| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 3, March 2013, pages 179-181
A Fatal Case of Misdiagnosed Cryptococcal Epididymo-Orchitis and Leg Cellulitis in a HIV-Negative Patient
Maria Katsiaria, e, Maria Laskoua, Ioannis Provatasb, Maria Theodorakopouloub, Zoi Roussouc, Sotirios Haramoglisd, Asimina Maguinaa
aIntensive Care Unit, Konstantopouleio General Hospital, Athens, Greece
bDepartment of Pathology, Konstantopouleio General Hospital, Athens, Greece
cDepartment of Clinical Microbiology, Konstantopouleio General Hospital, Athens, Greece
dUrology Department, Metropolitan Hospital, Athens, Greece
eCorresponding author: Maria Katsiari, 3-5, Agias Olgas street, 14233 Nea Ionia, Athens, Greece
Manuscript accepted for publication December 7, 2012
Short title: Disseminated Cryptococcosis
doi: https://doi.org/10.4021/jmc1053e
| Abstract | ▴Top |
Patients with disorders of T-cell mediated immunity are at high risk for cryptococcal infection. We present a 61-year-old male who was receiving corticosteroid therapy for vasculitis-associated necrotizing glomerulonephritis. The patient presented with fever, right orchiepididymitis and cellulitis of both legs. Despite surgical and combined antibiotic treatment, he developed septic shock and multi-organ dysfunction. Histological examination of skin lesion revealed acute panniculitis and numerous fungi spores, while blood cultures revealed Cryptococcus neoformans. Further stains on the testis specimen confirmed also the presence of Cryptococcus. The patient received amphotericin B and his clinical condition and laboratory findings were improved. However, he developed septic shock due to multi-drug resistant Klebsiella pneumoniae nosocomial pneumonia and he finally died. Cryptococcal infection should be added to the differential diagnosis of epididymo-orchitis and cellulitis in immunocompromised hosts. Early diagnosis and therapy are essential if the case-fatality rates associated with disseminated infection are to be improved.
Keywords: Immunocompromised patient; Disseminated cryptococcosis; Epididymo-orchitis; Cellulitis; Granulomatous necrotizing inflammation
| Introduction | ▴Top |
Cryptococcal infection is unusual in healthy people, but patients with disorders of T-cell mediated immunity, such as human immunodeficiency virus (HIV) infection or lymphoreticular malignancy or extreme immunosuppression after corticosteroid therapy or organ transplantation are at high risk [1, 2]. It can involve any organ following dissemination. Involvement of the genitourinary tract by fungal infection is uncommon, while cutaneous involvement occurs in approximately 15% of cases [1]. We describe an immunocompromised male with simultaneous genitourinary and cutaneous presentation of disseminated cryptococcosis, diagnosed upon histologic examination.
| Case Report | ▴Top |
A 61-year-old male presented with fever, right orchiepididymitis and cellulitis of both legs. The patient was receiving corticosteroid therapy for 3.5 consecutive years for vasculitis-associated necrotizing glomerulonephritis and had also received cyclophosphamide and mycophenolate mofetil at the time of diagnosis. He was corticosteroid-dependant, as his disease relapsed every time methylprednisolone was tapered to lower doses.
The patient was admitted in the urology department, and surgical exploration resulted in right epididymo-orchiectomy. An empiric scheme of ciprofloxacin, piperacillin/tazobactam and clindamycin was administered. His blood tests revealed normocytic anemia, thrombocytopenia and cholestasis. As histological examination of the testicle revealed a granulomatous necrotizing inflammation (Ziehl-Nielsen negative), anti-tuberculous agents were added (rifampicin, isoniazid, pyrazinamide and ethambutol) to his regimen. Despite surgical and combined antibiotic treatment, the patient remained febrile (daily temperature up to 38.5 °C). Three weeks after admission, he was intubated and transferred to the Intensive Care Unit (ICU) because he developed oliguria, respiratory failure, shock, lactic acidosis and depressed level of consciousness.
Upon arrival, he was hemodynamically unstable, hypothermic, with severe metabolic acidosis. His laboratory tests revealed mild leukocytosis (12870/mm3) with left shift (94% granulocytes), normocytic anemia (Hb = 9.7 gr/dL), thrombocytopenia (67000/mm3), renal failure (urea = 207 mg/dL, creatinine = 2.1 mg/dL), cholestasis (ALP = 207 IU/L, γGT = 209 IU/L, bilirubin = 3.27 mg/dL) and prolonged PT/INR (PT = 26 sec, INR = 2.4 and aPTT = 85 sec). His chest x-ray and oxygenation levels were normal (PaO2/FiO2 = 492 mmHg). Physical examination revealed only skin lesions: cellulitis and ulcers on the anterior surface of both legs and dispersed small sized purpuric lesions.
