| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 11, November 2013, pages 742-745
Sudden Sensorineural Hearing Loss After Laparoscopic Cholecystectomy Under General Anesthesia
Seong Pyo Muna, Sung Il Chob, c
aDepartment of Surgery, Chosun University School of Medicine, South Korea
bDepartment of Otolayngology-Head and Neck Surgery, Chosun University School of Medicine, South Korea
cCorresponding author: Sung Il Cho, Department of Otolaryngology-Head and Neck Surgery, Chosun University Hospital, 365 Pilmun-daero, Dong-gu, Gwangju 501-717, South Korea
Manuscript accepted for publication October 2, 2013
Short title: Sudden Hearing Loss After Cholecystectomy
doi: https://doi.org/10.4021/jmc1512w
| Abstract | ▴Top |
Sudden sensorineural hearing loss is infrequent, but it is considered an otologic emergency. Although multiple etiologies have been identified, idiopathic sudden sensorineural hearing loss is most common. Sudden sensorineural hearing loss following non-otologic surgery under general anesthesia is an extremely rare complication. A 55-year-old man presented with hearing loss, tinnitus in his right ear, which developed right after laparoscopic cholecystectomy. Pure tone audiogram showed profound sensorineural hearing loss in the right ear. Treatment included intravenous prednisolone, intratympanic dexamethasone, vasodilator and carbogen inhalation. The patient had improved hearing and resolution of tinnitus. This report represents the first documented case of unilateral sudden sensorineural hearing loss after laparoscopic cholecystectomy under general anesthesia.
Keywords: Hearing loss; Sensorineural; Cholecystectomy; Sudden
| Introduction | ▴Top |
Sudden sensorineural hearing loss (SNHL) is an otologic emergency and quite unusual after nonotologic surgery. Most occurrences reported in patients after cardiopulmonary bypass with an incidence of one in 1,000 cases [1]. On the contrary, there has been no report of sudden SNHL after cholecystectomy under general anesthesia in the English literature. We present a case of unilateral sudden SNHL after laparoscopic cholecystectomy under general anesthesia, and review the relevant literature.
| Case report | ▴Top |
A 55-year-old man had an asymptomatic mass in the gallbladder which was incidentally found at regular check-up. He denied anorexia, nausea, dysphagia, diarrhea. He had a past medical history of an uncomplicated appendectomy for acute appendicitis and no history of prior ear surgery or other medical problems. There were no reports of complication from previous general anesthesia. He had not taken any ototoxic drugs. Preoperative physical examination and laboratory studies were unremarkable. Propofol and fentanyl had been used for induction. General anesthesia was maintained with a mixture of oxygen and desflurane. The patient subsequently underwent laparoscopic cholecystectomy. There were no surgical complications. The procedure lasted for about one and half hours, and blood loss was minimal. No episode of hypotension was observed. Pathology revealed cholesterol polyp. On awakening the patient noted an acute hearing loss in the right ear with tinnitus but denied ear fullness and vertigo. Physical examination for the tympanic membrane, external auditory canal was normal. A tuning fork test indicated that Weber lateralized to the left side. Audiogram showed profound right deafness across the entire frequency (Fig. 1). On the left side, mild SNHL was documented. Hearing loss in the left ear was believed to be the patient’s preoperative baseline. The laboratory exams were within the normal range. The neurological and cardiovascular examinations revealed no pathological findings. To investigate the lesion of internal auditory canal and cerebellopontine angle, a magnetic resonance imaging (MRI) scan of the head was done. MRI revealed no tumor and other abnormalities. The patient was treated with high-dose steroid, intravenous prednisolone daily for 7 days, followed by progressive tapering of dose. There was no improvement of hearing loss by 7 days. Therefore, the patient was given a right ear intratympanic injection of dexamethasone. Additionally, carbogen inhalation was done. On the second week, the patient noted improvement in hearing and tinnitus. Complete recovery and resolution of tinnitus were achieved after 2 months (Fig. 2). During follow-up of 12 months, no recurrence was found.
