| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 6, June 2014, pages 344-346
Median Arcuate Ligament Syndrome: A Cause of Postprandial Abdominal Pain in a Patient With Ulcerative Colitis
Elizabeth Hilla, d, Mohamed Sultanb, Walid Chalhoubb, Patrick Jacksonc, Mark Mattarb
aDepartment of Internal Medicine, MedStar Georgetown University Hospital, 3800 Reservoir Rd, Washington, DC 20007, USA
bDivision of Gastroenterology, MedStar Georgetown University Hospital, 3800 Reservoir Rd, Washington, DC 20007, USA
cDepartment of General Surgery, MedStar Georgetown University Hospital, 3800 Reservoir Rd, Washington, DC 20007, USA
dCorresponding author: Elizabeth Hill, Medstar Georgetown University Hospital Department of Internal Medicine, 3800 Reservoir Rd, Washington, DC 20007, USA
Manuscript accepted for publication April 11, 2014
Short title: Median Arcuate Ligament Syndrome
doi: https://doi.org/10.14740/jmc1773w
| Abstract | ▴Top |
We report a case of a young woman with ulcerative colitis presenting with 6-month postprandial abdominal pain, nausea, vomiting and weight loss. After an extensive diagnostic workup confirming the presence of multiple other potential causes abdominal pain including ulcerative colitis, pancreatitis and primary sclerosing cholangitis (PSC), and then she was diagnosed with median arcuate ligament syndrome (MALS). Her pain was relieved after laparoscopic lysis of median arcuate ligament.
Keywords: Median arcuate ligament syndrome; Celiac compression syndrome; Inflammatory bowel disease; Ulcerative colitis; Postprandial abdominal pain
| Introduction | ▴Top |
Median arcuate ligament syndrome (MALS) is a condition caused by the external compression of the celiac artery by the median arcuate ligament. The median arcuate ligament is a fibrous arch formed from the left and right crus crossing the aorta, usually slightly superior to the celiac artery origin [1]. Occasionally, the ligament may insert at a lower level, crossing just above the proximal portion of the celiac artery. On expiration, the median arcuate ligament moves closer to the celiac axis and can cause compression [2]. This syndrome is most common in young females with a thin body habitus. It typically presents with symptoms of postprandial abdominal pain, nausea, vomiting and weight loss.
The pathophysiology of the pain is debated between ischemia due to celiac artery compression and neurogenic disturbance from celiac plexus compression. In either case, the question arises if chronic celiac artery or nerve compression can cause other abdominal pathologies. MALS has been linked to the development of other gastrointestinal disorders such as gastroparesis [3]. Additionally a review of the literature revealed two case reports of MALS in patients with Crohn’s disease [4, 5]. We present a case of MALS in a young woman with ulcerative colitis.
| Case Report | ▴Top |
A 21-year-old woman with ulcerative colitis presented with postprandial epigastric pain, nausea, vomiting and a 50-pound weight loss over the past 6 months. She had multiple recent hospitalizations for the abdominal pain without a successful diagnosis. At the time of presentation she was relying on narcotics for pain relief. During her previous admissions she had an extensive inconclusive workup including a normal EGD, a colonoscopy showing only her known ulcerative colitis, an ultrasound of her gallbladder negative for cholelithiasis or cholecysitis and a hepatobiliary scan (HIDA) revealing a normal gallbladder ejection fraction.
On one admission her lipase was found to be elevated to 800 thus an MRCP was performed which suggested the presence of pancreatic divisum and primary sclerosing cholangitis (PSC) including a stricture in the posterior pancreatic duct. A pancreatic sphincterotomy was performed and a pancreatic duct stent was placed. She tolerated the procedure well but her pain persisted.
When she presented to our institution, we obtained a CT angiography (CTA) of the abdomen and a celiac angiogram which showed moderate to severe celiac axis narrowing (Fig. 1, 2, 3). Of note on the CTA, there was prominent retrograde collateral flow in the pancreaticoduodenal arcade and gastroduodenal artery. Such collateral flow from the SMA is a sign of severe stenosis of the celiac artery [3].
