| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 7, July 2014, pages 388-391
The Application of a Novel Non-Invasive Respiratory Monitor (ExSpiron™) in the Extubation of a Patient With Persistent Upper Airway Swelling
George W. Williamsa, b, c, Aanchal Sharmaa, Peng R. Chenb
aDepartment of Anesthesiology, The University of Texas Medical School at Houston, Houston, Texas, USA
bDepartment of Neurosurgery, The University of Texas Medical School at Houston, Houston, Texas, USA
cCorresponding Author: George W. Williams, Department of Anesthesiology, The University of Texas Medical School at Houston, 6431 Fannin, MSB 5.020, Houston, Texas 77030-1501, USA
Manuscript accepted for publication May 6, 2014
Short title: ExSpiron™ in High Risk ICU Extubation
doi: https://doi.org/10.14740/jmc1796w
| Abstract | ▴Top |
A 45-year-old female s/p right-sided cerebropontine angle tumor resection had a post-operative course which was complicated by severe sub-lingual swelling and required urgent post-operative intubation. Due to pharyngeal swelling, intubation failed with a Glidescope® requiring a laryngeal mask airway (LMA) facilitated fiberoptic-Aintree exchange. When the patient was extubated 3 days later, monitoring for respiratory deterioration was necessary to avoid the morbidity of urgent re-intubation. The ExSpiron™ was utilized for 2.5 hours following extubation, displaying her tidal volume, respiratory rate and minute ventilation. Following extubation, the patient’s neuroscience intensive care unit course was uneventful.
Keywords: Extubation; Airway; Respiratory monitor; NICU; Post-operative intubation; Laryngeal mask airway
| Introduction | ▴Top |
Respiratory mechanics (i.e. minute ventilation (MV), tidal volume (TV) and respiratory rate (RR)) are important measures used in the assessment of respiratory function and readiness for extubation. They serve as a guide in the decision-making process regarding extubation as well as potential requirement for long-term ventilation support. Modern ventilators can display such figures to facilitate the extubation process [1]. However, following extubation, there is no device which can measure tidal volume to further guide patient management. Currently available protocols use only clinical assessment of the aforementioned variables, end tidal/transcutaneous CO2 monitoring or frequent arterial blood gas analysis post extubation for decision-making, sometimes leading to delayed recognition of high arterial pCO2 levels or even CO2 “narcosis” in few patients [2-5]. Furthermore, the cost of some of the available monitors is prohibitive to their selection in many hospitals. We present a case report of a patient whose extubation was guided device ExSpiron™. The ExSpiron™ is a noninvasive, continuous respiratory monitor which has received FDA clearance to graphically display lung volumes against time. It provides the real time display reporting quantitative values of MV, TV and RR [6]. It is clinically accurate and precise when compared to the gold standard spirometer [7]. IRB and patient permission were obtained.
| Case Report | ▴Top |
A 45-year-old female with a past medical history significant for recurrent migraine headaches presented with right-sided hearing loss to Memorial Hermann Hospital Mischer Neuroscience Institute. She had occasional imbalance with quick motions, no vertigo or dysphagia, and hearing loss. Magnetic resonance imaging (MRI) scan revealed a right-sided cerebropontine angle tumor located in the posterior petrous involved with the internal auditory meatus. This tumor was about 2 × 1.8 × 1.8 cm. The plan was made for surgical resection in view of large size of the tumor with brainstem compression with the involvement of the internal auditory meatus, and the pattern of the tumor was most suggestive of meningioma. Her surgery took place under an uneventful general anesthetic, with a right retro sigmoid craniotomy, right posterior petrous meningioma resection and right-sided posterior petrosectomy. The intraoperative procedure was uneventful. She was extubated in the operating room and transferred to the neuroscience intensive care unit (NSICU) for further management. In the NSICU later the same afternoon, the patient complained of tongue numbness with a neck and tongue swelling; she remained drowsy but arousable, obeyed commands and remained hemodynamically stable with normal oxygenation. The post-operative course was complicated by severe sub-lingual swelling and required urgent intubation that same evening. Figure 1 shows the post-operative MRI which reveals the swelling of the tongue and complete obliteration of the oropharynx. The anesthesiologist on call obtained a grade II view with the Glidescope® but tube could not cannulate the trachea due to pharyngeal swelling. Subsequently, an LMA 4 was placed and patient’s trachea was intubated with a 7.0 mm ID endotracheal tube via fiberoptic-Aintree exchange. She was started on intravenous dexamethasone and mechanically ventilated with daily pressure support ventilation (continuous positive airway pressure) over the next 2 days. The oral swelling decreased significantly and she was extubated on post-operative day 3. She saturated well on 2 L/min nasal cannula oxygen without notable increased work of breathing, though the oral swelling persisted with obvious drooling. In view of her difficult intubation, it was crucial to monitor her closely so should any intervention be required, steps could be taken earlier before respiratory failure. The patient was monitored with the ExSpiron™ for 2.5 h following extubation, displaying her TV, RR and MV.