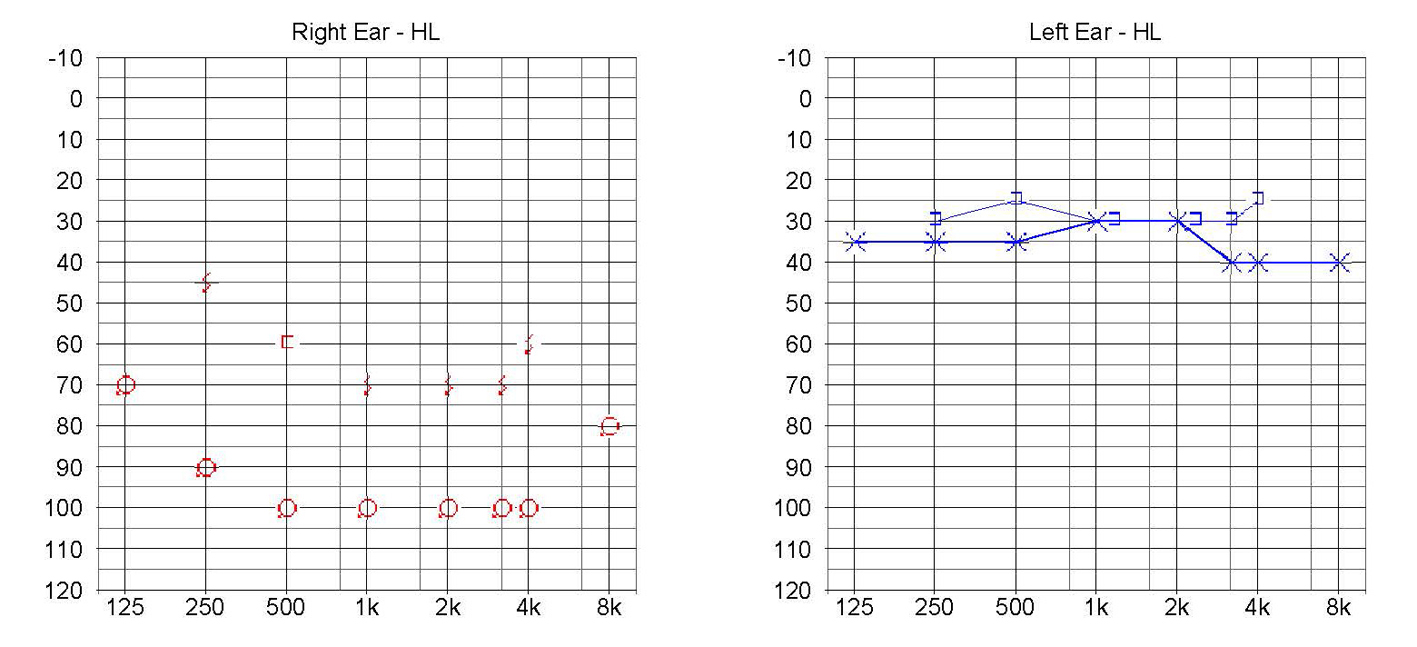 Click for large image | Figure 1. Initial audiogram. Profound deafness across the entire frequency range is seen on the right ear, while on the left side, mild SNHL is seen. Upper line represents bone conduction and lower line represents air conduction. |
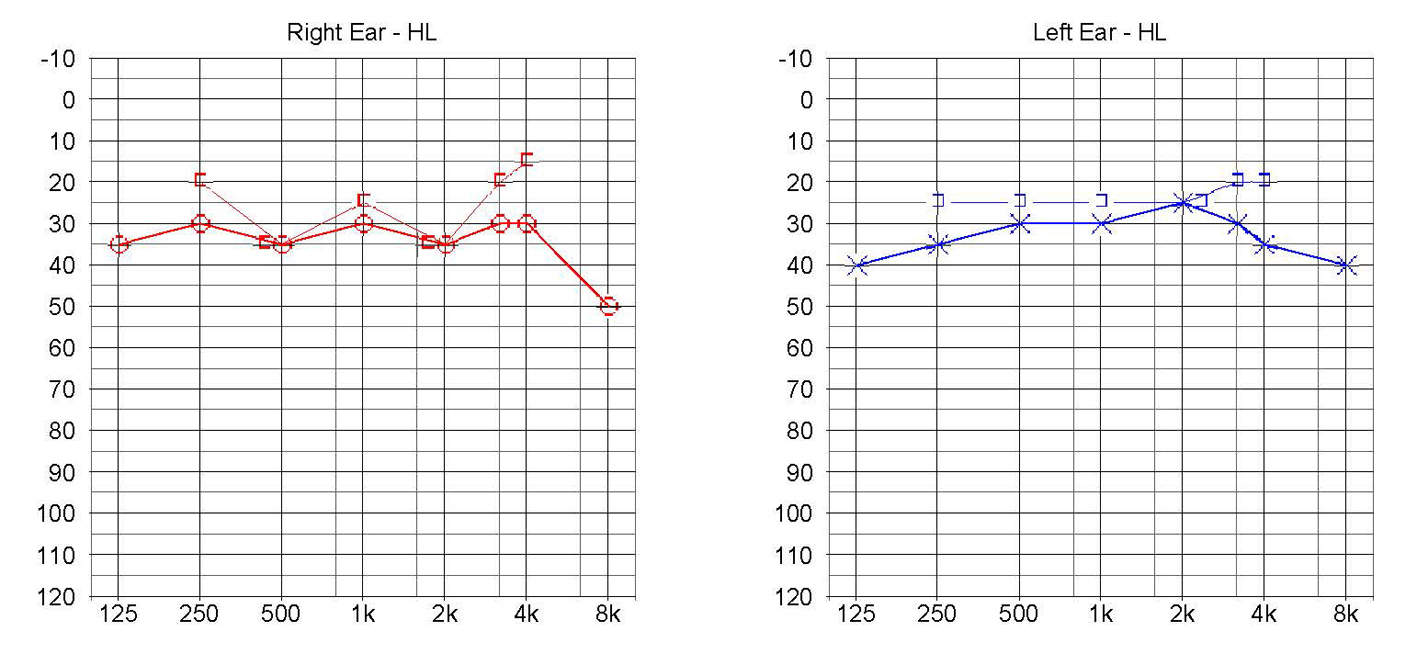 Click for large image | Figure 2. Audiogram at 2-month follow-up. Complete recovery is seen compared with the left ear. Upper line represents bone conduction and lower line represents air conduction. |
| Discussion | ▴Top |
Sudden SNHL is defined as a rapid onset, occurring over a 72-hour period, of a subjective sensation of hearing impairment in one of both ears. It is considered an otologic emergency because early diagnosis and treatment may result in a favourable outcome [2, 3]. The most frequently used audiometric criterion is a decrease in hearing of ≥ 30 decibels (dB), affecting at least 3 consecutive frequencies. Because premorbid audiometry is generally unavailable, hearing loss is defined as related to the opposite ear’s thresholds [3]. In most cases it is unilateral and is accompanied by tinnitus and sometimes by vertigo. The etiologic factors of sudden SNHL can be recognized infections, autoimmune diseases, traumatic damages, vascular causes, acoustic neuroma, multiple sclerosis or it may be idiopathic [4]. Sudden SNHL after nonotologic surgery has been seldom reported. Most postoperative non-otologic cases of sudden SNHL occur in patients with cardiopulmonary bypass [1, 5]. For patients who have undergone nonotologic surgery under general anesthesia, the recognition of a specific cause may be difficult. The most likely etiology was microemboli, particulate matter, fat, or calcium deposits from calcified heart valve. Microemboli could generate from the cardiopulmonary pump or particles of arteriosclerotic plaques and occlude the cochlear branch of the internal auditory artery [6, 7]. Several reports also suggested that microembolic phenomenon is the etiology for SNHL after general anesthesia in nonbypass surgery. Microembolisms have been typically associated with unilateral hearing loss and can cause ischemia of the stria vascularis and hair cells, which result in hearing impairment [8, 9].
