| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 8, August 2013, pages 557-559
Anti-Myelin Associated Glycoprotein Polyneuropathy in a Patient With Lymphoma and its Resolution After Chemotherapy
Nisar Ahmada, c, Sajjad Haidera, Muzaffar Jameela, Zainab Shahida, Marwan Yaredb, Saad Z Usmania
aMyeloma Institute for Research & Therapy, University of Arkansas for Medical Sciences, Little Rock, Arkansas, USA
bDepartment of Pathology, University of Arkansas for Medical Sciences, Little Rock, Arkansas, USA
cCorresponding author: Nisar Ahmad, Myeloma Institute for Research & Therapy, University of Arkansas for Medical Sciences, 4301 W Markham Street slot 816, Little Rock, AR, 72205, USA
Manuscript accepted for publication July 5, 2013
Short title: Anti-mag Polyneuropathy in Lymphoma
doi: https://doi.org/10.4021/jmc1399w
| Abstract | ▴Top |
Anti-myelin associated glycoprotein (anti-MAG) antibody associated polyneuropathy is a chronic distal symmetric sensorimotor neuropathy. The rarity of this condition precludes establishment of a standard of care. It has been treated with steroids, intravenous immunoglobulin (IVIG) and Rituximab. We present a case of a 72 years old man presenting with 1 year history of neuropathic pain in lower extremities and hands bilaterally, right cervical lymphadenopathy on physical exam, and the anti-MAG antibody ELISA was positive. An excisional biopsy of the cervical lymph node showed diffuse large B cell lymphoma. The staging bone marrow examination did not show lymphoma involvement, the PET/CT did only demonstrated neck and mediastinal lymphadenopathy. The patient received four cycles of R-CHOP (Rituximab, Cyclophosphamide, Doxorubicin, Vincristine and Prednisone) for Stage IIA disease with complete response, and complete resolution of polyneuropathy after the first cycle of chemotherapy. The case report highlights the successful treatment of a rare presentation of anti-MAG polyneuropathy associated with early stage diffuse large B-cell lymphoma.
Keywords: Anti-MAG antibody; Polyneuropathy; Lymphoma
| Introduction | ▴Top |
The estimated prevalence of this neuropathy in the population older than 50 years is at least 30 per 100,000 [1, 2]. Lymphoma can affect the peripheral nervous system in 5% of patients [3]. Peripheral neuropathy (PN) is however an uncommon presenting symptom in patients with lymphomas. Non-Hodgkin's lymphoma (NHL) is more often associated with PN than other lymphoproliferative disorders [4]. Neuropathy in lymphoma may be due to direct infiltration of nerves, paraneoplastic mechanisms, or related to metabolic and infectious processes. More than 50% of patients with neuropathy-associated IgM monoclonal gammopathy possess antibodies against MAG [5]. Anti-MAG antibody associated PN is however rare in hematological malignancies and presents a diagnostic and therapeutic challenge [6]. Detection of IgM autoantibody against myelin associated glycoprotein (MAG) suggests active demyelination in peripheral neuropathy. We present a case of anti-MAG antibody associated sensory peripheral neuropathy in a patient with diffuse large B-cell lymphoma which resolved after chemotherapy.
| Case Report | ▴Top |
A 72-year old male was referred to our center with a one year history of progressively worsening tingling, numbness and pain in both lower extremities in an ascending fashion. His past medical history was significant for hypertension, GERD and diverticulitis. Interestingly, he had two older sisters with history of Non-Hodgkin’s Lymphoma. He initially presented to his primary care physician with 3 months history of numbness in his lower extremities and was managed conservatively without any relief. Four months later, the patient had developed the neuropathy symptoms in both his arms as well. He had lost 25 pounds during this time. He was referred to a local oncologist and underwent a thorough workup including complete blood counts, comprehensive chemistry panel, thyroid functions, serum protein electrophoresis-immunofixation (SPEP-IF), serum vitamin B12 levels and serum folic acid levels revealing normal values except an IgM kappa monoclonal gammopathy. A fat pad biopsy for amyloid was negative. The patient underwent a nerve conduction study consistent with mild sensory and motor polyneuropathy in both upper and lower without evidence of demyelination.
The patient was then seen at our center in light of the IgM monoclonal gammopathy. He was found to have right cervical lymphadenopathy on physical exam. Additional laboratory work-up including cold agglutinins, serum cryoglobulins, serologies for HIV, hepatitis B, Hepatitis C, West Niles virus, Chaga’s disease, and cytomegalovirus was conducted and was unremarkable. Serum zinc and copper levels were also found to be within normal range. A bone marrow biopsy was negative for underlying plasma or B cell disorder. A PET scan demonstrated large intense hypermetabolic soft tissue mass involving the right oropharynx and right tongue base measuring about 2.7 cm (standard uptake value of 13.2) associated with right cervical and submandibular as well as supraclavicular and pretracheal lymph node positivity. Biopsies of the tonsillar mass as well as cervical lymph node excision were performed. The pathology revealed a non-germinal center cell type diffuse large B-cell lymphoma, positive for CD20, CD79a, PAX-5, MUM-1, BCL-6, BCL-2, and CD23 (Fig. 1, 2). The anti-MAG antibody ELISA was abnormal with a value of 167 TU.
