| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 4, Number 11, November 2013, pages 748-752
Acute Ischemic Stroke in Young Immunocompromised Patient With Hypolipidemia
Saravana Devulapallia, Mohankumar Kurukumbia, e, Mohammed Waqar Ahmedb, Ayyapa Dubac, Dulara Hussaind
aDepartment of Neurology, Howard University Hospital, Washington, D.C., USA
bDepartment of Psychiatry, Howard University Hospital, Washington, D.C., USA
cDepartment of Internal Medicine, Howard University Hospital, Washington, D.C., USA
dDepartment of Regional Neurology, Cleveland Clinic Foundation, Cleveland, OH, USA
eCorresponding author: Mohankumar Kurukumbi, Department of Neurology, Howard University Hospital, 2041 Georgia Ave. Washington, D.C., 20060, USA
Manuscript accepted for publication October 2, 2013
Short title: Ischemic Stroke in HIV Infection
doi: https://doi.org/10.4021/jmc1513w
| Abstract | ▴Top |
Although majority of strokes occur at age over 65, nearly one-fourth of strokes occur in people under age of 65. In 30% of these patients, the cause of stroke remains undetermined and therefore there is a need for discovering rare risk factors like human immunodeficiency virus (HIV). The incidence of stroke in young adults lacks the traditional risk factors such as hypertension and diabetes, but HIV-infected patients can manifest with stroke at younger age. Pathogenesis of ischemic stroke in HIV infection is unclear but is postulated to be caused by several possible mechanisms, including opportunistic infection, vasculopathy, cardioembolism, coagulopathy and combination antiretroviral therapies, and so on. Secondary hypolipidemia is common in the setting of chronic infection like HIV and anemia. Low serum cholesterol is a known cause for intracerebral hemorrhage. Hypolipidemia causing ischemic stroke is unknown. We report a unique case of ischemic stroke in young severely immunocompromised patient in the setting of hypolipidemia.
Keywords: Ischemic stroke; HIV; Hypolipidemia; Infection
| Introduction | ▴Top |
Nearly one-fourth of all strokes occur in people under age of 65 and in 30% of these patients, the cause of stroke remains undetermined and therefore there is a need for discovering rare risk factors like human immunodeficiency virus (HIV) infection. The incidence of stroke in young adults lacks the traditional risk factors such as hypertension and diabetes, but HIV-infected patients can manifest with stroke at younger age. Ischemic stroke in hypolipidemia is very unusual. Here we present a 31-year-old African American female with HIV infection and hypolipidemia presenting with acute ischemic stroke.
| Case Report | ▴Top |
A 31-year-old African American female presented to the emergency room with acute onset of left-sided weakness of few hours duration. The weakness began in the left upper extremity and advanced to the lower extremity later during the hospital course. Her past medical history was significant for HIV infection for the past 5 years. She was on Stribild for HIV infection but was not compliant for past couple of months.
Her family history was negative for any neurological or hematological conditions. On initial presentation, the patient had normal vitals including the blood pressure of 114/78 mmHg. She has left upper extremity 0/5 on MRC (Medical Research Council) scale for motor strength and 3/5 in left lower extremity and she remained alert and oriented with normal speech. The patient was also noted to have a left-sided facial weakness. Rest of the neurological examination was within normal limits.
Magnetic resonance imaging (MRI) of brain and magnetic resonance angiography (MRA) of head and neck with and without contrast revealed right corona radiata ischemic stroke extending to the periventricular region and did not show any evidence of cerebral hemorrhage, intracranial stenosis, thrombus, carotid dissection, carotid artery disease and contrast enhancement (Fig. 1a, 1b, 2a, 2b). Magnetic resonance venography (MRV) showed no evidence of sinus thrombosis (Fig. 3). She also has microhemorrhages in susceptibility-weighted imaging (SWI) sequence of MRI (Fig. 4a, b, c). Ultrasonography of bilateral carotid arteries was reported to be normal. Two-dimensional echocardiogram showed normal ejection fraction and no other abnormalities. She has normal sinus rhythm throughout the hospital course. Her initial laboratory examination was significant for anemia (hemoglobin: 8.4 gm/dL, hematocrit: 26.6%), leucopoenia (white blood cells: 1.7/mm3) and platelet count of 69,000/mm3. Her cholesterol, low density lipoprotein and high density lipoprotein levels are 65 mg/dL, 37 mg/dL and 27 mg/dL.
