| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 5, May 2014, pages 295-297
Parapharyngeal Abscess Two Years After Elective Tonsillectomy
Fabio Arcielloa, b, Erika Crosettia, Diego Di Lisia, Giovanni Succoa
aUniversity Department of Otorhinolaringology, San Luigi Gonzaga, Martini Hospital, Torino, Italy
bCorresponding author: Fabio Arciello, Department of Otorhinolaringology, Martini Hospital, Via Tofane 71, Torino, Italy
Manuscript accepted for publication March 31, 2014
Short title: Parapharyngeal Abscess After Elective Tonsillectomy
doi: https://doi.org/10.14740/jmc1760w
| Abstract | ▴Top |
Parapharyngeal abscesses are the second most common site of deep neck infections, and should not be underestimated due to potentially fatal complications. A case of parapharyngeal abscess in a young patient, with a previous history of elective tonsillectomy performed 2 years before, is reported.
Keywords: Parapharyngeal abscesses; Tonsillectomy; Deep neck infections
| Introduction | ▴Top |
Parapharyngeal abscesses are the second most common sites of deep neck infections, after those arising in the peritonsillar area, of which they are often a consequence [1]. Despite the widespread use of antibiotics in the therapy of head and neck infections, these deep abscesses are still relatively common and should not be underestimated due to potentially fatal complications. A case of parapharyngeal abscess in a young patient, with a previous history of elective tonsillectomy performed 2 years before, is reported.
| Case Report | ▴Top |
