| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 9, September 2013, pages 633-635
Intra-Abdominal Haemorrhage due to Traumatic Rupture of a Hepatic Cyst and Parenchymal Cystic Wall Laceration Following Blunt Abdominal Injury
Tsukasa Nakamuraa, c, Shumpei Haradaa, Toshimasa Nakaoa, Koji Masudab, Yoshio Osakab, Hirotaka Sakob, Norio Yoshimuraa
aDepartment of Transplant and General Surgery, Kyoto Prefectural University of Medicine, address: Kajii-cho 465, Kamigyo-ku, Kyoto- prefecture, Japan
bDepartment of Surgery, Omihachiman Medical Community Center, address: Tsuchida-cho 1379, Omihachiman-city, Shiga-prefecture, 523-0082, Japan
cCorresponding author: Tsukasa Nakamura, Department of Transplant and General Surgery, Kyoto Prefectural University of Medicine, Kajii-cho 465, Kamigyo-ku, Kyoto- prefecture, 602-8566, Japan
Manuscript accepted for publication August 5, 2013
Short title: Traumatic Liver Surgery
doi: https://doi.org/10.4021/jmc1429w
| Abstract | ▴Top |
Intra-abdominal haemorrhage due to traumatic rupture of a hepatic cyst is sometimes fatal. Rupture of a hepatic cyst without bleeding does not necessarily need any surgical intervention or vice versa. However, a ruptured hepatic cyst accompanied by parenchymal hepatic laceration potentially leads patients to a lethal status, because of delayed intra abdominal haemorrhage. Furthermore, the patient was under warfarin therapy and even small lacerations may lead to significant bleeding and subsequent laparotomies. Therefore, close observation is important for patients whose hepatic cyst is ruptured, albeit without any signs of simultaneous haemorrhage on arrival. This is the case of an 87-year-old woman who had a road traffic accident and whose hepatic cyst was ruptured without simultaneous haemorrhage. The following morning, she demonstrated haemorrhagic shock. A subsequent CT scan revealed intra abdominal haemorrhage, and bleeding from the biggest hepatic cyst. Immediately, she underwent emergency surgery under the pringle manoeuvre, inferior vena cava (IVC) total clamping, and venovenous bypass (VVB) from the femoral vein to the internal jugular vein. The patient soon became systemically well. Generally, occlusion of hepatic inflow and infra hepatic IVC are crucial for control of hepatic and behind hepatic IVC bleeding. Furthermore, in order to avoid instability due to IVC total clamping, it is important to execute VVB especially for pulmonary hypertension or cardiomyopathy patients.
Keywords: Blunt liver injury; Intra abdominal haemorrhage; Hepatic cyst; Rupture
| Introduction | ▴Top |
The frequency of hepatic cysts in the general population is estimated to be 1.6% to 3.6% [1]. Mostly they are asymptomatic, but complications may occur due to obstructive jaundice, rupture, intracystic haemorrhage, and infection. Among these complications, clinicians should be well aware of our case which demonstrated intra abdominal haemorrhage due to traumatic rupture of a hepatic cyst and parenchymal cystic wall laceration.
| Case Report | ▴Top |
An 87-year-old woman presented at our emergency room due to a road traffic accident, with stable vital signs. Physical examination was unremarkable relating to the traffic accident at that moment, albeit with high energy trauma. Her past medical history was pulmonary hypertension, chronic atrial fibrillation, chronic heart failure, and surgery for an atrial septal defect. Her medication included warfarin and diuretics. Hematologic studies showed Haemoglobin (HgB) of 9.8 g/dL, Platelet count of 190,000/µL, and Prothrombin time of (PT sec) 29.3 sec (INR: 2.56). CT scan revealed multiple liver cysts and traumatic rupture of some cysts larger than 10 cm, albeit without any signs of simultaneous intra abdominal haemorrhage (Fig. 1a). She was hospitalised for close observation by an emergency department doctor, because she had a high energy injury and her Prothrombin time was prolonged due to warfarin medication. However, there were no efforts to reverse the effects of warfarin by an aggressive management (such as fresh frozen plasma or vitamin K etc.). The following morning, about 18 hours after admission, she demonstrated severe anaemia: HgB 6.8 g/dL, hypotension, and tachycardia. Subsequent CT scan revealed intra abdominal haemorrhage, and bleeding from the biggest hepatic cyst (Fig. 1b). Then, the patient was referred to our surgery department. Immediately, she underwent emergency surgery under pringle manoeuvre, inferior vena cava (IVC) total clamping, and venovenous bypass (VVB) from the femoral vein to the internal jugular vein. Although the total amount of intra abdominal haemorrhage was up to 2,500 mL prior to surgery, haemorrhage during surgery with the above methods was only a small amount. Haemostasis was obtained firmly with burning and suturing the parenchymal laceration during a total of 12 minutes’ vascular exclusion and the cystic wall was open-roofed. Consequently, the patient became systemically well without any signs of haemorrhage.