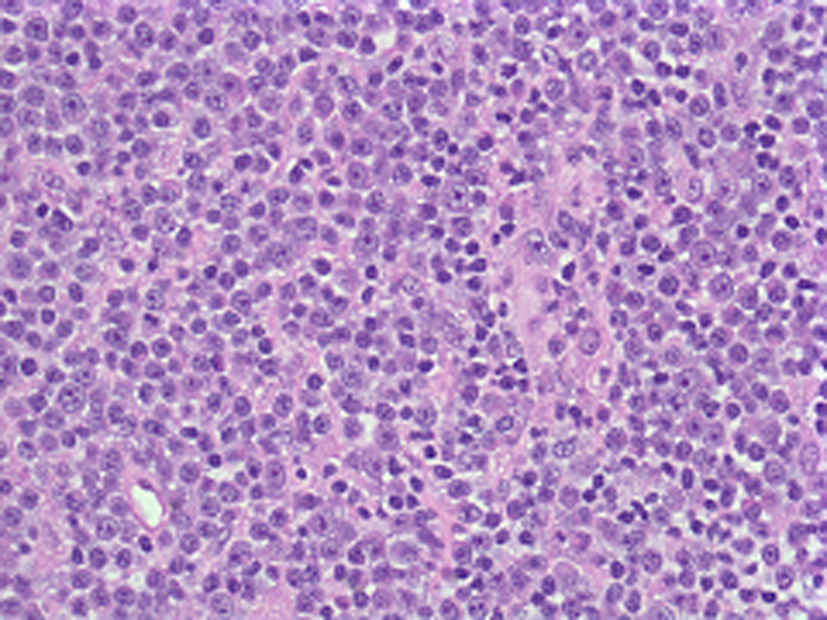 Click for large image | Figure 1. Lymph node biopsy: atypical lymphoid cells. |
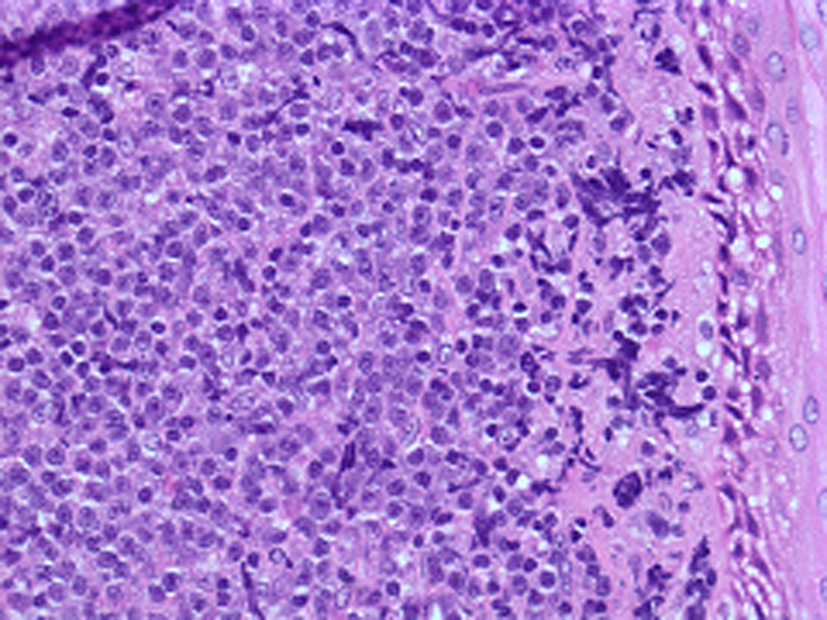 Click for large image | Figure 2. Tonsil biopsy (atypical lymphocytes with peripheral nucleoli). |
The patient was deemed to have Stage IIA diffuse large B-cell lymphoma and initiated on treatment with R-CHOP chemotherapy with resolution of neuropathy symptoms and PET avid lymphadenopathy after the two cycles of treatment.
| Discussion | ▴Top |
Neuropathy associated with anti-MAG antibody is a chronic distal symmetric sensorimotor neuropathy [7]. It has been reported with IgM monoclonal gammopathy and rarely with hematological malignancies. MAG is a schwan cell-based glycoprotein and has been implicated to influence the cytoskeleton integrity of aoxns. The electrophysiological findings in anti-MAG neuropathy indicate a demyelinating neuropathy [7]. It is clinically manifested as sensory ataxia, impaired gait and mild to moderate distal muscle weakness in advanced cases. Sural nerve biopsy typically shows a diminished number of myelinated axons and loss of large myelinating fibers. Nerve conduction studies demonstrate distal demyelination with prolongation of distal motor and sensory latencies.