A 19-year-old male presented to our department referring a 1-year-long history of recurrent fever associated with weakness and elevated white blood cell count. Physical examination revealed mild neck swelling and tenderness, but no other systemic symptoms. His medical history was unremarkable, except for an elective tonsillectomy performed 2 years earlier (at the age of 17) due to recurrent tonsillitis and peritonsillar abscess in the left tonsil. In the suspicion of a hematological malignancy, he was also referred for a complete blood analysis. At the time of last observation, MRI of the cervical region revealed a prestyloid parapharyngeal abscess on the left side (Fig. 1a, b). Direct inspection of the oral cavity did not reveal evident signs of involvement in the acute process documented by MRI, but did reveal fusion of the left palatine pillars (Fig. 2), which was probably a post-tonsillectomy sequela. Explorative fine needle aspiration was performed transorally, and the material was sent for microbiologic culture that subsequently revealed a polymicrobial infection.
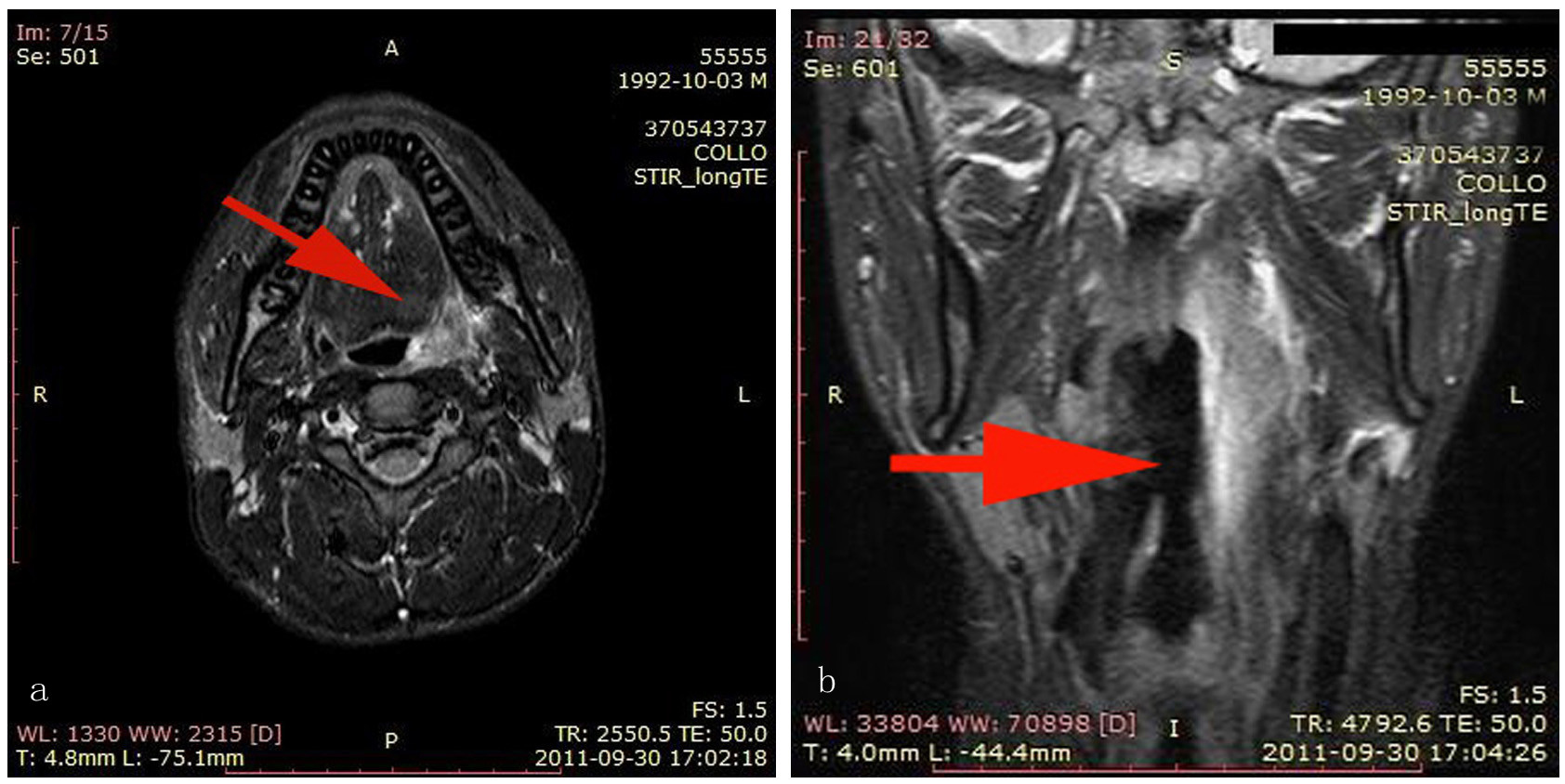 Click for large image | Figure 1. (a, b) MRI of the cervical region revealed a prestyloid parapharyngeal abscess on the left side (arrows). |
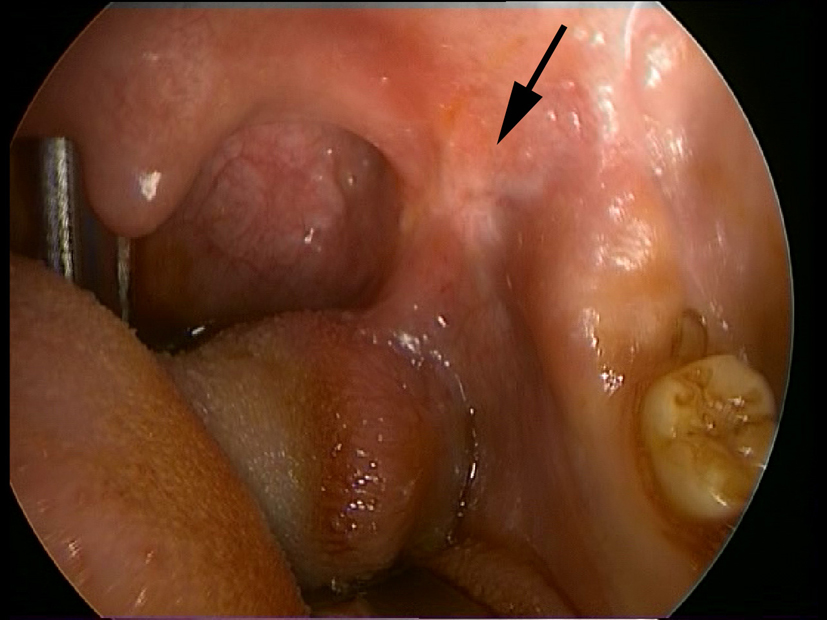 Click for large image | Figure 2. Direct inspection of the oral cavity revealed fusion of the palatine pillars (arrow) without evident signs of involvement in the acute process documented by MRI. |
Intravenous therapy based on steroids and antibiotics was administered for 10 days. Due to persistence of the abscess and new episodes of high fever (up to 41 °C), we performed surgical marsupialization (Fig. 3).
