| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 8, August 2013, pages 517-518
Unexplained Catastrophic Systemic Neutrophilic Syndrome in a 68-Year-Old Man: A Severe Variant of Aseptic Abscesses or a New Entity?
Gilles Safaa, d, Lisa Rousseaua, Laure Darrieuxa, Daniel Robertb, Dominique Boutrouxc
aDepartment of Dermatology, Centre Hospitalier de Saint-Brieuc, Saint-Brieuc, France
bDepartment of Hematology, Centre Hospitalier de Saint-Brieuc, Saint-Brieuc, France
cDepartment of Gastroenterology, Centre Hospitalier de Saint-Brieuc, Saint-Brieuc, France
dCorresponding author: Gilles Safa, Department of Dermatology, Centre Hospitalier de Saint-Brieuc, 10, rue Marcel Proust, 22000 Saint-Brieuc, France
Manuscript accepted for publication June 6, 2013
Short title: Catastrophic Systemic Neutrophilic Syndrome
doi: https://doi.org/10.4021/jmc1347w
| Abstract | ▴Top |
We report for the first time the case of a 68-year-old man with unexplained catastrophic systemic neutrophilic syndrome without abscesses. Although this case shares some features with autoinflammatory disorders, such as aseptic abscesses syndrome, including recurrent fever, leukocytosis, anemia, and elevated acute phase proteins, it is unique for the absence of deep abscess-like collections, the presence of high procalcitonin levels without infection, and a rapidly progressive, ultimately fatal condition despite aggressive therapies with high-dose corticosteroids and interleukin 1 receptor blockade with anakinra. We believe that this case presents unique characteristic features among autoinflammatory diseases. Further studies are needed to fully recognize this distinct clinical entity and clarify the role of neutrophil-derived cytokines in the pathogenic mechanisms of this life-threatening condition for the development of new treatment strategies.
Keywords: Auto-inflammatory syndrome; Neutrophilic disease; Polymorphonuclear neutrophil
| Introduction | ▴Top |
Aseptic abscesses (AA) syndrome is a rare but emerging entity within autoinflammatory disorders that is characterized by intra-abdominal aseptic collections consisting of neutrophils and is associated with fever, leukocytosis, and elevated blood markers of inflammation. Antibiotic treatment provides no improvement, but AA is highly sensitive to corticosteroids [1]. Herein we describe for the first time the case of a 68-year-old man with unexplained catastrophic systemic neutrophilic syndrome without abscesses who was unresponsive to multiple treatments and discuss the potential relationship with AA syndrome.
| Case Report | ▴Top |
A 68-year-old Caucasian man was admitted to the hospital for a 4-week history of recurrent attacks of high-grade fever (39 - 40 °C), poor general condition, and weight loss. His past medical history was significant for atopic eczema treated with methotrexate (20 mg weekly). On admission, there were no characteristic physical findings. The patient’s hemodynamic status was normal. Laboratory examinations showed marked leukocytosis, with neutrophilia reaching 51,770/mm3 (normal 1,800 - 7,500), anemia (hemoglobin level of 9.6 g/dL (normal 13 - 17)), an erythrocyte sedimentation rate (ESR) of 101 mm/hr (normal < 20), a serum C-reactive protein (CRP) level of 232 mg/L (normal < 10), and a procalcitonin level of 4.89 µg/L (normal < 0.1). Renal function and liver enzymes were normal. Autoantibodies, including antinuclear antibodies, antineutrophil cytoplasmic antibody, rheumatoid factor, and anti-Saccharomyces cerevisiae antibody, were negative. An exhaustive search for viral, bacterial, fungal, mycobacterial, and parasitic infections was negative. Empiric treatment with broad-spectrum antibiotics, including ceftriaxone, amoxicillin/clavulanate, and metronidazole, associated with antifungal therapy (fluconazole) and intravenous acyclovir was unsuccessful. Bone marrow aspiration and biopsy failed to disclose an underlying hematologic malignancy. The patient was negative for the Janus kinase 2 (Jak2) V617F mutation. A whole-body computed tomography scan showed hepatomegaly and splenomegaly, without abscesses (Fig. 1). Esogastroduodenoscopy and colonoscopy were normal. Fluorodeoxyglucose (FDG)-positron emission tomography scan showed intense FDG uptake in the liver and spleen, with no other localization. Histological analysis of a liver biopsy showed sterile polymorphonuclear leukocyte infiltration without collections (Fig. 2). A diagnosis of unexplained catastrophic systemic neutrophilic syndrome was considered. The patient was treated with intravenous pulses of methylprednisolone 1,000 mg per day for 3 days, followed by oral prednisone 1 mg/kg/day. The fever disappeared, but biological abnormalities (elevated CRP and ESR and raised leukocyte count) were still present. Because of progressive deterioration of the patient’s condition, off-label therapy with the interleukin 1 (IL-1) receptor antagonist anakinra (Kineret®, 100 mg/day subcutaneously) was administered. Despite initial stabilization, the patient’s condition worsened, and he subsequently died of multiorgan failure.