Diagnosis of anti MAG neuropathy requires a high clinical suspicion based on symptoms, a distal demyelination on nerve conduction studies and a positive anti-MAG antibody titer by ELISA. A recent study in a large number of samples has confirmed that ELISA testing for MAG is more sensitive than Western blotting [8]. Anti-MAG neuropathy remains a therapeutic challenge. It has been treated with immune-modulating therapies that include intravenous immunoglobulin, chlorambucil, and plasma exchange, interferon-alpha with inconsistent or non-beneficial effects in placebo-controlled trials. These treatments have limited long-term efficacy and are associated with significant morbidity [9-11]. Rituximab therapy on the other hand has shown encouraging results in few case reports and clinical trials and may be the treatment of choice at present [12-14].
Conclusion
It is important to differentiate anti-MAG PN from other forms of chronic inflammatory neuropathies and search for underlying etiology. Anti-MAG polyneuropathy has distinctive clinical, electrophysiological, and pathological features that may help distinguish it from chronic inflammatory demyelinating polyneuropathy and other IgM-related neuropathies [15]. Identifying and treating the underlying etiology of symptoms is extremely important. Our Patient presented with symptomatic PN etiology of which was unclear at presentation and he had gradual progression of the symptoms. His PN symptoms resolved with treatment of the underlying lymphoma.
| References | ▴Top |
- Nobile-Orazio E. Antigenic determinants in IgMparaprotein-related neuropathies. Clin Lymphoma Myeloma. 2009;9(1):107-109.
doi pubmed - Ropper AH, Gorson KC. Neuropathies associated with paraproteinemia. N Engl J Med. 1998;338(22):1601-1607.
doi pubmed - Hughes RA, Britton T, Richards M. Effects of lymphoma on the peripheral nervous system. J R Soc Med. 1994;87(9):526-530.
pubmed - Kelly JJ, Karcher DS. Lymphoma and peripheral neuropathy: a clinical review. Muscle Nerve. 2005;31(3):301-313.
doi pubmed - Latov N. Pathogenesis and therapy of neuropathies associated with monoclonal gammopathies. Ann Neurol. 1995;37(Suppl 1):S32-42.
doi pubmed - Marfia GA, Pachatz C, Terracciano C, Leone G, Bernardini S, Bernardi G, Massa R. Subacute demyelinating polyneuropathy in B-cell lymphoma with IgM antibodies against glycolipid GD1b. Neurol Sci. 2005;26(5):355-357.
doi pubmed - Launay M, Delmont E, Benaim C, Sacconi S, Butori C, Desnuelle C. [Anti-MAG paraproteinemic demyelinating polyneuropathy: a clinical, biological, electrophysiological and anatomopathological descriptive study of a 13-patients' cohort]. Rev Neurol (Paris). 2009;165(12):1071-1079.
doi pubmed - Kuijf ML, Eurelings M, Tio-Gillen AP, van Doorn PA, van den Berg LH, Hooijkaas H, Stork J, et al. Detection of anti-MAG antibodies in polyneuropathy associated with IgM monoclonal gammopathy. Neurology. 2009;73(9):688-695.
doi pubmed - Notermans NC, Lokhorst HM, Franssen H, Van der Graaf Y, Teunissen LL, Jennekens FG, Van den Berg LH, et al. Intermittent cyclophosphamide and prednisone treatment of polyneuropathy associated with monoclonal gammopathy of undetermined significance. Neurology. 1996;47(5):1227-1233.
doi pubmed - Mariette X, Chastang C, Clavelou P, Louboutin JP, Leger JM, Brouet JC. A randomised clinical trial comparing interferon-alpha and intravenous immunoglobulin in polyneuropathy associated with monoclonal IgM. The IgM-associated Polyneuropathy Study Group.J NeurolNeurosurg Psychiatry. 1997;63(1):28-34.
doi pubmed - Gorson KC, Ropper AH, Weinberg DH, Weinstein R. Treatment experience in patients with anti-myelin-associated glycoprotein neuropathy. Muscle Nerve. 2001;24(6):778-786.
doi pubmed - Steck AJ, Stalder AK, Renaud S. Anti-myelin-associated glycoprotein neuropathy. Curr Opin Neurol. 2006;19(5):458-463.
doi - Renaud S, Fuhr P, Gregor M, Schweikert K, Lorenz D, Daniels C, Deuschl G, et al. High-dose rituximab and anti-MAG-associated polyneuropathy. Neurology. 2006;66(5):742-744.
doi pubmed - Renaud S, Gregor M, Fuhr P, Lorenz D, Deuschl G, Gratwohl A, Steck AJ. Rituximab in the treatment of polyneuropathy associated with anti-MAG antibodies. Muscle Nerve. 2003;27(5):611-615.
doi pubmed - Cocito D, Durelli L, Isoardo G. Different clinical, electrophysiological and immunological features of CIDP associated with paraproteinaemia. ActaNeurol Scand. 2003;108(4):274-280.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


