| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 5, May 2013, pages 327-329
Signet Ring Cell Carcinoma of the Duodenal Bulb With Metastases to the Ovaries and the Colon: A Case Report
Josia N Henrya, b, c, Belen Tesfayea, b, Freaw Dejeniea, Sara Hortona, Adeyinka Layiemoa
aHoward University Hospital, 2041 Georgia Avenue, Washington DC, 20060, USA
bFirst authors
cCorresponding author: Josia N Henry, Howard University Hospital, 2041 Georgia Avenue, Washington DC, 20060, USA
Manuscript accepted for publication March 21, 2013
Short title: Duodenal Bulb to Ovaries and Colon
doi: https://doi.org/10.4021/jmc1223w
| Abstract | ▴Top |
Primary duodenal cancer is a rare entity which has accounted for only 0.3% of all gastrointestinal cancers. The majority of duodenal bulb cancers are adenocarcinomas and other histological variants are less frequent. Signet ring cell carcinoma, though more commonly found in the stomach, is uncommonly found to originate in the duodenal bulb. A review of the literature revealed only one previously reported cases of signet ring cell carcinoma of the duodenal bulb. We report a rare case of signet call carcinoma of the duodenal bulb with metastasis to the ovaries, peritoneum, and colon in a 25-year-old Hispanic female. She presented with abdominal pain, ascites, nausea and jaundice. Subsequent imaging studies revealed an adnexal mass and upper endoscopy revealed an exophytic obstructing duodenal bulb mass, biopsy consistent with signet ring carcinoma. Etiology and survival of signet ring cell carcinoma of the duodenal bulb is not well-defined in the literature due to the extreme rarity of this disease. Continued reporting of this rare entity will help in characterizing the natural history of the disease, which may allow for earlier recognition and treatment.
Keywords: Signet ring; Duodenal bulb; Carcinoma
| Introduction | ▴Top |
Signet-ring cell carcinoma (SRC) is uncommon in the small intestine, colon and rectum, with a reported incidence ranging from 0.1% to 0.9% [1, 2]. Although > 96% of SRCs occur in the stomach, the rest arise in other organs, including the breast, gallbladder, pancreas, urinary bladder, and large bowel [3]. Since the first description of SRC by Laufman and Saphir [4], the incidence of SRC has become 0.6/100,000 individuals [5]. The incidence continues to slowly increase with improvements in diagnostic capabilities. Unfortunately cases detected and treated at early stages are rare. Clinical symptoms usually appear late and, signet-ring cell carcinomas are commonly detected at advanced stages. In this case report, we present our experience with a signet-ring cell carcinoma of the duodenal bulb with metastasis to the colon and ovary detected at a late stage in a 25-year-old Hispanic female along with a review the literature.
| Case Report | ▴Top |
A 25-year-old Hispanic female was admitted to the Howard University Hospital with four weeks complaint of epigastric, peri-umbilical pain, nausea, vomiting, early satiety and ten pound weight loss. The patient also reported a two day history of jaundice. Past medical history included pancreatitis and a history of recently diagnosed ovarian mass. She had a family history significant for a cousin diagnosed with leukemia. The patient denied tobacco, alcohol or any illicit drug use. On physical examination, the patient was found to have icterus, bilateral cervical adenopathy more prominent on the left, and bilateral lower quadrant tenderness. Pelvic examination revealed a ballottable right adnexal mass.
Laboratory study results showed a total bilirubin of 19.0 mg/dL with a conjugated picture, aspartate aminotransferase and alanine aminotransferase levels of 131 and 116 MU/ML, respectively (normal < 55 MU/ML) and alkaline phosphatase 914 MU/ML (normal 30 - 165 MU/ML). Amylase and lipase were 354 U/L and 468 U/L respectively (normal 28 - 100 and 22 - 51 U/L). Hemoglobin levels during admission ranged between 8 - 10 g/dL (normal 12 - 15 g/dl).Tumor markers obtained revealed an elevated cancer antigen-125(CA-125) at 458 U/mL (normal < 20 U/mL), cancer antigen 19-9 (CA 19-9 526), carcinoembryonic antigen (CEA) 85 ng/mL (normal < 2.5 ng/mL) and alpha fetoprotein level of 55.8 ng/mL (normal < 6.1 ng/mL).
