| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 5, May 2013, pages 349-352
Listeria Brain Abscess in a Patient With Crescentic Glomerulonephritis That Progressed to Chronic Kidney Disease: A Case Report
Yuh Ming Changa, Chang Phone Fungb, Yang Kai Fanc, Cheng Yin Tsengd, e
aDepartment of Neurology, Hsinchu Mackay Memorial Hospital, Hsinchu City, Taiwan
bDivision of Infectious Diseases, Department of Medicine, Taipei Veterans General Hospital (TPVGH) and National Yang-Ming University, Taipei, Taiwan
cDepartment of Radiology, Hsinchu Mackay Memorial Hospital, Hsinchu City, Taiwan
dDivision of Infectious Diseases, Department of Internal Medicine, Hsinchu Mackay Memorial Hospital, Hsinchu City, Taiwan
eCorresponding author: Cheng-Yin Tseng, Division of Infectious Diseases, Department of Internal Medicine, Hsinchu Mackay Memorial Hospital, No. 690, Section 2, Guangfu Road, Hsinchu City 30071, Taiwan
Manuscript accepted for publication March 19, 2013
Short title: Listeria Brain Abscess Associated With CKD
doi: https://doi.org/10.4021/jmc1253e
| Abstract | ▴Top |
Listeria monocytogenes is a gram-positive opportunistic intracellular pathogen that causes listeriosis, a rare but serious foodborne illness. Listeriosis has a predilection to invade the central nervous system and is associated with high mortality. L. monocytogenes commonly causes meningitis, and brain abscesses are rare. Among the ones reported thus far, most Listeria brain abscess occur in patients with underlying hematological malignancies or in those receiving solid organ transplants. Listeria brain abscess in a patient with crescentic glomerulonephritis, however, has not yet been reported. Here, we report a case of Listeria brain abscess with intraventricular rupture causing ventriculitis and hydrocephalus in a 61-year-old man with crescentic glomerulonephritis that progressed to chronic kidney disease.
Keywords: Brain abscess; Central nervous system infections; Hydrocephalus; Listeria monocytogenes; Listeriosis
| Introduction | ▴Top |
Listeria monocytogenes, an opportunistic intracellular pathogen, is the causative agent of listeriosis, a rare but serious systemic infection. Listeriosis can be clinically divided into noninvasive and invasive forms. Invasive listeriosis usually develops in patients with impaired cell-mediated immunity [1], while noninvasive listeriosis is either asymptomatic or presents as acute self-limited febrile gastroenteritis in immunocompromised hosts [2].
Invasive listeriosis has a wide clinical spectrum. It exhibits central nervous system (CNS)-specific tropism and is associated with high mortality [3]. Meningitis is the most common symptom of CNS listeriosis, while brain abscess is rare [3]. Most cases of Listeria brain abscess occur in patients with underlying hematological malignancies or in those receiving solid organ transplants [4-6]. To date, only 70 cases of Listeria brain abscess have been reported in the literature [7].
To the best of our knowledge, Listeria brain abscess in patients with crescentic glomerulonephritis has not been previously reported. Here, we report a case of Listeria brain abscess with intraventricular rupture causing ventriculitis and hydrocephalus in a 61-year-old man with crescentic glomerulonephritis that progressed to chronic kidney disease.
| Case Report | ▴Top |
A 61-year-old man was admitted to the emergency department of our hospital because of intermittent fever, shaking chills, and progressive lethargy since the past 4 days. He had developed bloody stools 4 days before admission owing to consumption of a substantial amount of refrigerated foods several days before disease onset. Two years ago, he had biopsy-proven crescentic glomerulonephritis that progressed to chronic kidney disease stage V, requiring hemodialysis. The patient discontinued dialysis after 8 months because his renal function improved with methylprednisolone pulse therapy and maintenance therapy with 20 mg prednisolone/day. Approximately 12 h after arrival, the patient developed shaking chills and high fever (38.7 °C) again. Two sets of blood samples were collected. Initial physical examination was noncontributory. His initial laboratory tests revealed leukocytosis (white blood cell (WBC) count, 13,400/mm3) with neutrophil predominance (neutrophils, 93%; lymphocytes, 4%; and monocytes, 3%), low hemoglobin level (8.7 g/dL), and impaired renal function (blood urea nitrogen, 147 mg/dL and creatinine, 5.0 mg/dL). His chest radiograph was unremarkable. Upper gastrointestinal endoscopy revealed superficial gastritis with no signs of recent bleeding. Sigmoidoscopy up to 15 cm was normal. The fever subsided after the administration of an antipyretic, and the patient was referred to the Gastroenterology clinic from the emergency department on the same day.