Resuscitation was initiated and after blood and urine cultures were obtained, the patient was treated parenterally with meropenem, teicoplanin and clindamycin. The daily dose of prednisolone was increased and anti-tuberculous drugs were discontinued. A urine culture revealed 20.000 cfu/mL fungi and, as a result, caspofungin was added to the antibiotic therapy. Due to further deterioration of cholestasis (bilirubin = 20.46 mg/dL, γGT = 1013 IU/L), a CT scan of the abdomen and scrotum was obtained. An enlarged gallbladder with pericholocystic fluid collection was revealed, while no signs of inflammation of prostate or pelvis were identified. Upon the diagnosis of acalculus cholecystitis, the gallbladder was laparoscopically removed. At the same time, a tissue biopsy of skin lesion on the left leg was obtained. After seven days of incubation, blood cultures obtained upon ICU admission revealed Cryptococcus neoformans. Parenteral liposomal amphotericin B (4 mg/kg/day) was immediately added.
A brain CT scan and a lumbar puncture were performed. All studies of the cerebrospinal fluid were negative, including the cryptococcal antigen titer. Laboratory examination showed a positive serum cryptococcal antigen (1:64). Histological examination of a skin specimen (hematoxylin and eosin, periodic acid-Schiff and periodic acid-Schiff diastase stains) revealed acute panniculitis and cryptococcal infection, disclosing numerous fungi spores (Fig. 1), and a culture isolated Cryptococcus neoformans. The epidermis and dermis remained intact. Histological examination of the gallbladder was negative for fungi, while further stains (periodic acid-Schiff, Croccot, blennocarmin) on the testis specimen confirmed the presence of Cryptococcus.
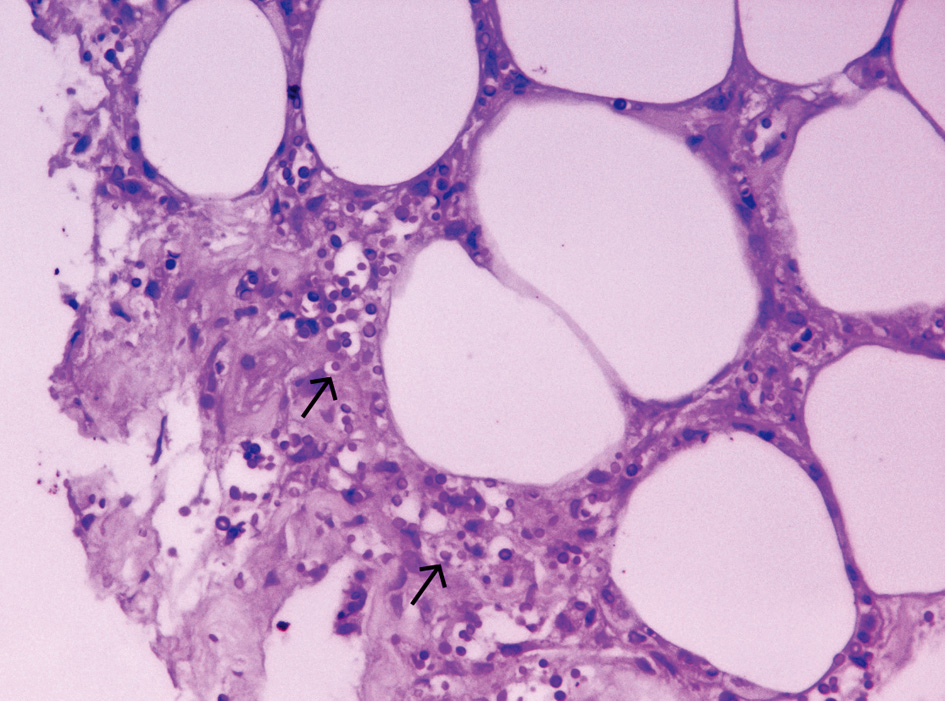 Click for large image | Figure 1. Piece of subcutaneous biopsy that discloses spores of fungi (arrows) (Hematoxylin and Eosin stains × 400). |
Five days after treatment with amphotericin B was initiated, the patient’s laboratory findings improved (creatinine = 0.6 mg/dL, bilirubin = 9.79 mg/dL, γGT = 568 IU/L) and being afebrile, with hemodynamic and respiratory stability, he was extubated. Six days after the extubation, he became septic with high fever (39 °C), respiratory failure and hemodynamic instability and needed to be re-intubated. Urine culture, as a mode of a follow up of genitourinary tract fungal infection, revealed no cryptococci. New infiltrates appeared on his chest x-ray, while multi-resistant Klebsiella pneumoniae was isolated in bronchial secretions. Despite modification on antibiotic therapy, he developed refractory septic shock and succumbed to a multiple organ failure six days later.
