| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 1, January 2014, pages 23-25
Ranolazine as Treatment of Microvascular Coronary Dysfunction in a Woman With Signs and Symptoms of Ischemia but No Obstructive Coronary Artery Disease
Zainab Miana, Puja K. Mehtaa, Janet Weia, Chrisandra Shufelta, Melody Zayaa, Afsaneh Haftbaradarana, Louise E.J. Thomsona, C. Noel Bairey Merza, b
aThe Barbra Streisand Women’s Heart Center, Cedars-Sinai Heart Institute, Cedars-Sinai Medical Center, Los Angeles, California, USA
bCorresponding author: C. Noel Bairey Merz, 8631 W. Third Street, Suite 740 East, Los Angeles, California 90048, USA
Manuscript accepted for publication October 2, 2013
Short title: Microvascular Coronary Dysfunction Treatment
doi: https://doi.org/10.4021/jmc1522w
| Abstract | ▴Top |
Women often exhibit persistent symptoms, functional disability and a relatively high prevalence of microvascular coronary dysfunction (MCD) with no obstructive coronary artery disease (CAD) when evaluated for signs and symptoms of myocardial ischemia. A 27-year-old woman was referred by her treating cardiologist for symptoms of persistent chest pain for 10 years. Cardiac catheterization showed normal coronary arteries. Given the constellation of persistent chest pain and no obstructive CAD, a diagnosis of MCD was suspected, and she underwent coronary reactivity testing (CRT) with intracoronary infusions of adenosine, acetylcholine and nitroglycerin to test nonendothelial- and endothelial-dependent, micro- and macro-vascular coronary function. CRT results were consistent with a diagnosis of MCD. The patient was started on ranolazine, with significant improvement in symptoms. Cardiac magnetic resonance imaging (CMRI) after 3 months of treatment demonstrated improvement in perfusion compared to baseline.
Keywords: Microvascular coronary dysfunction; No obstructive coronary artery disease; Ranolazine; Cardiac magnetic resonance imaging
| Introduction | ▴Top |
Women with signs and symptoms of myocardial ischemia often have no obstructive coronary artery disease (CAD) by invasive coronary angiography when compared to men. Microvascular coronary dysfunction (MCD) with open coronary arteries is associated with a female predominance, pain that can be disabling, and inconsistent responses with use of conventional anti-ischemic therapy [1, 2]. MCD should be diagnosed and treated adequately due to compromised quality of life and increased association with adverse cardiac outcomes [3]. Ranolazine has been observed to improve the symptoms of myocardial ischemia and improve the quality of life in such patients [4]. MCD appears to be a key contributory mechanism for myocardial ischemia in women with no obstructive CAD and significant symptom improvement is seen with ranolazine [3].
| Case Report | ▴Top |
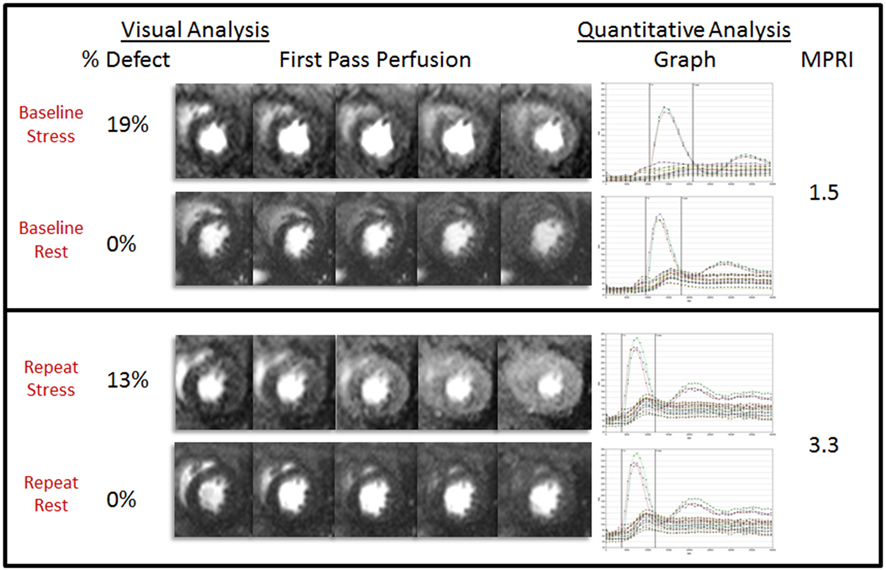
A 27-year-old woman was referred by her treating cardiologist for a 10-year history of exertional midsternal stabbing chest pain with shortness of breath and fatigue. Her symptoms began at age 17, and she was initially treated for pericarditis with non-steroidal anti-inflammatory drugs. She was subsequently treated for myocarditis after high coxsackie viral titers was identified 4 years later. Her work-up for autoimmune disease was negative, and her TSH was normal. Cardiac catheterization at age 24 revealed normal coronary arteries with no coronary anomalies. Echocardiography showed normal right ventricular and left ventricular systolic function with left ventricular ejection fraction of 60%, possible anterior leaflet mitral valve prolapse and normal valves. There was no pericardial effusion or thickening. She had no cardiac risk factors including no history of diabetes, hypertension, or family history of premature CAD. She underwent adenosine stress cardiac magnetic resonance imaging (CMRI), in which she developed chest discomfort from the adenosine infusion, but resting and stress ECG showed no abnormalities or ischemia. Adenosine-induced first-pass hypoperfusion of the subendocardium was visualized in mid-anteroseptum, anterior and anterolateral wall segments (Fig. 1). There was also circumferential subendocardial hypoperfusion in the distal left ventricle, which was measured as a reversible perfusion defect of 19% with quantitative myocardial perfusion reserve index (MPRI) of 1.5 (normal MPRI > 1.8). Pericardium was normal thickness with no pericardial effusion [5].