Abdominal ultrasonography demonstrated moderately diffuse ascites, mild hepatomegaly with moderately diffuse heterogeneity of the parenchyma without evidence of a solid mass. There was extra-hepatic ductal dilatation without evidence of intrahepatic ductal dilatation. Transvaginal ultrasound demonstrated an enlarged right ovary. Subsequent computerized tomography of abdomen and pelvis confirmed moderate ascites, a diffusely heterogenous liver with numerous ill-defined foci. Bilateral heterogeneous adnexal masses with the largest being on the right measuring 5.5 × 4.0 cm were observed. A heterogeneous large kidney with decreased function was noted. There was small to moderate diffuse adenopathy.
Ultrasound guided core needle biopsy of the right adnexal mass revealed poorly differentiated mucin producing adenocarcinoma with focal signet ring features (Fig. 1). Immunostains revealed expression of CK7, CK20 and CDX2 which suggested a site of origin in the upper gastrointestinal tract (Fig. 2). Bidirectional endoscopy was then performed. Upper endoscopy revealed an exophytic mass lesion extending from the duodenal bulb and obstructing distally appearing to involve the ampulla and causing jaundice (Fig. 3). No obvious mass was noted in the stomach. Colonoscopy revealed multiple masses in the ascending, transverse, descending and sigmoid colon the largest being a 5 cm exophytic lesion. There was no evidence of familial adenomatous polyposis. Biopsy of these lesions also revealed poorly differentiated adenocarcinoma with focal signet ring features displaying lymphatic invasion (Fig. 4).
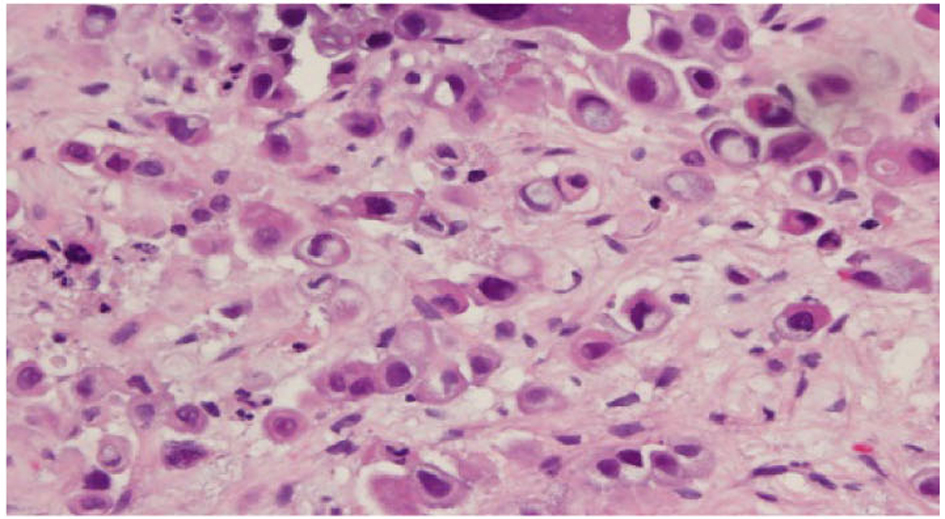 Click for large image | Figure 1. Right adnexal mass biopsy illustrating signet ring cells. |
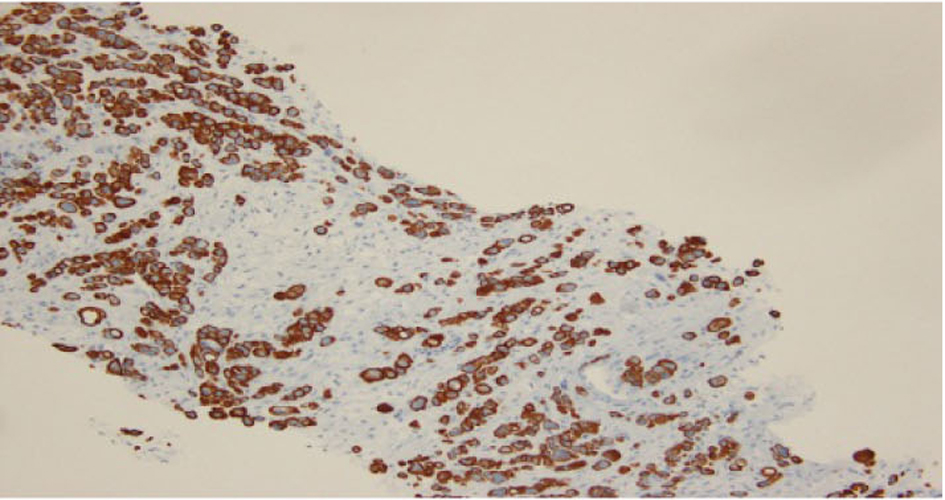 Click for large image | Figure 2. Immunostains of adnexal mass expression of CK7, CK20 and CDX2. |