Three days later, he was re-admitted to the emergency department because of fever (38.3 °C), chills, and lethargy. Because L. monocytogenes was isolated from the 2 sets of blood cultures collected during his first visit, ampicillin with renal dose adjustment (2 g every 12 h) plus gentamicin (60 mg every 24 h) were administered parenterally, and the patient was then admitted to the medical ward.
On arrival, his blood pressure, pulse, respiratory rate, and temperature were 183/90 mmHg, 100 beats/min, 20 breaths/min, and 37.8 °C, respectively. His conjunctivae were pale with anicteric sclera. His neck was supple without jugular venous engorgement, bruits, or lymphadenopathy. He had a regular heart rate without murmur. Lung auscultation revealed no wheezing or rales. His abdomen was soft with normal active bowel sounds, while the liver and spleen were not palpable. On neurological examination, he was alert and well oriented. His higher cortical function and cranial nerve and motor system examination were normal. Deep tendon reflexes were equal and plantar reflexes were flexor. Sensory examination and coordination were normal as well.
The next morning, however, our patient went into a coma. Brain computed tomography (CT) without contrast revealed a hypodensity with perifocal edema in the left frontal lobe, a communicating hydrocephalus with pressure, and fluid-fluid levels in the dependent portion of the occipital horns (Fig. 1). Brain abscess with intraventricular rupture causing ventriculitis and hydrocephalus was highly suspected. Urgent external ventricular drainage was recommended by emergent neurosurgery consultation, owing to a rapid decline in the patient’s mental status. The cerebrospinal fluid (CSF) was found to be slightly turbid in appearance and under high pressure during surgery. Ventricular CSF analysis revealed pleocytosis (WBC count, 115 cells/mL) with neutrophil predominance (neutrophils, 78%; lymphocytes, 22%) and red blood cells (622 cells/mL). The CSF protein concentration was elevated (321 mg/dL; reference range 10 - 45 mg/dL), and the CSF glucose concentration was 55 mg/dL (simultaneous blood glucose level was 204 mg/dL). CSF gram staining and cultures were negative. On day 3 after admission, our patient’s blood pressure dropped and despite management, his condition continued to deteriorate and he eventually died on day 4.
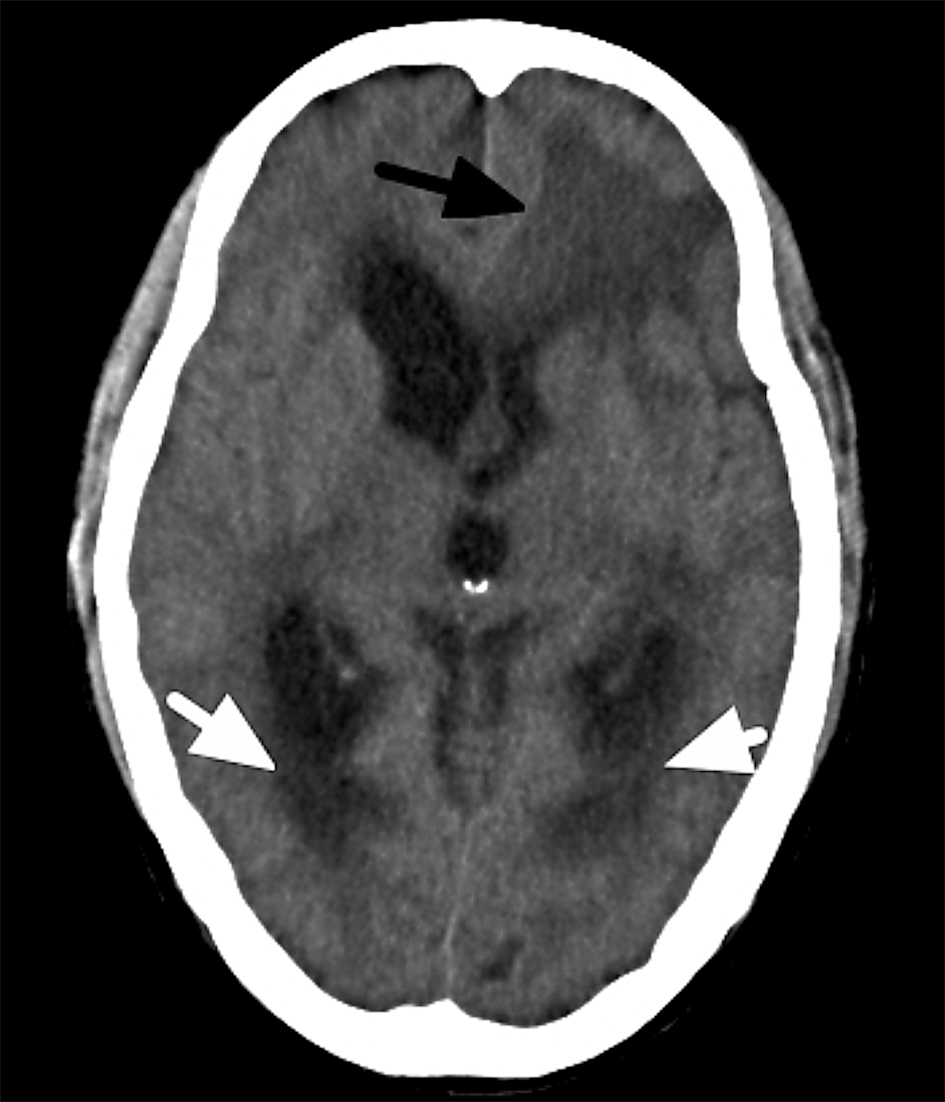 Click for large image | Figure 1. Axial non-contrast brain computed tomography scan of our patient revealed a hypodensity with perifocal edema in the left frontal lobe (black arrow), a communicating hydrocephalus with pressure, and fluid-fluid levels in the dependent portion of occipital horns (white arrows). |
| Discussion | ▴Top |
In retrospect, long-term steroid use in our patient suppressed his cell-mediated immunity and increased his susceptibility to listeriosis [8]. In our patient, the steroids may have masked the symptoms and signs of Listeria, delaying its diagnosis.
L. monocytogenes is a gram-positive rod that has been recognized as an emerging foodborne pathogen since the 1980s [9]. Its main mode of transmission is contaminated food. After entering the host via the gastrointestinal tract, L. monocytogenes can survive and spread intracellularly without extracellular exposure to humoral immunity [10]. Thus, cell-mediated immunity is the host’s primary defense mechanism against L. monocytogenes infection.