The use of nitrous oxide (NO) during general anesthesia is also one of proposed causal factors for postoperative SNHL. NO enters enclosed cavities such as the middle ear, and can increase middle ear pressure. This causes disruption of the cochlear membrane with resulting SNHL [10]. The increase middle ear pressure can be maintained for 45 minutes after discontinuation of NO [2]. Another potential cause is sustained high upper airway pressures which are required to break an episode of laryngospasm during general anesthesia. Sustained high positive pressures may force open the Eustachian tube, transmitting them to the middle ear [11]. In addition, some anesthetic agents such as profopol or fentanyl can cause hemodynamic instability with perioperative hypotension and subsequently reduce blood supply to the cochlea causing hearing loss. Other etiologic factors include hypercoagulable states and vasospasm [4].
In this patient, NO and high positive pressures was not applied during general anesthesia. However, drugs such as propofol and fentanyl used for induction could be possible causes of transient vertebrobasilar hypoperfusion producing cochlear injury resulting in hearing loss.
In addition, cholecystectomy might result in liberation of microemboli which could occlude the cochlear division of the internal auditory artery, subsequently result in a hearing loss. It is more likely to explain unilateral hearing loss of the present case.
Treatment options include systemic and intratympanic steroids, hyperbaric oxygen, vasodilators, plasma expanders, carbogen (5% carbon dioxide and 95% oxygen) inhalation. Steroids, used in the present patient, reduce the inflammatory effect and endolymphatic pressure. Hyperbaric oxygen, vasodilators, and plasma expanders improve blood circulation. Inhaled carbogen improves the blood supply in the perilymph [2-4]. If the patient has partial or no hearing recovery, hearing aid and other supportive measures are indicated. The mainstay of treatment is usually based on corticosteroid administration regardless of the initiating cause of SNHL. Corticosteroid is initial therapy and the treatment appears to offer the greatest recovery in the first 2 weeks, with little benefit after 4 to 6 weeks. For maximal treatment outcomes, recommended treatment doses of prednisolone are given at 1 mg/kg per day with the usual maximum dose of 60 mg daily, and treatment duration of 7 to 14 days, and then taper over similar time period [3]. A more recent method of corticosteroid delivery is the intratympanic route. Intratympanic dexamethasone injection can be administered into middle ear space every 3 to 7 days for a total of 3 to 4 sessions. Intratympanic steroids can be a valuable solution for patients with sudden SNHL who either cannot tolerate systemic steroid therapy or are refractory to it. For patients with diabetes who cannot take systemic steroids, intratympanic steroid injection may be an alternative [12].