 Click for large image | Figure 3. Exophytic mass arising from duodenal bulb. |
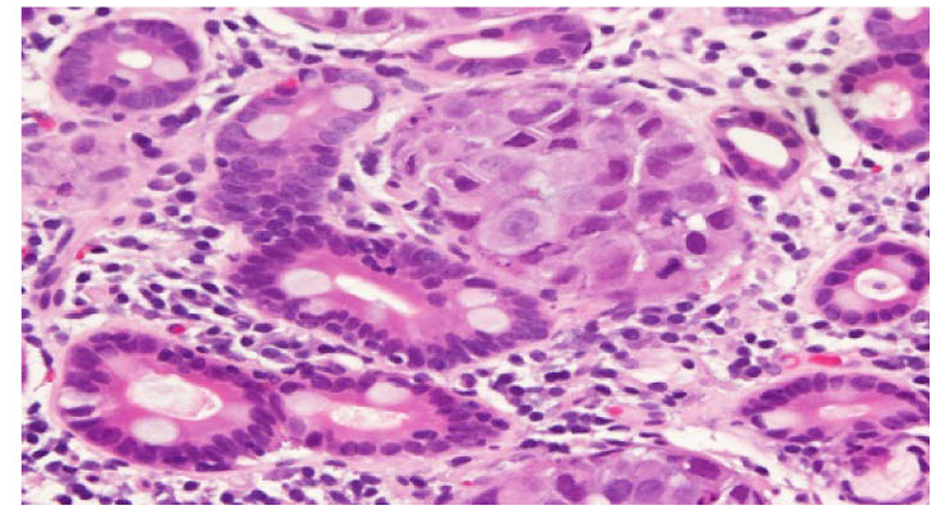 Click for large image | Figure 4. Duodenal mass biopsy illustrating focal signet ring features. |
Medical oncology was consulted and palliative care measures were recommended. Chemotherapy was not recommended secondary to the patient’s overall poor performance status and significantly elevated liver tests. Biliary stenting and ureteral stenting was suggested for palliation. Unfortunately, the patient died before within a few days of admission.
| Discussion | ▴Top |
Signet ring carcinoma of the duodenum was first described by Sekoguchi et al in 1979 [6]. Histologically, the origin of signet-ring cells remains unknown. One theory regarding the etiology is that the signet cells are thought to originate in ectopic gastric mucosa found in the duodenum. Another theory is that the signet ring cell carcinoma arises from gastric type metaplastic epithelia. These metaplastic changes are considered to be a protective response to acid production and can usually be seen in the duodenal bulb [7]. In our case the endoscopy revealed a mass extending from the duodenal bulb and obstructing the ampulla. This was histologically consistent with poorly differentiated signet ring cell adenocarcinoma.
Signet ring cell tumors generally carry a poor prognosis regardless of site of origin with greater that 80% of SRC diagnoses present with advanced (stage III or IV) disease [8, 9].
Duodenal cancers commonly occur in the ampullary or periampullary regions of the descending duodenum [10]; however, these tumors are occasionally found in other portions of the duodenum [11]. If caught early, the preferred treatment for resectable lesions in the second and third portions of the duodenum is a pancreaticoduodenectomy with en bloc resection of adjacent tissues, including regional lymph nodes [12].