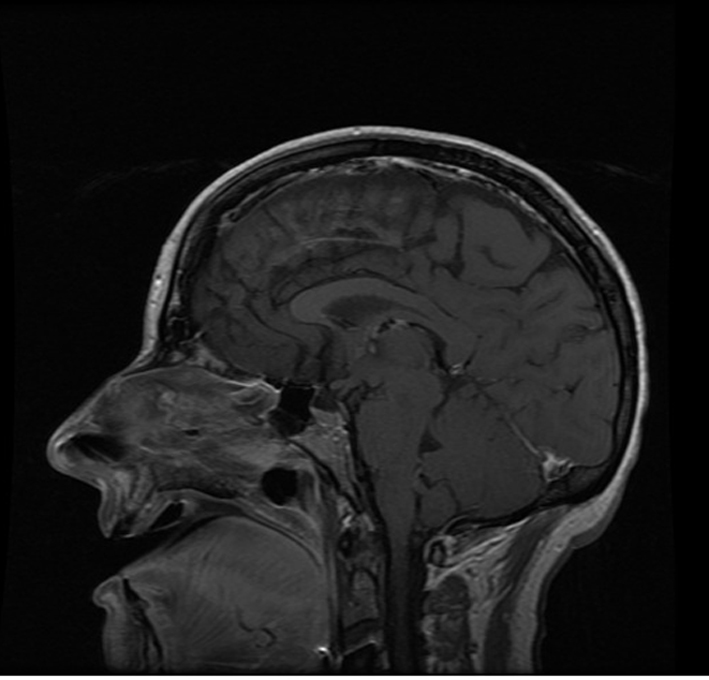 Click for large image | Figure 1.ExSpiron. ExSpiron case, post intubation MRI image POD 0. |
Additionally, the rapid shallow breathing index was calculated using these values. Figure 2 shows the TV, RR and MV values during this period. Following extubation, the patient’s NSICU course was uneventful. The patient was started on a liquid diet after the oral swelling further decreased and she was discharged on post-operative day 9.
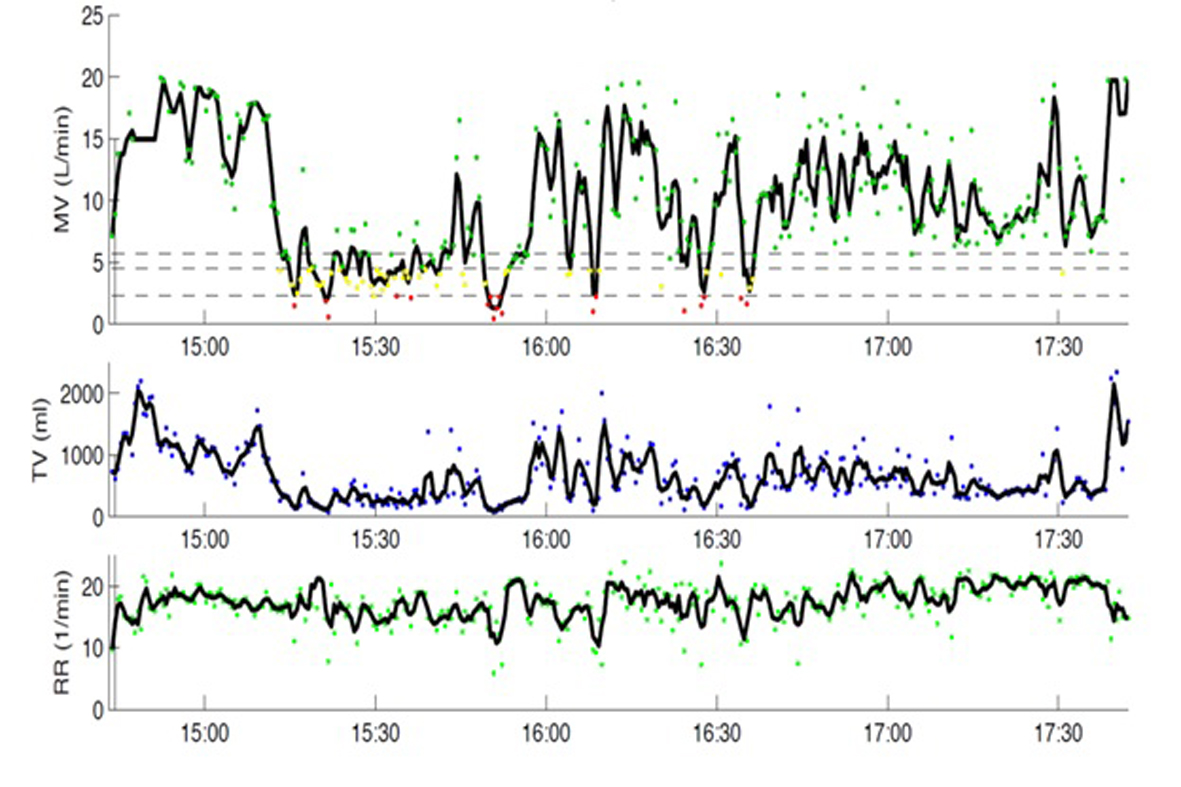 Click for large image | Figure 2. A graph demonstrating the patient's absolute values of minute ventilation, tidal volume and respiratory rate when plotted against time. MV: minute ventilation; TV: tidal volume; RR: respiratory rate. |
| Discussion | ▴Top |
This patient had a known difficult intubation which, in an emergency situation, can result in a “cannot ventilate/cannot intubate” situation. Expeditious extubation is also necessary in awake patients who are otherwise doing well to decrease the risk of ventilator associated events and overall hospital length of stay. This patient had uneventful surgery and neurologically and hemodynamically stable. The primary issue was the risky extubation secondary to an obvious oral mass. As a result, we planned to use the novel device ExSpiron™ which allowed continuous post extubation monitoring of respiratory mechanics. We were able to accurately measure the patient’s TV, RR and MV in a real time; furthermore, this monitor provided a respiratory curve similar to ECG suitable for advanced analysis. The patient was intermittently drowsy and could not swallow easily during her recovery phase, but having a monitor to confirm normal respiratory mechanics and absence of apneic events was crucial. Similar patients monitored using this device could be saved from the morbidity of re-intubation and/or repeated blood gas analysis. The patient was discharged home when the oral swelling decreased to the point that she could tolerate a liquid diet well.
Challenges remain in the monitoring of the respiratory mechanics. To date only the subjective clinical assessment, oxygen saturation and end-tidal or transcutaneous CO2 monitor are the only noninvasive means to monitor any deterioration and the need of any respiratory intervention. Heine et al observed a good correlation between end tidal (et) CO2 and PaCO2; however, they suggested that etCO2 measurements were not valid to estimate PaCO2 [8]. In another study performed by Nishiyama et al, it was concluded that transcutaneous PCO2 might be useful as noninvasive monitors of CO2 status during general anesthesia, but the absolute values are not interchangeable with PaCO2 [9]. However, these methods provide a lagging indication of pulmonary