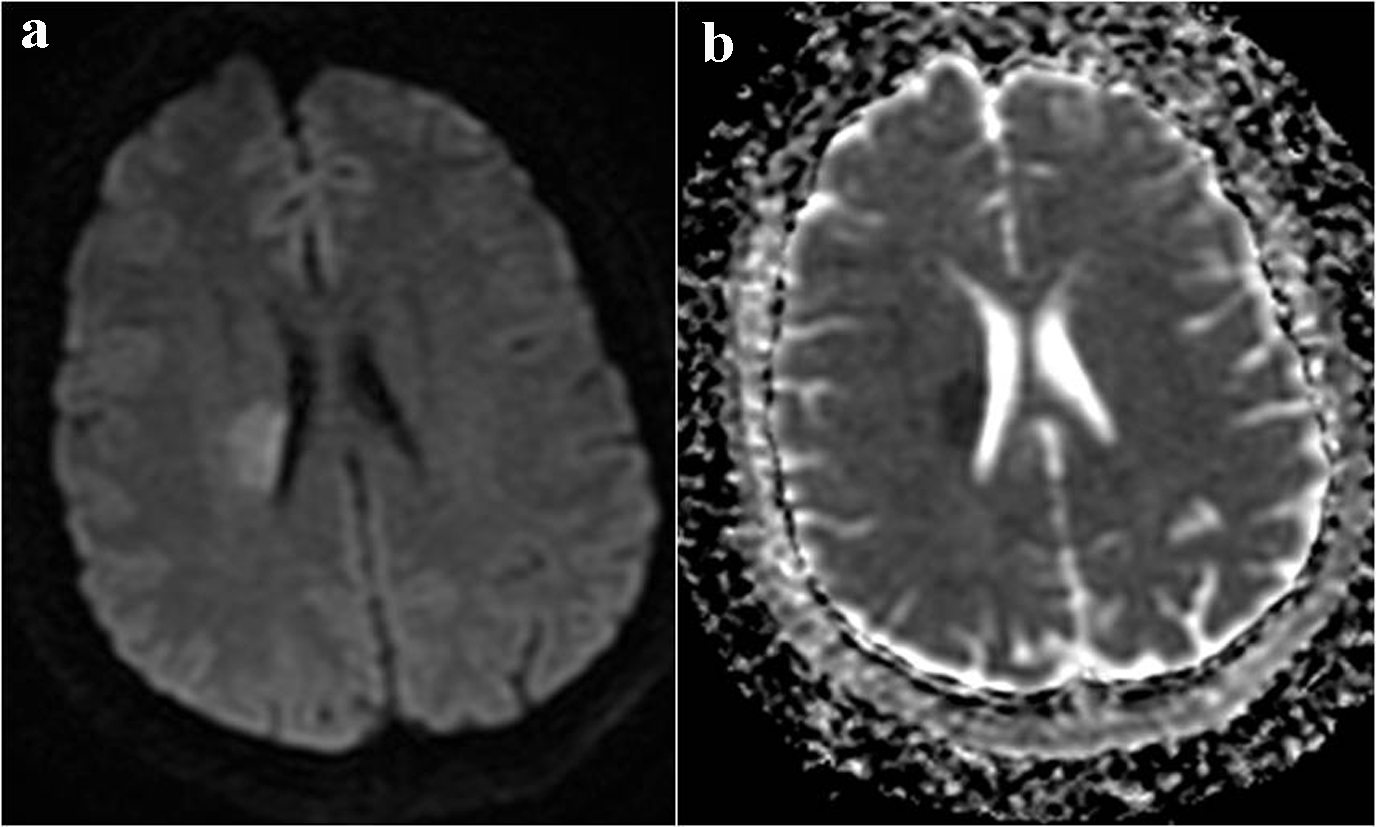 Click for large image | Figure 1. MRI brain (a) DWI showing hyperintensity in right corona radiata and (b) ADC showing corresponding mismatch in the same region, confirming acute stroke. |
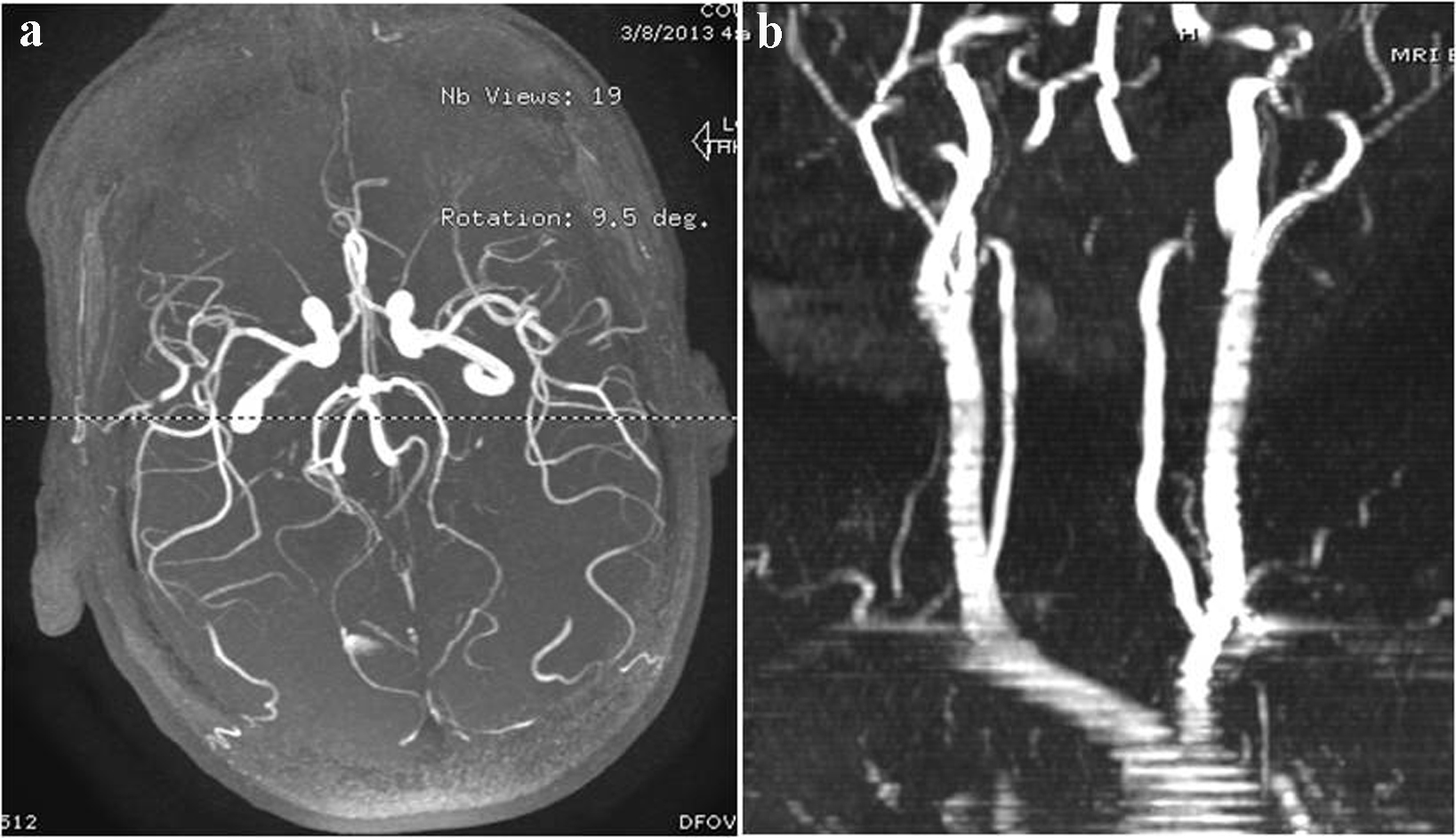 Click for large image | Figure 2. MRA brain and neck (a) showing no evidence for intracranial stenosis (b) showing no evidence for carotid artery stenosis or dissection. |
 Click for large image | Figure 3. MRV showing no evidence for venous thrombosis. |