The most frequent clinical findings of duodenal cancer include epigastric pain, nausea, vomiting, postprandial bloating, weight loss. There can be signs of upper gastrointestinal bleeding, such as guaiac-positive stool and iron-deficiency anemia [10, 11, 13].
Unfortunately, most symptomatic patients with duodenal cancer have advanced lesions at presentation. As a result, these patients have a poor prognosis, with overall 5-year survival rates ranging from 20% to 40% [10, 11, 12]. Factors affecting patient survival include the histologic grade of the tumor (the degree of differentiation and the nuclear grade), depth of invasion, presence or absence of nodal or distant metastases, duration of symptoms, and location of tumor in the duodenum (distal lesions have a better prognosis) [11].
Ovarian metastases occur in about 3% of all CRC patients and make up between 5% and 10% of all CRC metastases. The best known tumor of this type is the signet-ring adenocarcinoma (Krukenburg tumor) of gastric origin [14]. Carcinomas of the colon, appendix and breast are the next most common site of origin. This case is unique in that the small intestine (duodenal bulb) is not a frequent site of origin of Krukenburg tumor.
The limited number of cases of signet cell cancer reported in the duodenal bulb precludes any conclusions about survival associated with this histological variant.
Conflict of Interests
The authors declare no conflict of interests.
| References | ▴Top |
- Giacchero A, Aste H, Baracchini P, Conio M, Fulcheri E, Lapertosa G, Tanzi R. Primary signet-ring carcinoma of the large bowel. Report of nine cases. Cancer. 1985;56(11):2723-2726.
doi - Almagro UA. Primary signet-ring carcinoma of the colon. Cancer. 1983;52(8):1453-1457.
doi - Tung SY, Wu CS, Chen PC. Primary signet ring cell carcinoma of colorectum: an age- and sex-matched controlled study. Am J Gastroenterol. 1996;91(10):2195-2199.
pubmed - Laufman H, Saphir O. Primary linitis plastica type of carcinoma of the colon. AMA Arch Surg. 1951;62(1):79-91.
doi - Kang H, O'Connell JB, Maggard MA, Sack J, Ko CY. A 10-year outcomes evaluation of mucinous and signet-ring cell carcinoma of the colon and rectum. Dis Colon Rectum. 2005;48(6):1161-1168.
doi pubmed - Sekoguchi T, Mizumoto R. Clinicopathological study of papilla of Vater. Geka Chiryo 1979; 41:1-5.
- Hoedemaeker PJ. Heterotopic gastric mucosa in the duodenum. Digestion. 1970;3(3):165-173.
doi pubmed - Nissan A, Guillem JG, Paty PB, Wong WD, Cohen AM. Signet-ring cell carcinoma of the colon and rectum: a matched control study. Dis Colon Rectum. 1999;42(9):1176-1180.
doi pubmed - Psathakis D, Schiedeck TH, Krug F, Oevermann E, Kujath P, Bruch HP. Ordinary colorectal adenocarcinoma vs. primary colorectal signet-ring cell carcinoma: study matched for age, gender, grade, and stage. Dis Colon Rectum. 1999;42(12):1618-1625.
doi pubmed - Fenoglio-Preiser CM, Pascal RR, Perzin KH. Tumors of the intestines. In:Atlas of tumor pathology, 2nd series, fascicle 27. Washington, DC: Armed Forces Institute of Pathology, 1990: 175-250.
- Delcore R, Thomas JH, Forster J, Hermreck AS. Improving resectability and survival in patients with primary duodenal carcinoma. Am J Surg. 1993;166(6):626-630; discussion 630-621.
- Rose DM, Hochwald SN, Klimstra DS, Brennan MF. Primary duodenal adenocarcinoma: a ten-year experience with 79 patients. J Am Coll Surg. 1996;183(2):89-96.
pubmed - Levine MS. Benign tumors. In: Gore RM, Levine MS, Laufer I, eds. Textbook of gastrointestinal radiology. Philadelphia: Saunders, 1994:628 -659.
- Lashgari M, Behmaram B, Hoffman JS, Garcia J. Primary biliary carcinoma with metastasis to the ovary. Gynecol Oncol. 1992;47(2):272-274.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