 Click for large image | Figure 1. CT scan showing an incarcerated right femoral hernia. |
Due to her abnormal stress CMRI and persistent symptoms, she then underwent CRT to evaluate endothelial-dependent, nonendothelial-dependent and smooth muscle coronary vasomotor pathways, as previously published [3]. Coronary angiography again showed normal appearing coronary arteries, with no luminal irregularities, no spasm, no bridging, and a normal left ventricular end-diastolic pressure of 7 mmHg. She developed moderate to severe chest discomfort during catheter manipulation in the coronary arteries and during contrast infusion, consistent with a cardiac nociception abnormality. Coronary flow reserve to intracoronary adenosine was abnormal at 1.8 (normal > 2.5), consistent with nonendothelial-dependent microvascular coronary dysfunction. Intracoronary acetylcholine testing showed 0% dilation (normal response > 0%) consistent with endothelial-dependent macrovascular coronary dysfunction, although coronary blood flow increased by 72%, which was within normal limits, indicating normal endothelial-dependent microvascular function. Response to intracoronary nitroglycerin revealed 40% dilation (normal ≥ 20% dilation) consistent with normal smooth muscle function.
She had previously been treated with metoprolol succinate 100 mg daily, verapamil ER 100 mg daily, isosorbide mononitrate 30 mg daily, and sublingual nitroglycerin as needed and had persistent symptoms. Following her CMRI and CRT, she was treated with ranolazine 500 mg twice daily, carvedilol CR 20 mg daily and isosorbide dinitrate 10 mg three times daily. After 3 months’ treatment, her angina improved from 9/10 to 5/10 in severity. Repeat CMRI scan was also improved, with a faster rate of myocardial enhancement seen in the consecutive cine images, a decrease in perfusion defect to 13% and an increase in MPRI to 3.3 (Fig. 1).
| Discussion | ▴Top |
This case highlights the clinical importance of diagnosing MCD and improvement of symptoms with the anti-anginal medication ranolazine. Ranolazine is an FDA-approved drug for the treatment of angina, and was shown to significantly improve angina scores in women with MCD in a pilot study [3]. The beneficial effects of ranolazine are proposed to be a consequence of its action to reduce sodium entry into myocardial cells through sodium channels and maintaining the sodium -calcium homeostasis [6]. Identification of angina caused by MCD is crucial due to the associated major adverse cardiac events such as myocardial infarction, congestive heart failure and sudden cardiac death. Approximately 50% of women with symptoms of persistent chest pain, evidence of ischemia and presence of no obstructive CAD have been found to have MCD [7]. Since stress testing with echocardiography and nuclear perfusion imaging may reveal normal wall motion and normal myocardial perfusion, first-pass perfusion CMRI has been used to identify and measure subendocardial perfusion defects in patients with suspected MCD [8]. As patients with MCD do not typically have vascular territory perfusion defects as seen in patients with epicardial CAD, visual interpretation of the CMRI scans may be challenging, and quantitative measurements of MPRI may be necessary to evaluate the speed and intensity of the myocardial enhancement.