| Discussion | ▴Top |
Cryptococcosis crosses the entire spectrum of patient populations, from the apparently immunocompetent hosts to those severely immunocompromised [1]. Corticosteroids are a predisposing factor in 5.4% of patients with cryptococcosis and the long-term high doses received periodically in this case strongly support its etiological role [2]. Cryptococcosis has a wide range of clinical presentations. After pulmonary and central nervous system (CNS) sites of infection, the skin is the third most commonly infected organ. Cryptococcus neoformans can produce a vast variety of skin lesions, including subcutaneous masses, abscesses, draining sinuses, ulcers, granulomas, papulonodules, pustules and plaques [1]. In severely immunocompromised patients, skin infections may present as cellulitis or an abcess that mimics a bacterial skin infection in both appearance and onset rapidity [1]. Although cutaneous involvement occurs in up to 15% of patients with disseminated cryptococcosis, cellulitis has been rarely reported [3, 4]. Skin lesions, may occur before other manifestations of systemic cryptococcosis [1]. These patients are frequently treated empirically for a presumed bacterial cellulitis with no response, as in this case [5]. Needle aspiration or biopsy of new cutaneous lesions must be performed early in immunocompromised hosts.
In the present case, cryptococcosis appeared with simultaneous involvement of skin and genitourinary tract, reflecting systemic dissemination. Involvement of the genitourinary system is relatively uncommon [1, 2]. Cryptococcal infections of the kidney, prostate gland and epididymis have been reported [6]. However, the testis has been previously described as a site of cryptococcal infection only in one HIV-negative patient [7]. The granulomatous necrotizing inflammation of our patient’s testis was misdiagnosed as a mycobacterial infection. Similarly, in a recent retrospective study of cryptococcosis in HIV-negative patients, 14% of the patients were initially misdiagnosed and treated for tuberculosis [8]. Granulomatous epididymo-orchitis can be encountered in a variety of infectious and non-infectious diseases. However, the appearance of the granulomata in routine stains at light microscopy may be indicative of the etiology and special stains for agents such as mycobacteria, spermatozoa and fungi are mandatory. With routine histopathological stains, such as hematoxylin and eosin, the yeasts are surrounded by empty spaces, reflecting the capsule (Fig. 1). The polysaccharide capsule can be identified with stains, such as mucicarmine and alcian blue, and its ability to produce melanin allows it to be stained with the Fontana-Masson stain. Gomori’s methenamine silver fungal stain identifies the narrow-based budding yeast in tissue [1].
Our patient improved during antifungal therapy with amphotericin B, but finally succumbed as a result of hospital-acquired pneumonia due to Klebsiella pneumoniae. It remains unknown whether earlier recognition and initiation of specific antimicrobial therapy would have improved the patient survival, as a result of shorter length of ICU stay. The most important prognostic factor for success in the treatment of cryptococcosis remains the nature of underlying immunosuppression and the ability to control the patients’ primary disease [1].
In conclusion, cryptococcal infection should be added to the differential diagnosis of epididymo-orchitis and cellulitis in immunocompromised hosts. We stress the vital importance of a correct diagnosis, which requires a biopsy with proper histopathology and culture. Early diagnosis and therapy are essential if the case-fatality rates associated with disseminated infection are to be improved.
Conflict of Interest
The authors declare that they have no conflict of interest.
| References | ▴Top |
- Mitchell TG, Perfect JR. Cryptococcosis in the era of AIDS—100 years after the discovery of Cryptococcus neoformans. Clin Microbiol Rev. 1995;8(4):515-548.
pubmed - Pappas PG, Perfect JR, Cloud GA, Larsen RA, Pankey GA, Lancaster DJ, Henderson H, et al. Cryptococcosis in human immunodeficiency virus-negative patients in the era of effective azole therapy. Clin Infect Dis. 2001;33(5):690-699.
doi pubmed - Anderson DJ, Schmidt C, Goodman J, Pomeroy C. Cryptococcal disease presenting as cellulitis. Clin Infect Dis. 1992;14(3):666-672.
doi pubmed - Shrader SK, Watts JC, Dancik JA, Band JD. Disseminated cryptococcosis presenting as cellulitis with necrotizing vasculitis. J Clin Microbiol. 1986;24(5):860-862.
pubmed - Mayers DL, Martone WJ, Mandell GL. Cutaneous cryptococcosis mimicking gram-positive cellulitis in a renal transplant patient. South Med J. 1981;74(8):1032-1033.
doi pubmed - Mamo GJ, Rivero MA, Jacobs SC. Cryptococcal prostatic abscess associated with the acquired immunodeficiency syndrome. J Urol. 1992;148(3):889-890.
pubmed - James CL, Lomax-Smith JD. Cryptococcal epididymo-orchitis complicating steroid therapy for relapsing polychondritis. Pathology. 1991;23(3):256-258.
doi pubmed - Kiertiburanakul S, Wirojtananugoon S, Pracharktam R, Sungkanuparph S. Cryptococcosis in human immunodeficiency virus-negative patients. Int J Infect Dis. 2006;10(1):72-78.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