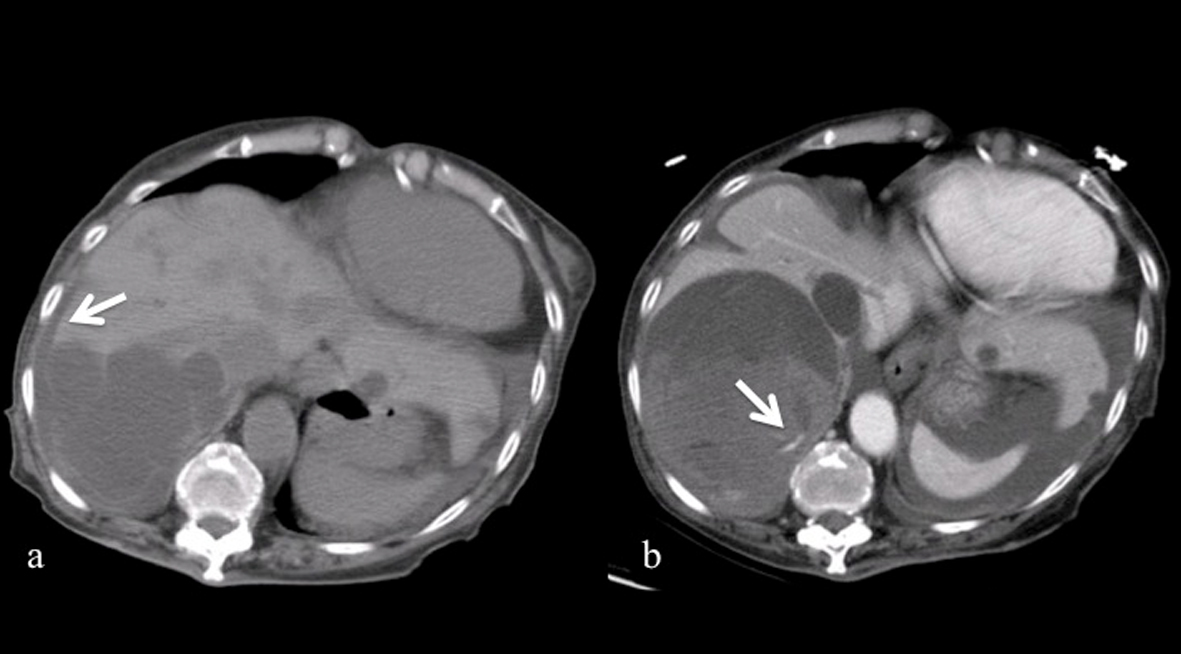 Click for large image | Figure 1. a). Multiple hepatic cysts over the posterior aspect of the right lobe of the liver. Some of the hepatic cysts walls were ruptured and free peritoneal fluid was present (White arrow). b). Extravasation was clearly seen on the enhanced CT scan (White arrow), and some extent of tamponade effect may be observed. |
| Discussion | ▴Top |
Generally, a large amount of intra abdominal haemorrhages and suspicions of multiple organ injuries are common indications for an emergency laparotomy, including damage control surgery. Haemostasis effect due to tamponade effect [2] might prevent a parenchymal cystic wall laceration from problematic bleeding. However, a laceration which is accompanied with rupture of a hepatic cyst increases the risk of intra abdominal bleeding. The incidence of rupture has not been reported clearly, but reported ruptured hepatic cysts tend to be larger than 10 cm [3]. Furthermore, the usage of warfarin clearly had been responsible for the severe intra abdominal haemorrhage of our patient. In this case, only CT scan on arrival revealed the rupture of some of the hepatic cysts, but did not reveal any bleeding at that time. Close observation, however, must be applied on the assumption that it might develop later into lethal intra abdominal haemorrhage. In the case of emergency surgery, immediate occlusion of hepatic inflow and infra hepatic IVC are crucial for the control of hepatic or behind liver IVC bleeding. Furthermore, total hepatic vascular exclusion (THVE) also may be helpful for this type of surgery. Therefore, surgical and anaesthetic technique of liver transplantation can be applied for traumatic liver surgery. In order to avoid hemodynamic instability due to IVC total clamping, it is useful to execute VVB especially for pulmonary hypertension, heart failure, ischemic heart disease, or cardiomyopathy patients [4, 5]. From the aspects of theoretical and evidenced physiology, advantages of VVB also include: Reducing over excessive fluid loading; Maintaining renal function [6]. Although, 1.5 - 5.0 L/min shunt flows have been described in cases of liver transplantation [7-9], it has been pointed out that ideal normalised haemodynamic state and renal perfusion during IVC cross-clamping can be obtained where shunt flows should be greater than 3.0 L/min [10]. Considering our case, the shunt flow was up to 0.5 L/min, because of the limitation in utilising larger catheters. However, it is reasonable to assume that it was effective to maintain her stable haemodynamic state.