 Click for large image | Figure 1. Abdominal computed tomography scan showing hepatosplenomegaly without abscesses. |
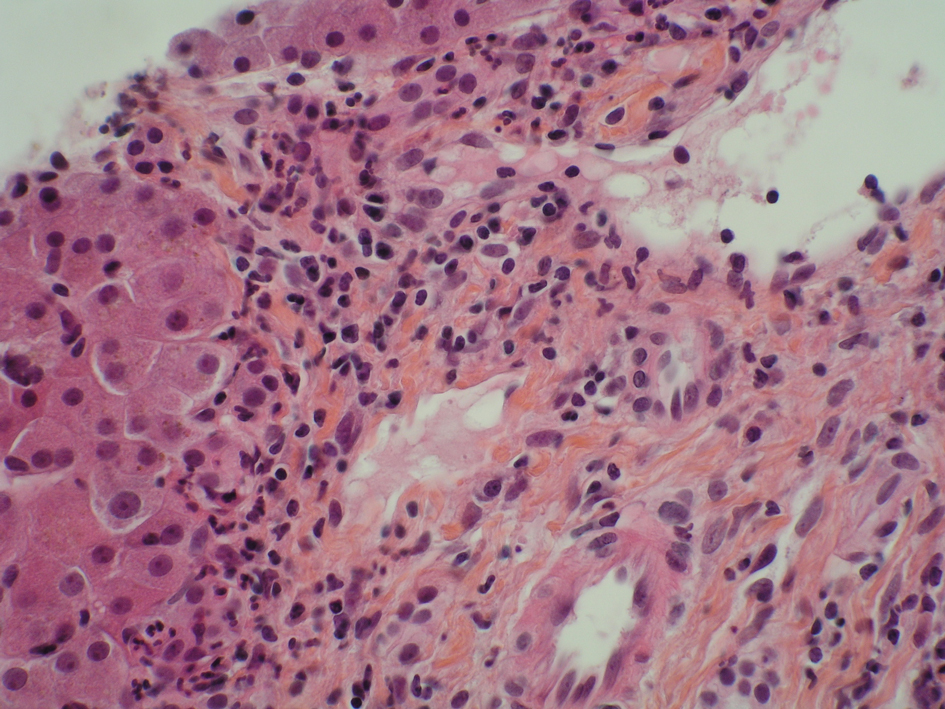 Click for large image | Figure 2. Liver biopsy specimen showing prominent portal infiltration by neutrophils (hematoxyline-eosin, 40 ×). |
| Discussion | ▴Top |
AA syndrome is a systemic disorder of unknown etiology involving polymorphonuclear neutrophils. There is a strong association of AA with inflammatory bowel diseases and neutrophilic dermatoses, which suggests both genetic susceptibility and a relationship with autoinflammatory disorders [2]. Although this case shares some features with autoinflammatory disorders, such as AA syndrome, including recurrent fever, leukocytosis, anemia, and elevated acute phase proteins, it is unique for the absence of deep abscess-like collections, the presence of high procalcitonin levels without infection, and a rapidly progressive, ultimately fatal condition despite aggressive therapies with high-dose corticosteroids and IL-1 receptor blockade with anakinra. Autoinflammation is characterized by dysregulation of the innate immune system and neutrophils play a prominent role in the clinical manifestations seen in several of the autoinflammatory disorders [3]. A growing number of systemic autoinflammatory diseases are linked to IL-1 activity because rapid and sustained resolution is observed upon specific blockade of the IL-1 receptor [4]. In this case, blocking IL-1 was unsuccessful.
We believe that this case presents unique characteristic features among autoinflammatory diseases, and we introduce the term catastrophic systemic neutrophilic syndrome to describe this clinical entity. Further studies are needed to fully recognize this distinct clinical entity and clarify the role of neutrophil-derived cytokines and chemokines in the pathogenic mechanisms of this life-threatening condition for the development of new treatment strategies.
Competing Interests
The authors declare that they have no competing interests.
| References | ▴Top |
- Andre MF, Piette JC, Kemeny JL, Ninet J, Jego P, Delevaux I, Wechsler B, et al. Aseptic abscesses: a study of 30 patients with or without inflammatory bowel disease and review of the literature. Medicine (Baltimore). 2007;86(3):145-161.
doi pubmed - Andre M, Aumaitre O, Papo T, Kemeny JL, Vital-Durand D, Rousset H, Ninet J, et al. Disseminated aseptic abscesses associated with Crohn's disease: a new entity? Dig Dis Sci. 1998;43(2):420-428.
doi pubmed - Ferguson PJ, Lokuta MA, El-Shanti HI, Muhle L, Bing X, Huttenlocher A. Neutrophil dysfunction in a family with a SAPHO syndrome-like phenotype. Arthritis Rheum. 2008;58(10):3264-3269.
doi pubmed - Dinarello CA. Blocking IL-1 in systemic inflammation. J Exp Med. 2005;201(9):1355-1359.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