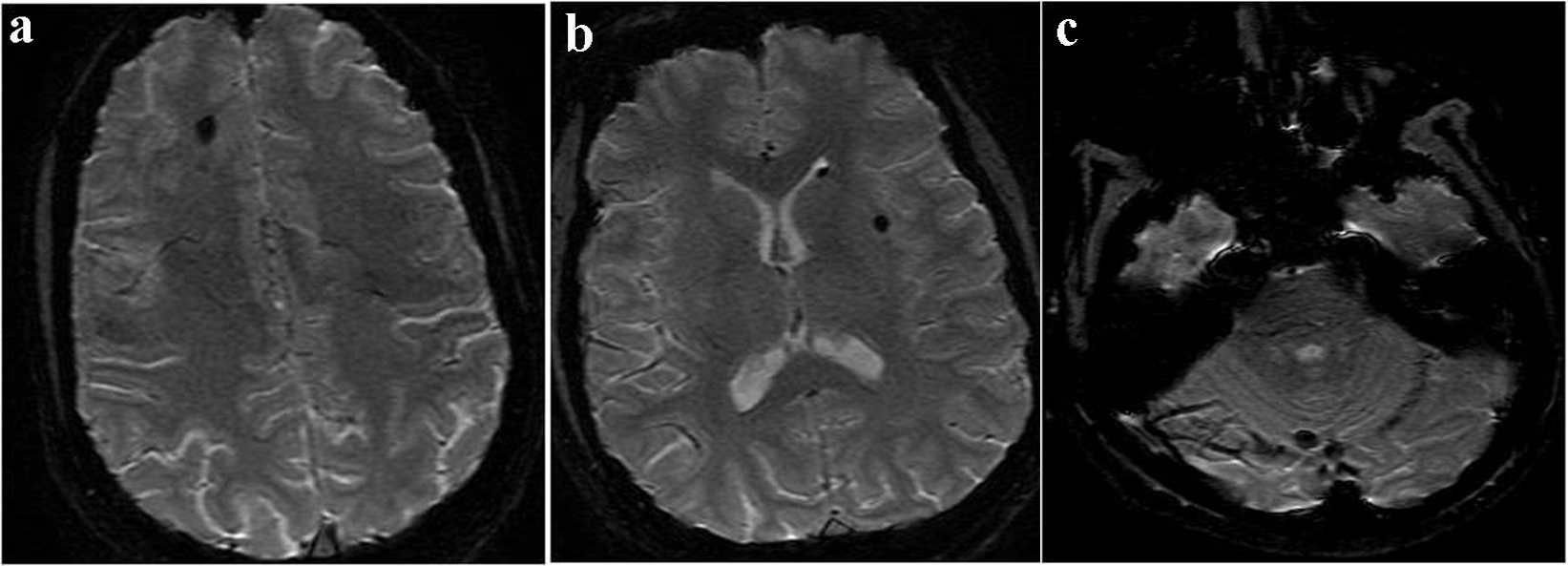 Click for large image | Figure 4. (a, b, c) SWI sequence of MRI showing microhemorrhages. |
Homocysteine level was 12.8 µmol/L which is slightly above normal. Her urine toxicology screen was negative. All other possible confounding factors for stroke were excluded by performing Leiden V, anticardiolipin antibodies, antinuclear antibody and protein C tests, which were normal. Total protein S was slightly low with a value of 64% of normal. Her rheumatoid factor was within normal limits and serum toxoplasma antibodies were negative. Her cerebrospinal fluid study was deferred. Her CD4 count was 4.
Patient received physical therapy and was able to ambulate with the help of a cane and she was discharged home in stable condition with home physical therapy.
| Discussion | ▴Top |
One to five percent of patients with HIV infection, up to 7% of acquired AIDS patients clinically develop stroke and 4-34% have ischemic cerebral lesions at autopsy [1]. No prospective studies till now assessed HIV infection and stroke [1]. Ischemic strokes are more common than hemorrhagic strokes and there is no clear association between HIV infection and types of stroke classified according to TOAST criteria [2-4].