function without measurement of lung volumes. Patients with impending respiratory failure or not tolerating the post extubation phase will sometimes exhibit CO2 narcosis and unconsciousness before any intervention can be taken. This is because apneic events are often unrecognized without the objective data and SpO2 values are masked when supplemental oxygen is delivered. Ventilation monitoring and pattern assessment is not routine in most institutions. In a study done in surgical/trauma intensive care unit (STICU) patients, a multivariate model predicted increases in risk of intubation in the following 24 h based on vital sign data available currently on bedside monitors and suggested that further refinement could allow for earlier detection of respiratory decompensation and intervention to decrease preventable morbidity and mortality in STICU patients [10]. Hence ventilation monitoring is increasingly recommended as oxygen saturation levels inadequately predict ventilatory distress [2, 10]. The ExSpiron™ system is an innovative and accurate approach to quantitative assessment of respiratory function. By passing a small amount of electrical current across several vectors through the lung, and exploiting the large conductivity difference between air and tissue, it is able to accurately quantify the amount of air moving in and out of the lung in real time. This monitor has been shown to measure TV accurately in patients with upper airway obstruction and can help in detection of any prolonged apnea episodes [11] facilitating respiratory intervention before actual desaturation. MV is an early indicator of respiratory compromise and is the best way to assess respiratory competence [12]. These valuable data, previously only available for intubated patients receiving mechanical ventilation, are now available noninvasively to assess respiratory function in a wide variety of patients. This may serve not only reduce complications, but also reduce cost of care [13]. When used for monitoring in traumatic chest injuries, it was found that it provides quantitative evaluation of unilateral lung function in real time which may aid in the evaluation of the effectiveness of interventions [14]. Panasyuk et al used this monitor in elderly patients and concluded that it can be used to accurately determine RR, TV and MV in ambulatory older adults. Real-time monitoring of older post-operative patients may allow for more accurate titration of analgesics with the potential to reduce the risk of consequent respiratory depression [15]. The ExSpiron monitor has the potential to bridge the monitoring gap in non-intubated patients, as it provides an indicator of respiratory deterioration to help in directing for timely therapeutic intervention.
