of the right lung and irregular mass in left lung lingula, M1 at 5th dorsal vertebra. |
The case was discussed by the tumors interdisciplinary committee, and prophylactic surgery of the right hip by intramedullary nailing and, subsequent possible chemotherapy were decided. Due to the rapid deterioration of the patient’s lung function, elective surgery could not be performed and 19 days after hospitalization, the patient died of respiratory failure.
| Discussion | ▴Top |
Isolated fractures of the femoral lesser trochanter in adults are rare [1, 2, 4, 5]. There are 33 cases reported in the literature [1]. In the first study which was conducted by Bertin et al [1], 36 cases of isolated fractures of the lesser trochanter were collected, of which only 4 were in adults with no history of direct trauma or fall. Of these, all were secondary to metastases: one thyroid, one pancreatic, one prostate and one adenocarcinoma of unknown origin. All patients were in good general condition before the diagnosis of the fracture. This paper also mentions that retrospectively reviewing the radiographs, obvious radiographic changes suggestive of metastasis were missed.
In a radiological study Phillips et al [2] collected, 4 cases of metastasis. In these cases, primary tumors were: colon, prostate, bronchial adenocarcinoma and Hodgkin lymphoma. In the largest study conducted on tumor processes of the proximal femur by James and Davies [4], 295 cases were identified retrospectively over a period of 20 years. Of these cases, only 15 were atraumatic fractures of the lesser femoral trochanter. Metastases were the most common cause (60%), and the most common primary tumors were: breast, bronchus, kidney, bladder and melanoma. The remaining cases (40%) were diagnosed of myeloma, Ewing sarcoma, chondrosarcoma, non-Hodgkin lymphoma, and giant cell tumor of bone. The study also noted that incidence of 5% of the lesser trochanter avulsion fractures was probably enlarged because the study was conducted in an orthopedic oncology center.
As for primary tumor lesions of bone, Afra R, Boardman DL [4] were the first to describe the avulsion of the lesser trochanter as a primary manifestation of non-metastatic cancer, which corresponded to chondrosarcoma [2], Ewing sarcoma [1] and solitary plasmacytoma [1]. Finally, a single case of leukemia in a patient with avulsion of the lesser trochanter as a primary lesion has been published [6]. After a review of the literature Rouvillain JL et al, state that the etiology of Isolated fractures of the femoral lesser trochanter in adults with no history of trauma is metastatic most of the times, accounting for 70% of cases (3). The most frequent primary causes are: myeloma (9%), chondrosarcoma (9%) and Ewing sarcoma (6%) [4].
To diagnose these lesions, an antero-posterior and axial hip radiograph are necessary. It is important to take into account that an older patient with this type of injury and no history of trauma, should raise the suspicion of an underlying neoplastic process. After diagnosis, many authors recommend a magnetic resonance imaging to study the trochanteric region and display the extent of tumor infiltration to plan tumor resection [2, 4-6]. In our case it was not performed due to advanced stage of the primary tumor. To rule out other bone metastases, some authors recommend a technetium-99 scintigraphy [5, 6]. In the case presented it allowed the diagnosis of rib and vertebral metastases.
Finally, treatment of these patients depends on the stage of primary tumor, as discussed previously. In advanced stages, prophylactic fixation associated with palliative treatment of tumor is the most recommended treatment [1]. In patients with single metastases or controlled primary tumor, resection of the lesion and proximal femoral prosthetic replacement is recommended. In this sense Rouvillain et al report a case of resection-reconstruction by megaprosthesis of the proximal femur in a patient with an isolated fracture of the femoral lesser trochanter secondary to metastatic lung adenocarcinoma [3]. In the case presented, prophylactic nailing was planned but it was not performed because of the patient’s respiratory rapid deterioration.
In conclusion, in an older patient (adult) with an isolated lesser femoral trochanter fracture, without traumatic history, an underlying neoplastic process must be suspected. Because metastatic infiltratyive processes are the most common cause of these fractures, thorough medical history and additional tests need to be performed in order to diagnose the primary lesion.
| References | ▴Top |
- Bertin KC, Horstman J, Coleman SS. Isolated fracture of the lesser trochanter in adults: an initial manifestation of metastatic malignant disease. J Bone Joint Surg Am. 1984;66(5):770-773.
pubmed - Phillips CD, Pope TL, Jr., Jones JE, Keats TE, MacMillan RH, 3rd. Nontraumatic avulsion of the lesser trochanter: a pathognomonic sign of metastatic disease? Skeletal Radiol. 1988;17(2):106-110.
doi pubmed - Rouvillain JL, Jawahdou R, Labrada Blanco O, Benchikh-El-Fegoun A, Enkaoua E, Uzel M. Isolated lesser trochanter fracture in adults: an early indicator of tumor infiltration. Orthop Traumatol Surg Res. 2011;97(2):217-220.
doi pubmed - James SL, Davies AM. Atraumatic avulsion of the lesser trochanter as an indicator of tumour infiltration. Eur Radiol. 2006;16(2):512-514.
doi pubmed - Afra R, Boardman DL, Kabo JM, Eckardt JJ. Avulsion fracture of the lesser trochanter as a result of a preliminary malignant tumor of bone. A report of four cases. J Bone Joint Surg Am. 1999;81(9):1299-1304.
pubmed - Heiney JP, Leeson MC. Isolated lesser trochanter fracture associated with leukemia. Am J Orthop (Belle Mead NJ). 2009;38(3):E56-58.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