 Click for large image | Figure 1. CTA of abdomen. CTA of the abdomen shows severe narrowing of the celiac artery in our patient. |
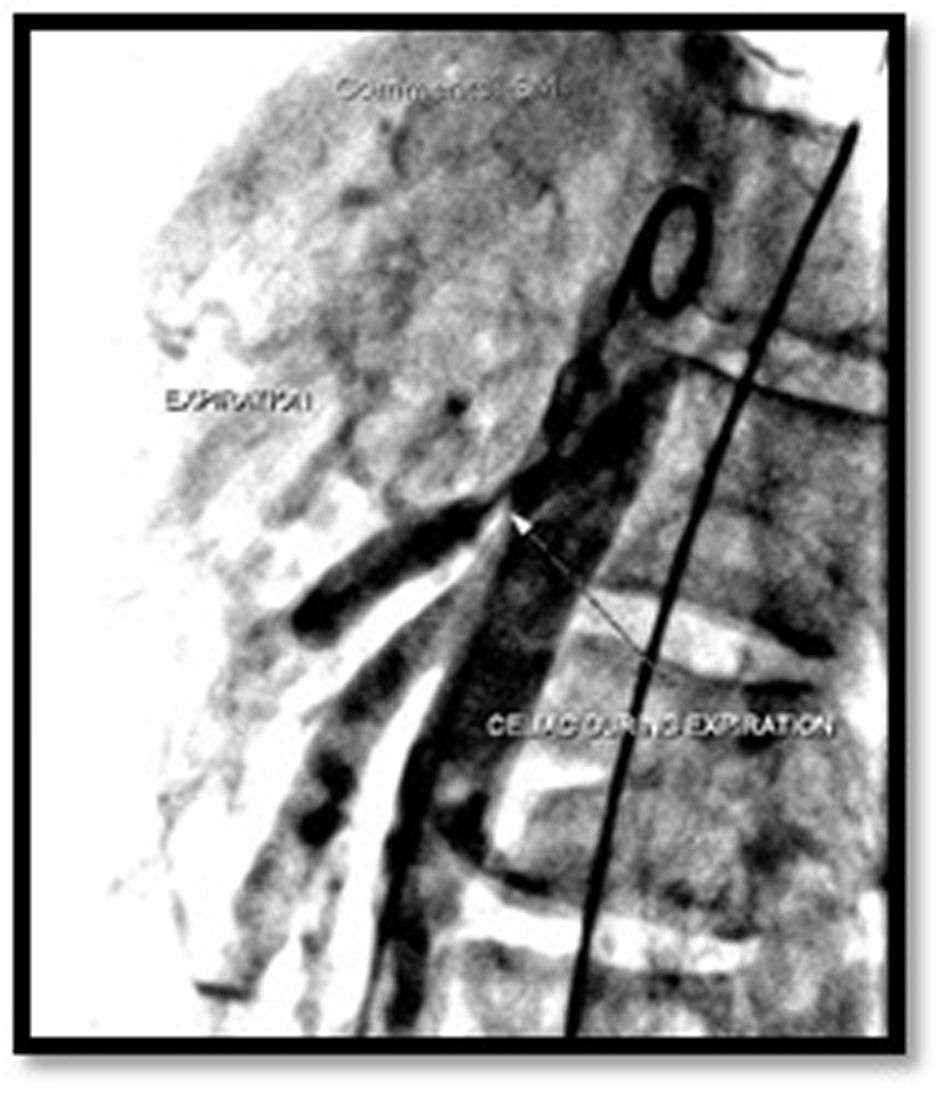 Click for large image | Figure 2. Celiac angiogram during expiration. Her celiac angiogram showed increased compression of the celiac artery during expiration. During expiration, the median arcuate ligament moves closer to the celiac axis and causes the compression. |
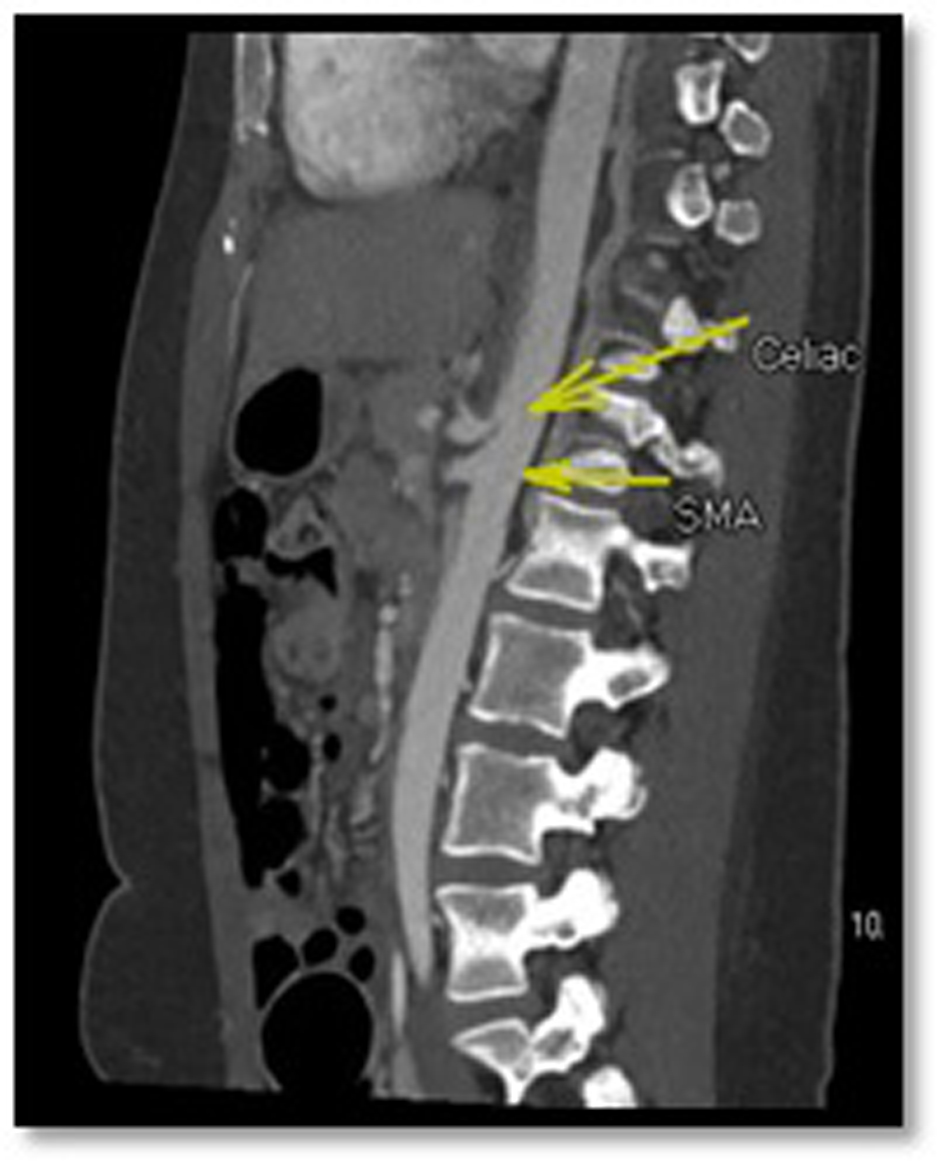 Click for large image | Figure 3. CTA of the abdomen. The proximal celiac artery is compressed compared to the superior mesenteric artery (SMA). |
She was referred to general surgery and underwent a laparoscopic lysis of median arcuate ligament as well as a cholecystectomy. Her pain immediately improved. She was discharged the next day no longer requiring narcotics. Two weeks after her surgery she continued to be pain free.
| Discussion | ▴Top |
This case exemplifies the importance of evaluating for MALS in patients with seemingly multiple other causes for abdominal pain. For example, this patient was treated for worsening ulcerative colitis, pancreatitis and pancreatic duct stricture without resolution of her pain. Her pain was finally relieved when she was treated for MALS.
The goal of treatment of MALS is restoring normal blood flow in the celiac axis. The typical treatment is laparoscopic division of the median arcuate ligament to relieve the extrinsic compression [6]. Percutaneous endovascular treatment is an alternative technique [7]. Our patient was treated with laparoscopic lysis of her arcuate ligament and had a complete remission of her abdominal symptoms. While she had a simultaneous cholecystectomy at the time of her surgery, it is important to note she had no signs of gallbladder dysfunction on ultrasound or HIDA scan. Therefore it is unlikely that the gallbladder was the sole source of her pain.
The consequence of chronic celiac trunk compression is unknown. This is one of three case reports discussing MALS in a patient with a previous diagnosis of inflammatory bowel disease [4, 5]. While no known correlation currently exists, future studies should evaluate the risk of developing inflammatory bowel disease and other gastrointestinal disorders in patients diagnosed with MALS.