Invasive listeriosis most frequently presents as primary bacteremia, CNS infections, maternal-fetal/neonatal infections, or localized infections [3]. Meningitis is the most common form of CNS listeriosis, while rhombencephalitis [11] and brain abscess are rarely detected.
Brain abscess occurs in approximately 10% cases of CNS listeriosis [4-6]. Most cases of Listeria brain abscess occur in patients with underlying hematological malignancies or in those receiving solid organ transplants [4-6]. Listeria brain abscesses are usually single and located in the frontal and/or parietal lobe. Involvement of the subcortical gray matter has been observed in one-fifth of the affected patients [4]. Listeria brain abscess is associated with positive blood culture in 85% patients and concomitant meningitis in nearly 25% patients [4, 5]. The high rate of positive blood culture suggests that the pathogenesis of Listeria brain abscess is secondary to spread [4].
Axial non-contrast brain CT of our patient revealed a hypodensity with perifocal edema in the left frontal lobe, a communicating hydrocephalus with pressure, and fluid-fluid levels in the dependent portion of the occipital horns (Fig. 1). The most likely differential diagnoses could be brain abscess with intraventricular rupture, primary or metastatic tumor with subacute or old hemorrhage, and resolving hematoma. Although brain contrast-enhanced magnetic resonance imaging (MRI) is more sensitive in lesion differentiation, this modality could not be applied to our patient because of his rapid clinical deterioration and severe renal dysfunction. However, the differential diagnoses could be narrowed down based on the clinical course, positive blood cultures, ventricular CSF study, and location of the lesion, making Listeria brain abscess with intraventricular rupture causing ventriculitis and hydrocephalus the most likely diagnosis. Even though gram staining of the CSF and CSF bacterial culture were negative in our patient, Al-Khatti et al diagnosis of Listeria brain abscess, presenting with frontal hypodensity on the initial brain CT scan, in which the pathogen was isolated only from the blood cultures drawn at the time of admission, supports our diagnosis [12].
Our patient acquired L. monocytogenes probably by consumption of refrigerated foods several days before disease onset, and developed bloody stool. Although diarrhea associated with Listeria gastroenteritis is usually non-bloody, bloody diarrhea has been reported in 3% patients [2]. Listeria gastroenteritis is self-limiting in most cases; however, invasive listeriosis can occur if bacteremia presents. The factors determining the transformation of self-limiting listeriosis to the fatal invasive form include virulence factors produced by the pathogen, number of pathogens ingested, and host immunity [2].
The incidence of listeriosis in Taiwan remains unknown. Recently, 2 retrospective single-center studies in Taiwan reported that the incidence of listeriosis has increased from 2005 to 2008 [13, 14]. Although the main reason for this increase remains unclear, most affected patients had predisposing factors that lowered their immunity, such as malignancy, renal failure, and type II diabetes mellitus.