The incidence of stroke is low in young adults as they lack the traditional risk factors such as hypertension and diabetes, but HIV-infected patients manifest with stroke at a younger age [1]. Ovbiagele and Nath reported a median age for individuals who had stroke with HIV infection of 42.9 years in 1997 and 48.4 years in 2006 in their review of database. Ortiz and colleagues reported a median age of 42 years between 1996 and 2004 in a similar setting [2, 5]. In one study, mean age of the HIV-infected stroke patients (33.4 years) was considerably lower than the mean age of the patients determined not to be HIV-infected (64.0 years) and recent or intercurrent infection was 6.4 times more likely to be associated with HIV-related stroke [6].
Hemorrhagic stroke in HIV infection is probably caused by vasculopathy, mycotic aneurysm and thrombocytopenia [1]. The etiology of cerebral infarction or transient neurological deficit in AIDS patients can be found in approximately 50% of cases; in others the pathogenesis is unclear [7]. Ischemic stroke in HIV infection can be caused by several possible mechanisms, including opportunistic infection, vasculopathy, cardioembolism, coagulopathy and combination antiretroviral therapies, and so on, although no established theory exists [1]. The current thought is that vasculopathy, due to the direct toxic effect of viral antigen, is an important mechanism of stroke in AIDS patients [8]. HIV infection causes neuronal injury without being found in neurons through the toxicity of viral proteins and chronic proinflammatory state induced by local viral replication [9]. Detailed pathophysiology is beyond the scope of this case report. Protein C and protein S deficiencies have been reported in stroke patients with HIV infection [1]. Our patient has slightly low protein S and slightly elevated homocysteine levels.
Acceleration of large vessel atherosclerosis, endothelial injury and dyslipidemia can be caused by antiretroviral therapy [10]. FABP4 (fatty acid binding protein-4) is a strong plasma marker of metabolic disturbances in HIV-infected patients, and therefore, could serve to guide therapeutic intervention in this group of patients [11]. Our patient has normal ultrasound carotid and MRA of brain and neck which rules out atherosclerotic changes. Non-nucleotide reverse transcriptase inhibitors and protease inhibitors are reported to cause endothelial inflammation and increase cardiovascular risk, but unknown regarding cerebrovascular events [1].
Secondary causes of hypolipidemia are much more common than the primary disorders. Chronic HIV infection and anemia are the most probable causes for hypolipidemia in our patient. Our patient does not have malabsorption symptoms, abnormal liver function and is not on any lipid lowering agent. HIV infection is associated with hypocholesterolemia during the asymptomatic phase and alters with immune function [12]. Mechanism of hypolipidemia in chronic infection like HIV includes exposure to interleukin 6, 10 and tumor necrosis factor [13]. Hypolipidemia in anemia is probably secondary to increased cholesterol requirements by the proliferating erythoid cells, elevated serum level of macrophage colony stimulating factor, hypersplenism and autoantibodies against low density lipoproteins [14]. Low cholesterol is a known cause for intracerebral hemorrhage [15]. Cerebral microbleeds were reported in patients with hypolipidemia in association with hypertension [16]. Our patient has microbleeds without history of hypertension. Hypolipidemia causing ischemic strokes is unknown. To our knowledge, we are reporting this first case of ischemic stroke in severe hypolipidemia in the setting of HIV infection. HIV vasculopathy might be playing an important role in causing ischemic stroke rather than hypolipidemia causing cerebral hemorrhage in our patient. Our patient was on newly approved Stribild (Elvitegravir/cobicistat/emtricitabine/tenofovir), which she stopped for couple of months before the hospital admission that resulted in her low CD4 count. It is not known whether Stribild has any role in the pathogenesis of stroke and further studies are needed to confirm this.
Conclusion
We report a case of ischemic stroke in young severely immunocompromised patient without any opportunistic infection. The pathogenesis of stroke in HIV infection is not clear. However vasculopathy due to the direct toxic effect of viral antigen is considered in our patient, in the absence of classical atherosclerotic risk factors and ruling out the other causes of stroke in young patient. Ischemic stroke in the setting of hypolipidemia was unique in our patient with underlying HIV infection.