The current management for the treatment of MCD includes controlling symptoms, improving quality of life and reducing hospitalization. Cardiac rehabilitation can be initiated to minimize symptoms. Statins may improve endothelial function through their anti-inflammatory and anti-oxidant properties or through their ability to restore vascular nitric oxide and thus endothelial-dependent relaxation of coronary resistance vessels. Beta blockade, particularly with atenolol, has been shown to improve functional capacity and reduce angina episodes in patients with MCD [9]. The role of nitrates and calcium channel blockers for management of MCD is not yet supported by evidence, even though these medications are first-line therapy for vasospastic angina [10].
Conclusions
Women with signs and symptoms of ischemia with no obstructive coronary artery disease often have MCD that carries an adverse prognosis. Anti-anginal medications should be used to alleviate symptoms, and novel anti-anginal, anti-ischemic medication, ranolazine, can be used as a treatment strategy.
Acknowledgments
This work was supported by contracts from the National Heart, Lung and Blood Institutes nos. N01-HV-68161, N01-HV-68162, N01-HV-68163, N01-HV-68164, grants U0164829, U01 HL649141, U01 HL649241, T32HL69751, R01 HL090957, 1R03AG032631 from the National Institute on Aging, GCRC grant MO1-RR00425 from the National Center for Research Resources, the National Center for Advancing Translational Sciences Grant UL1TR000124, and grants from the Gustavus and Louis Pfeiffer Research Foundation, Danville, NJ, The Women’s Guild of Cedars-Sinai Medical Center, Los Angeles, CA, The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, PA, and QMED, Inc., Laurence Harbor, NJ, the Edythe L. Broad Women’s Heart Research Fellowship, Cedars-Sinai Medical Center, Los Angeles, California, the Barbra Streisand Women’s Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles, The Society for Women’s Health Research (SWHR), Washington, D.C., and the Linda Joy Pollin Women’s Heart Health Program.
| References | ▴Top |
- Cannon RO
3rd . Microvascular angina and the continuing dilemma of chest pain with normal coronary angiograms. J Am Coll Cardiol. 2009;54(10):877-885.
doi pubmed - Kothawade K, Bairey Merz CN. Microvascular coronary dysfunction in women: pathophysiology, diagnosis, and management. Curr Probl Cardiol. 2011;36(8):291-318.
pubmed - Mehta PK, Goykhman P, Thomson LE, Shufelt C, Wei J, Yang Y, Gill E,
et al . Ranolazine improves angina in women with evidence of myocardial ischemia but no obstructive coronary artery disease. JACC Cardiovasc Imaging. 2011;4(5):514-522.
doi pubmed - Chaitman BR, Pepine CJ, Parker JO, Skopal J, Chumakova G, Kuch J, Wang W,
et al . Effects of ranolazine with atenolol, amlodipine, or diltiazem on exercise tolerance and angina frequency in patients with severe chronic angina: a randomized controlled trial. JAMA. 2004;291(3):309-316.
doi pubmed - Vermeltfoort IA, Bondarenko O, Raijmakers PG, Odekerken DA, Kuijper AF, Zwijnenburg A, van der Vis-Melsen MJ,
et al . Is subendocardial ischaemia present in patients with chest pain and normal coronary angiograms? A cardiovascular MR study. Eur Heart J. 2007;28(13):1554-1558.
doi pubmed - Belardinelli L, Shryock JC, Fraser H. The mechanism of ranolazine action to reduce ischemia-induced diastolic dysfunction. Eur Heart J Suppl. 2006;8(suppl A):A10-A3.
doi - Reis SE, Holubkov R, Conrad Smith AJ, Kelsey SF, Sharaf BL, Reichek N, Rogers WJ,
et al . Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE study. Am Heart J. 2001;141(5):735-741.
doi pubmed - Panting JR, Gatehouse PD, Yang GZ, Grothues F, Firmin DN, Collins P, Pennell DJ. Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N Engl J Med. 2002;346(25):1948-1953.
doi pubmed - Lanza GA, Colonna G, Pasceri V, Maseri A. Atenolol versus amlodipine versus isosorbide-5-mononitrate on anginal symptoms in syndrome X. Am J Cardiol. 1999;84(7):854-856, A858.
- Cannon RO
3rd , Watson RM, Rosing DR, Epstein SE. Efficacy of calcium channel blocker therapy for angina pectoris resulting from small-vessel coronary artery disease and abnormal vasodilator reserve. Am J Cardiol. 1985;56(4):242-246.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