Emergency haemostatic surgery was performed safely for a patient who demonstrated intra abdominal haemorrhage from a ruptured hepatic cyst following a blunt abdominal injury. It is of vital importance to maintain hemodynamic stability while performing emergency haemostatic surgery. At the same time, over-transfusion should be avoided in order to prevent post-operative pulmonary oedema and ascites. It is clear, therefore, that VVB seems to be useful for traumatic liver surgery with pringle manoeuvre and IVC clamping, especially for patients who demonstrate pulmonary hypertension or cardiomyopathy. Needless to say, it is important to maintain an adequate level of PT INR. As a result of this report we would like to make clinicians, surgeons and anaesthetists, who might deal with blunt liver injury, more aware of delayed significant bleeding due to liver laceration, traumatic liver surgery and techniques of liver transplantation. When recognised and managed appropriately it will lead to improved survival rates.
Conflict of Interest Statement
None.
Funding
None.
| References | ▴Top |
- Caremani M, Vincenti A, Benci A, Sassoli S, Tacconi D. Ecographic epidemiology of non-parasitic hepatic cysts. J Clin Ultrasound. 1993;21(2):115-118.
doi pubmed - Zanen AL, van Tilburg AJ. Bleeding into a liver cyst can be treated conservatively. Eur J Gastroenterol Hepatol. 1995;7(1):91-93.
pubmed - Yamaguchi M, Kuzume M, Matsumoto T, Matsumiya A, Nakano H, Kumada K. Spontaneous rupture of a nonparasitic liver cyst complicated by intracystic hemorrhage. J Gastroenterol. 1999;34(5):645-648.
doi pubmed - Gifford DJ. Support perfusion for liver transplantation. Perfusion. 1991;6(3):203-208.
doi pubmed - Beltran J, Taura P, Grande L, Garcia-Valdecasas JC, Rimola A, Cugat E. Venovenous bypass and liver transplantation. Anesth Analg. 1993;77(3):642.
doi pubmed - Grande L, Rimola A, Cugat E, Alvarez L, Garcia-Valdecasas JC, Taura P, Beltran J, et al. Effect of venovenous bypass on perioperative renal function in liver transplantation: results of a randomized, controlled trial. Hepatology. 1996;23(6):1418-1428.
doi pubmed - Shaw BW, Jr., Martin DJ, Marquez JM, Kang YG, Bugbee AC, Jr., Iwatsuki S, Griffith BP, et al. Venous bypass in clinical liver transplantation. Ann Surg. 1984;200(4):524-534.
doi pubmed - Paulsen AW, Whitten CW, Ramsay MA, Klintmalm GB. Considerations for anesthetic management during veno-venous bypass in adult hepatic transplantation. Anesth Analg. 1989;68(4):489-496.
doi pubmed - Wall WJ, Grant DR, Duff JH, Kutt JL, Ghent CN. Blood transfusion requirements and renal function in patients undergoing liver transplantation without venous bypass. Transplant Proc. 1987;19(Suppl 3):4 17-20.
pubmed - Scherer RU, Giebler RM, Schmutzler MJ, Gunnicker FM, Kox WJ. Shunt flow and caval pressure gradient during veno-venous bypass in human orthotopic liver transplantation. Br J Anaesth. 1993;70(6):689-690.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