Conclusion
The ExSpiron™ monitor can be used to monitor post extubation respiratory mechanics in a patient with upper airway mass and a known difficult airway in order to facilitate or rule out the need for early respiratory intervention.
Conflict of Interests
None.
Grant Support/Funding
None.
| References | ▴Top |
- Lyazidi A, Thille AW, Carteaux G, Galia F, Brochard L, Richard JC. Bench test evaluation of volume delivered by modern ICU ventilators during volume-controlled ventilation. Intensive Care Med. 2010;36(12):2074-2080.
doi pubmed - Arakawa H, Kaise M, Sumiyama K, Saito S, Suzuki T, Tajiri H. Does pulse oximetry accurately monitor a patient's ventilation during sedated endoscopy under oxygen supplementation?. Singapore Med J. 2013;54(4):212-215.
doi pubmed - Belenkiy S, Ivey KM, Batchinsky AI, Langer T, Necsoiu C, Baker W, Salinas J,
et al . Noninvasive carbon dioxide monitoring in a porcine model of acute lung injury due to smoke inhalation and burns. Shock. 2013;39(6):495-500.
doi pubmed - Westlake EK. Respiratory failure and carbon dioxide narcosis. Postgrad Med J. 1958;34(387):2-6.
doi pubmed - Cavallone LF, Vannucci A. Review article: Extubation of the difficult airway and extubation failure. Anesth Analg. 2013;116(2):368-383.
doi pubmed - Freeman J, George E, Brayanov J, MacNabb CM, Cho E, Ladd D, Lalli M,
et al . The Use of a Respiratory Volume Monitor in the Assessment of Obstructed Breathing and Postoperative Apnea. Poster Presentation, American Academy of Pain Medicine, April 2013, Ft. Lauderdale, FL. - Freeman J, Yocum N, Panasyuk A, Lalli M, Panasyuk S, Fahy D, Messana E,
et al . Evaluation of the Accuracy of a Continuous, Non-Invasive System for Monitoring Tidal Volume, Respiratory Rate and Minute Ventilation in Non-Intubated Patients. Oral Presentation, American Society of Anesthesiologists, October 2012, Washington, DC. - Heines SJ, Strauch U, Roekaerts PM, Winkens B, Bergmans DC. Accuracy of end-tidal CO2 capnometers in post-cardiac surgery patients during controlled mechanical ventilation. J Emerg Med. 2013;45(1):130-135.
doi pubmed - Nishiyama T, Nakamura S, Yamashita K. Comparison of the transcutaneous oxygen and carbon dioxide tension in different electrode locations during general anaesthesia. Eur J Anaesthesiol. 2006;23(12):1049-1054.
doi pubmed - Politano AD, Riccio LM, Lake DE, Rusin CG, Guin LE, Josef CS, Clark MT,
et al . Predicting the need for urgent intubation in a surgical/trauma intensive care unit. Surgery. 2013;154(5):1110-1116.
doi pubmed - Voscopoulous C, Freeman J, Brayanov J, Ladd D, Lalli M, MacNabb C, Marshall EM. Evaluation of a Non-invasive Respiratory Volume Monitor during Obstructed Breathing. Critical Care Medicine: December 2012. 42nd Critical Care Congress, January 19-23, 2013. San Juan, Puerto Rico.
- McConnell A. The Respiratory Muscles: Respiratory Muscle Training. Uxbridge, London, United Kingdom: Elsevier Ltd, 2013:57-96.
- Freeman J, Galvagno S, Panasyuk A, Lalli M, Yocum N, Bokhenik R, Desmarais L,
et al . Evaluation of a Noninvasive Respiration Monitor for Continuous Monitoring of Respiratory Parameters. Chest. 2012;142(4_MeetingAbstracts):950A. - Freeman J, Galvagno S, Corneille M, Voscopoulous C, Sordo S, Brayanov J. Continuous Non-Invasive Monitoring of Respiratory Status of Injured Lung in Patients with Traumatic Thoracic Injuries. Critical Care Medicine: December 2012. 42nd Critical Care Congress, January 19, 2013. San Juan, Puerto Rico.
- Panasyuk A, Lalli M, Yocum N, Panasyuk S, Lew R, Freeman J. Development of a Continuous, Non-Invasive Respiratory Variation Monitor for use in Pain Management of an Aging Population. The Journal of Pain. 2012;13(4):S1.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