Conclusion
In this patient with ulcerative colitis, a 6-month history of postprandial abdominal pain and an extensive inconclusive diagnostic workup, CTA of the abdomen confirmed presence of celiac artery compression. Her pain, nausea and vomiting resolved after lysis of the median arcuate ligament. This case exemplifies the importance of evaluating for MALS in patients with seemingly multiple other causes for abdominal pain. Additionally, it provokes the question of whether MALS can lead to other abdominal pathologies.
Disclosure
There were no conflicts of interest to report and no grant support.
| References | ▴Top |
- Horton KM, Talamini MA, Fishman EK. Median arcuate ligament syndrome: evaluation with CT angiography. Radiographics. 2005;25(5):1177-1182.
doi pubmed - Delis KT, Gloviczki P, Altuwaijri M, McKusick MA. Median arcuate ligament syndrome: open celiac artery reconstruction and ligament division after endovascular failure. J Vasc Surg. 2007;46(4):799-802.
doi pubmed - Balaban DH, Chen J, Lin Z, Tribble CG, McCallum RW. Median arcuate ligament syndrome: a possible cause of idiopathic gastroparesis. Am J Gastroenterol. 1997;92(3):519-523.
pubmed - Sturiale A, Alemanno G, Giudici F, Addasi R, Bellucci F, Tonelli F. Median Arcuate Ligament Syndrome in a patient with Crohn's disease. Int J Surg Case Rep. 2013;4(4):399-402.
doi pubmed - Biyikoglu I, Sarikaya M, Ramadan SU, Ergul B, Dogan Z. Crohn's disease masked by median arcuate ligament syndrome. Chin Med J (Engl). 2013;126(14):2798.
- Duffy AJ, Panait L, Eisenberg D, Bell RL, Roberts KE, Sumpio B. Management of median arcuate ligament syndrome: a new paradigm. Ann Vasc Surg. 2009;23(6):778-784.
doi pubmed - Hongsakul K, Rookkapan S, Sungsiri J, Tubtawee T. A severe case of median arcuate ligament syndrome with successful angioplasty and stenting. Case Rep Vasc Med. 2012;2012:129870.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