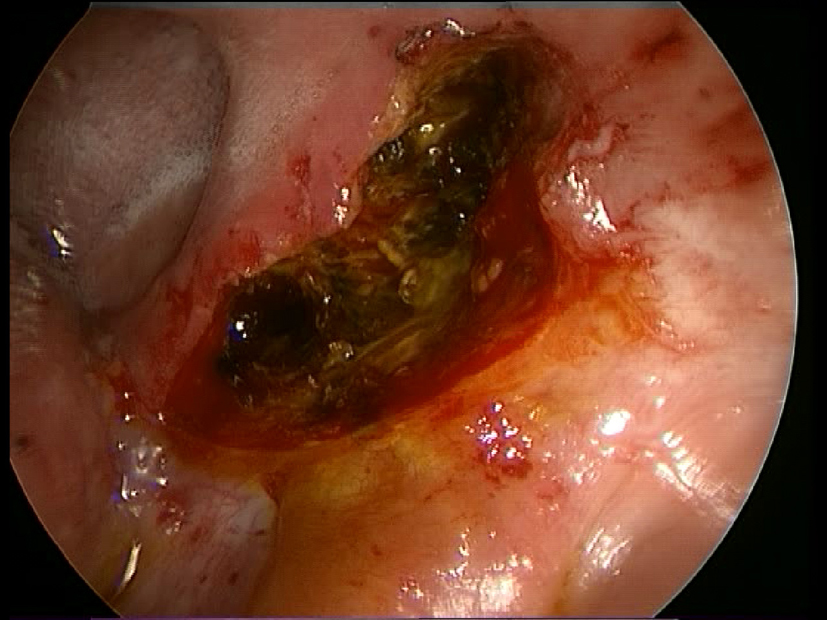 Click for large image | Figure 3. Surgical marsupialization. |
Surgical drainage was promptly performed using an intra-oral approach with healing as second intention. The surgical specimen was sent for both microbiological and pathological analyses. Pathology examination described a chronic gigantocellular infiltrate that was most likely a foreign body reaction to the previous tonsillectomy. Microbiological culture confirmed the polymicrobial population found in the first fine needle aspiration. During hospitalization, the patient continued antibiotic therapy, and the surgical wound was strictly monitored and thoroughly cleansed after every meal. The patient was discharged 8 days after surgery and is now physically well, afebrile, with no evidence of recurrence or sequelae on radiological follow-up (Fig. 4).
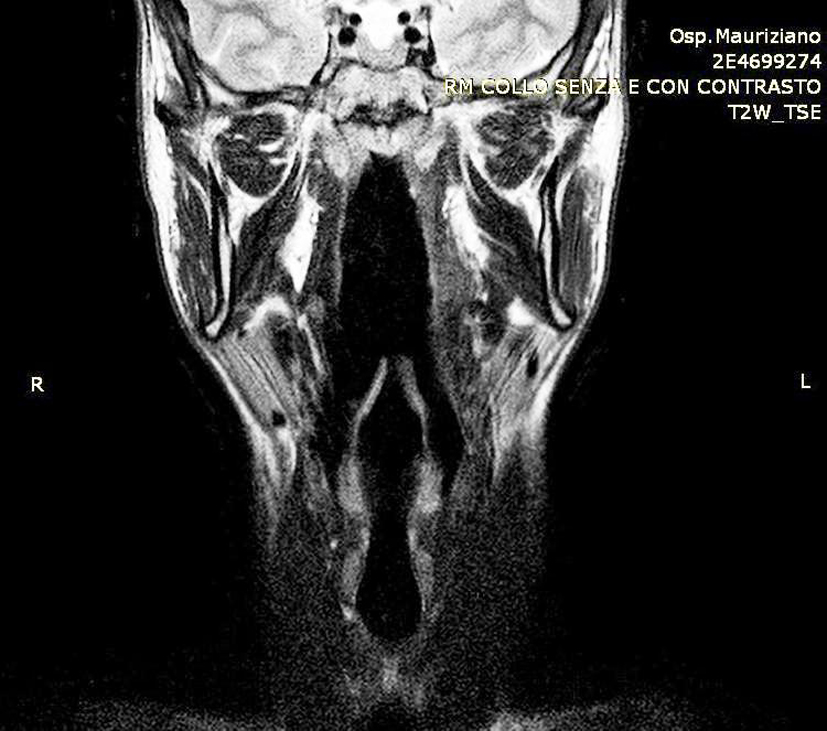 Click for large image | Figure 4. Radiological follow-up at 25 days after surgery showed no evidence of recurrence or sequelae. |
| Discussion | ▴Top |
Parapharyngeal abscess are the second most common deep neck infection, after those arising in the peritonsillar area, of which they are often a consequence [1]. Anatomically, the parapharyngeal region is located in the upper neck, extending from the skull base to the hyoid bone, and divided by the styloid process and muscles in a prestyloid and postyloid compartment, the latter containing the carotid sheath.