The treatment choice for Listeria brain abscess is high-dose ampicillin (2 g every 4 h) for at least 6 - 8 weeks and serial monitoring by MRI or CT [4-6]. Gentamicin was administered in our case for its synergic effect. For patients allergic to penicillin, trimethoprim/sulfamethoxazole is the drug of choice. Third-generation cephalosporins are ineffective against L. monocytogenes. Surgical drainage had been indicated if the abscess is > 2.5 cm or is located in the deep brain matter, and it can facilitate correct identification of the infectious pathogen [4]. Although ventricular drainage with intravenous and/or intrathecal antibiotics are recommended in ruptured brain abscess with hydrocephalus and ventriculitis [15], no definitive therapeutic regimens for intraventricular rupture of Listeria brain abscess have been reported in the literature.
In conclusion, Listeria brain abscess in patients with crescentic glomerulonephritis is uncommon, and long-term steroid treatment in such patients may increase the risk of opportunistic infections. The prognosis of Listeria brain abscess is poor with intraventricular rupture. Early diagnosis in patients undergoing long-term immunosuppression therapy is challenging. Thus, clinicians should consider the possibility of CNS listeriosis in patients presenting with rapidly progressing CNS manifestations that appear after acute gastrointestinal illness, and should provide adequate antibiotic therapy.
Declaration
The authors have no conflicts of interest to declare.
| References | ▴Top |
- Bortolussi R. Listeriosis: a primer. CMAJ. 2008;179(8):795-797.
doi pubmed - Ooi ST, Lorber B. Gastroenteritis due to Listeria monocytogenes. Clin Infect Dis. 2005;40(9):1327-1332.
doi pubmed - Drevets DA, Bronze MS. Listeria monocytogenes: epidemiology, human disease, and mechanisms of brain invasion. FEMS Immunol Med Microbiol. 2008;53(2):151-165.
doi pubmed - Eckburg PB, Montoya JG, Vosti KL. Brain abscess due to Listeria monocytogenes: five cases and a review of the literature. Medicine (Baltimore). 2001;80(4):223-235.
doi - Cone LA, Leung MM, Byrd RG, Annunziata GM, Lam RY, Herman BK. Multiple cerebral abscesses because of Listeria monocytogenes: three case reports and a literature review of supratentorial listerial brain abscess(es). Surg Neurol. 2003;59(4):320-328.
doi - Soares-Fernandes JP, Beleza P, Cerqueira JJ, Ribeiro M, Mare R, Lourenco E, Rocha JF. Simultaneous supratentorial and brainstem abscesses due to Listeria monocytogenes. J Neuroradiol. 2008;35(3):173-176.
doi pubmed - Coste JF, Duval V, Nguyen Y, Guillard T, Brasme L, David C, Strady C, et al. [Unusual location of a brain abscess due to Listeria monocytogenes]. Pathol Biol (Paris). 2012;60(5):e45-48.
doi pubmed - Klein NC, Go CH, Cunha BA. Infections associated with steroid use. Infect Dis Clin North Am. 2001;15(2):423-432, viii.
doi - Disson O, Lecuit M. Targeting of the central nervous system by Listeria monocytogenes. Virulence. 2012;3(2):213-221.
doi pubmed - Freitag NE, Port GC, Miner MD. Listeria monocytogenes - from saprophyte to intracellular pathogen. Nat Rev Microbiol. 2009;7(9):623-628.
doi pubmed - Armstrong RW, Fung PC. Brainstem encephalitis (rhombencephalitis) due to Listeria monocytogenes: case report and review. Clin Infect Dis. 1993;16(5):689-702.
doi - Al-Khatti AA, Al-Tawfiq JA. Listeria monocytogenes brain abscess in a patient with multiple myeloma. J Infect Dev Ctries. 2010;4(12):849-851.
pubmed - Huang YT, Liao CH, Yang CJ, Teng LJ, Wang JT, Hsueh PR. Listeriosis, Taiwan, 1996-2008. Emerg Infect Dis. 2011;17(9):1731-1733.
doi pubmed - Huang SL, Chou YT, Hsieh YC, Huang YC, Lin TY, Chiu CH. Epidemiology and clinical characteristics of Listeria monocytogenes bacteremia in a Taiwanese medical center. J Microbiol Immunol Infect. 2010;43(6):485-490.
doi - Takeshita M, Kawamata T, Izawa M, Hori T. Prodromal signs and clinical factors influencing outcome in patients with intraventricular rupture of purulent brain abscess. Neurosurgery. 2001;48(2):310-316; discussion 316-317.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