Grant Support
None.
Conflict of Interest
None.
Abbreviations
AIDS: Acquired Immunodeficiency Syndrome; ADC: Apparent Diffusion Coefficient; DWI: Diffusion Weighted Image; HIV: Human Immunodeficiency Virus; MRA: Magnetic Resonance Angiography; MRI: Magnetic Resonance Imaging; MRV: Magnetic Resonance Venography; SWI: Susceptibility-Weighted Imaging
| References | ▴Top |
- Benjamin LA, Bryer A, Emsley HC, Khoo S, Solomon T, Connor MD. HIV infection and stroke: current perspectives and future directions. Lancet Neurol. 2012;11(10):878-890.
doi - Ortiz G, Koch S, Romano JG, Forteza AM, Rabinstein AA. Mechanisms of ischemic stroke in HIV-infected patients. Neurology. 2007;68(16):1257-1261.
doi pubmed - Tipping B, de Villiers L, Candy S, Wainwright H. Stroke caused by human immunodeficiency virus-associated intracranial large-vessel aneurysmal vasculopathy. Arch Neurol. 2006;63(11):1640-1642.
doi pubmed - Mochan A, Modi M, Modi G. Protein S deficiency in HIV associated ischaemic stroke: an epiphenomenon of HIV infection. J Neurol Neurosurg Psychiatry. 2005;76(10):1455-1456.
doi pubmed - Ovbiagele B, Nath A. Increasing incidence of ischemic stroke in patients with HIV infection. Neurology. 2011;76(5):444-450.
doi pubmed - Tipping B, de Villiers L, Wainwright H, Candy S, Bryer A. Stroke in patients with human immunodeficiency virus infection. J Neurol Neurosurg Psychiatry. 2007;78(12):1320-1324.
doi pubmed - Saul RF, Gallagher JG, Mateer JE. Sudden hemiparesis as the presenting sign in cryptococcal meningoencephalitis. Stroke. 1986;17(4):753-754.
doi pubmed - Rabinstein AA. Stroke in HIV-infected patients: a clinical perspective. Cerebrovasc Dis. 2003;15(1-2):37-44.
doi pubmed - McArthur JC, Steiner J, Sacktor N, Nath A. Human immunodeficiency virus-associated neurocognitive disorders: Mind the gap. Ann Neurol. 2010;67(6):699-714.
pubmed - Sen S, Rabinstein AA, Elkind MS, Powers WJ. Recent developments regarding human immunodeficiency virus infection and stroke. Cerebrovasc Dis. 2012;33(3):209-218.
doi pubmed - Coll B, Cabre A, Alonso-Villaverde C, Lazaro I, Aragones G, Parra S, Girona J, et al. The fatty acid binding protein-4 (FABP4) is a strong biomarker of metabolic syndrome and lipodystrophy in HIV-infected patients. Atherosclerosis. 2008;199(1):147-153.
doi pubmed - Shor-Posner G, Basit A, Lu Y, Cabrejos C, Chang J, Fletcher M, Mantero-Atienza E, et al. Hypocholesterolemia is associated with immune dysfunction in early human immunodeficiency virus-1 infection. Am J Med. 1993;94(5):515-519.
doi - Bologa RM, Levine DM, Parker TS, Cheigh JS, Serur D, Stenzel KH, Rubin AL. Interleukin-6 predicts hypoalbuminemia, hypocholesterolemia, and mortality in hemodialysis patients. Am J Kidney Dis. 1998;32(1):107-114.
doi pubmed - Elmehdawi R. Hypolipidemia: a word of caution. Libyan J Med. 2008;3(2):84-90.
doi pubmed - Segal AZ, Chiu RI, Eggleston-Sexton PM, Beiser A, Greenberg SM. Low cholesterol as a risk factor for primary intracerebral hemorrhage: A case-control study. Neuroepidemiology. 1999;18(4):185-193.
doi pubmed - Valappil AV, Chaudhary NV, Praveenkumar R, Gopalakrishnan B, Girija AS. Low cholesterol as a risk factor for primary intracerebral hemorrhage: A case-control study. Ann Indian Acad Neurol. 2012;15(1):19-22.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