Clinically, parapharyngeal abscesses can be mistaken for simple quinsy, since both present with fever, trismus and medial displacement of the palatine tonsil, even though frank paraphayngeal abscesses often cause more severe symptoms, such as laryngeal deviation and unilateral neck swelling [2]. In our case, symptoms were unspecific and could be initially misinterpreted as a hematological malignancy. However, MRI revealed inflammatory involvement of the cervical region and documented its extension to the parapharyngeal space, prompting a surgical approach. Parapharyngeal abscess are most commonly diagnosed using contrast-enhanced computed tomography, since it allows reliable assessment of the extension of the abscess [3].
Even if some recent reports [1, 4, 5] have confirmed that intravenous antibiotic therapy alone, associated with strict radiological follow-up, can be successfully used in the management of uncomplicated parapharyngeal abscess, surgical drainage is the treatment of choice in cases where patients are not responsive to first-line antibiotics, with systemic symptoms or with severe complications, such as airway compromise, meningitis, mediastinitis (through retropharyngeal space) and Lemierre’s syndrome [6, 7]. Following these indications, we decided to promptly perform intraoral drainage in our patient, since he did not respond to the antibiotic therapy, and had episodes of high fever. We cannot exclude that the healing wound that created a fusion of the palatine pillars played a role in the pathogenesis of the abscess, and might have concurred in the abscess formation acting as a predisposing factor.
In conclusion, we confirm the importance of early diagnosis of parapharyngeal abscess in order to avoid possible life-threatening complications, and highlight how this condition should be considered in patients with a previous history of tonsillectomy, even if elective and apparently completely recovered.
Conflict of Interest
None.
| References | ▴Top |
- Page C, Biet A, Zaatar R, Strunski V. Parapharyngeal abscess: diagnosis and treatment. Eur Arch Otorhinolaryngol. 2008;265(6):681-686.
doi pubmed - Thapar A, Tassone P, Bhat N, Pfleiderer A. Parapharyngeal abscess: a life-threatening complication of quinsy. Clin Anat. 2008;21(1):23-26.
doi pubmed - Monobe H, Suzuki S, Nakashima M, Tojima H, Kaga K. Peritonsillar abscess with parapharyngeal and retropharyngeal involvement: incidence and intraoral approach. Acta Otolaryngol Suppl. 2007;127(559):91-94.
doi pubmed - Sichel JY, Dano I, Hocwald E, Biron A, Eliashar R. Nonsurgical management of parapharyngeal space infections: a prospective study. Laryngoscope. 2002;112(5):906-910.
doi pubmed - McClay JE, Murray AD, Booth T. Intravenous antibiotic therapy for deep neck abscesses defined by computed tomography. Arch Otolaryngol Head Neck Surg. 2003;129(11):1207-1212.
doi pubmed - Collin J, Beasley N. Tonsillitis to mediastinitis. J Laryngol Otol. 2006;120(11):963-966.
doi pubmed - Koivunen P, Lopponen H. Internal carotid artery thrombosis and Horner's syndrome as complications of parapharyngeal abscess. Otolaryngol Head Neck Surg. 1999;121(1):160-162.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