Prognosis for recovery is dependent on a number of factors, including patient age, presence of vertigo at onset, degree of hearing loss, audiometric configuration, and time between onset of hearing loss and treatment [3]. Early treatment, within 7 days of symptom onset, is associated with good prognosis, hearing improvement in 49-79% of patients [13]. The greatest improvement in hearing usually occurs during the first 2 weeks; late recovery has been reported but is a rare event [3]. In the present case, the prompt diagnosis and treatment seemed to help the recovery of hearing loss.
In conclusion, sudden SNHL is an unusual complication of laparoscopic cholecystectomy. Clinical suspicion is required for early diagnosis of this rare complication because early treatment may improve recovery and prognosis. Therefore, it is prudent for surgeons to be aware of this possible complication of laparoscopic cholecystectomy. Although the role of corticosteroids is undocumented in postoperative SNHL, high-dose steroid therapy can be beneficial.
Grant Support
This study was supported by research fund from Chosun University Hospital, 2012.
Conflict of Interest
None of the authors has a conflict of interest to declare.
| References | ▴Top |
- Plasse HM, Mittleman M, Frost JO. Unilateral sudden hearing loss after open heart surgery: a detailed study of seven cases. Laryngoscope. 1981;91(1):101-109.
doi pubmed - Srinivasan B, Ethunandan M, Markus A. Sensorineural hearing loss after dental extraction under general anesthesia: report of a case. J Oral Maxillofac Surg. 2008;66(9):1939-1941.
doi pubmed - Stachler RJ, Chandrasekhar SS, Archer SM, Rosenfeld RM, Schwartz SR, Barrs DM, Brown SR, et al. Clinical practice guideline: sudden hearing loss. Otolaryngol Head Neck Surg. 2012;146(3 Suppl):S1-35.
doi pubmed - Galanopoulos G, Rapti D, Nikolopoulos I, Lambidis C. Sudden sensorineural hearing loss after varicose vein surgery under general anesthesia. Case report. G Chir. 2011;32(8-9):385-387.
pubmed - Park P, Toung JS, Smythe P, Telian SA, La Marca F. Unilateral sensorineural hearing loss after spine surgery: Case report and review of the literature. Surg Neurol. 2006;66(4):415-418; discussion 418-419.
doi pubmed - Millen SJ, Toohill RJ, Lehman RH. Sudden sensorineural hearing loss: operative complication in non-otologic surgery. Laryngoscope. 1982;92(6 Pt 1):613-617.
pubmed - Walsted A, Andreassen UK, Berthelsen PG, Olesen A. Hearing loss after cardiopulmonary bypass surgery. Eur Arch Otorhinolaryngol. 2000;257(3):124-127.
doi pubmed - Journeaux SF, Master B, Greenhalgh RM, Bull TR. Sudden sensorineural hearing loss as a complication of non-otologic surgery. J Laryngol Otol. 1990;104(9):711-712.
doi pubmed - Son HJ, Joh JH, Kim WJ, Chin JH, Choi DK, Lee EH, Sim JY, et al. Temporary bilateral sensorineural hearing loss following cardiopulmonary bypass -A case report. Korean J Anesthesiol. 2011;61(2):162-165.
doi pubmed - de la Cruz M, Bance M. Bilateral sudden sensorineural hearing loss following non-otologic surgery. J Laryngol Otol. 1998;112(8):769-771.
doi pubmed - Segal S, Man A, Winerman I. Labyrinthine membrane rupture caused by elevated intratympanic pressure during general anesthesia. Am J Otol. 1984;5(4):308-310.
pubmed - Seggas I, Koltsidopoulos P, Bibas A, Tzonou A, Sismanis A. Intratympanic steroid therapy for sudden hearing loss: a review of the literature. Otol Neurotol. 2011;32(1):29-35.
doi pubmed - Battaglia A, Burchette R, Cueva R. Combination therapy (intratympanic dexamethasone + high-dose prednisone taper) for the treatment of idiopathic sudden sensorineural hearing loss. Otol Neurotol. 2008;29(4):453-460.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


