| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 8, August 2014, pages 463-465
Ileitis Is Not Always Crohn’s Disease: Case Report
Abdel Rahman Omera, Omar Nadhema, b, Nibras Talibmamurya, Yasir Al Abboodia, James Lusbya, Steven Urbana
aInternal Medicine Department, Texas Tech University Health Sciences Center, Amarillo, TX, USA
bCorresponding Author: Omar Nadhem, Internal Medicine Department, Texas Tech University Health Sciences Center, 1400 Coulter, Amarillo, TX 79106, USA
Manuscript accepted for publication July 29, 2014
Short title: Ileitis Is Not Always Crohn’s Disease
doi: https://doi.org/10.14740/jmc1869w
| Abstract | ▴Top |
Eosinophilic gastroenteritis (EG) is a rare disorder characterized by eosinophilic infiltration of the bowel wall with various gastrointestinal manifestations. Clinical presentation may vary depending on sites and depth of involvement of the gastrointestinal tract. Imaging has very little role in supporting the diagnosis, and therefore a high degree of clinical suspicion is required. In this article, we describe a 51-year-old male who presented with severe abdominal pain, nausea, vomiting and constipation. CT scan of the abdomen showed ileitis and laproscopy revealed ileitis with stricture in the terminal ileum. The patient was treated with laproscopic right hemicolectomy with final diagnosis of EG.
Keywords: Eosinophilic gastroenteritis; Muscularispropria; Small bowel obstruction
| Introduction | ▴Top |
Eosinophilic gastroenteritis (EG) is a rare disorder characterized by eosinophilic infiltration of the bowel wall with various gastrointestinal manifestations [1]. The involvement of different layers of the intestinal wall usually gives rise to different clinical manifestations. The mucosal form, which is the most common EG subtype, presents with vomiting, abdominal pain, diarrhea, fecal blood loss, anemia and weight loss secondary to malabsorption. The muscularis form is characterized by infiltration of eosinophils predominantly in the muscularis layer, leading to thickening of the bowel wall, which might result in gastrointestinal obstructive symptoms. The subserosal form occurs in a minority of patients with EG, and it is characterized by exudative ascites with higher peripheral eosinophil counts compared with the other forms [2]. The etiology of EG is unknown and its pathogenesis is poorly understood. EG has features of allergy and immune dysregulation but does not clearly fit into the category of allergic or immune disorder [3]. The diagnostic criteria for the EG are well defined. They include gastrointestinal symptoms, eosinophilic infiltration in at least one area of the digestive tract demonstrated by biopsy, absence of eosinophilic infiltration in other organs outside the digestive tract and absence of parasitic infections [4]. Corticosteroids are the mainstay of therapy with a 90% response rate in some studies. Appropriate duration of steroid treatment is unknown and relapse often necessitates long-term treatment [1].
| Case Report | ▴Top |
We present a 51-year old white gentleman who presented with acute onset of severe constant right-sided abdominal pain associated with abdominal distension, nausea and vomiting. He was unable to tolerate solids or liquids. He states that he has not had a bowel movement or passed flatus in the last 48 h. He had a colonoscopy 5 months prior to this presentation which showed moderately severe diverticulosis of the sigmoid colon. Past surgical history consists of inguinal hernia repair and appendectomy.
On examination
He was in mild distress, and abdomen was soft, distended with tenderness in the right lower quadrant and otherwise normal exam.
Labs
WBC 11,800/µL with 81% neutrophils and 0.7% eosinophils, HGB 14.8 g/dL, platelets 250,000/µL. Sodium 140 mmol/L, potassium 3.9 mmol/L, chloride 107 mmol/L, CO2 26 mmol/L, glucose 137 mg/dL, BUN 10 mg/dL, creatinine 1.0 mg/dL, total bilirubin 0.8 mg/dL, total protein 6.1 g/dL, albumin 3.6 g/dL, alkaline phosphatase 52 IU/L, SGOT 20 IU/L and SGPT 20 IU/L.
Imaging
CT of abdomen and pelvis with intravenous contrast showed bowel wall thickening and inflammatory changes around the terminal ileum (Fig. 1). Findings suggest inflammatory bowel disease or infectious enteritis. Mild dilatation of the small bowel just proximal to this area may be a reactive ileus. Sigmoid and descending colon diverticulosis without features of acute diverticulitis are present.
 Click for large image | Figure 1. CT of abdomen and pelvis with intravenous contrast showed bowel wall thickening and inflammatory changes around the terminal ileum. Red arrow indicates bowel wall thickening and inflammatory changes around the terminal ileum (sagittal view). Green arrow indicates dilatation of the small bowel just proximal to ileitis area (sagittal view). |
Hospital course
The patient was kept nothing per mouth with intravenous fluids and intravenous analgesia. Surgery team was consulted and due to the severity of symptoms they decided to proceed with laproscopic procedure. During the procedure, the ileum was distended with thickened bowel wall. Several centimeters proximal to the ileocecal valve, there was a puckering which appeared to be stricture with some ulceration with no obvious cobble stoning. The colonic mucosa was tan-pink to red, smooth and glistening, and displays prominent irregular folds. Right hemicolectomy was done and the tissue was sent for pathologic evaluation.
Pathology
Dense infiltrate of eosinophils in the muscularis propria suggests EG (Fig. 2). Small areas of ischemic damage are present. Neither granulomas nor parasitic forms are identified.
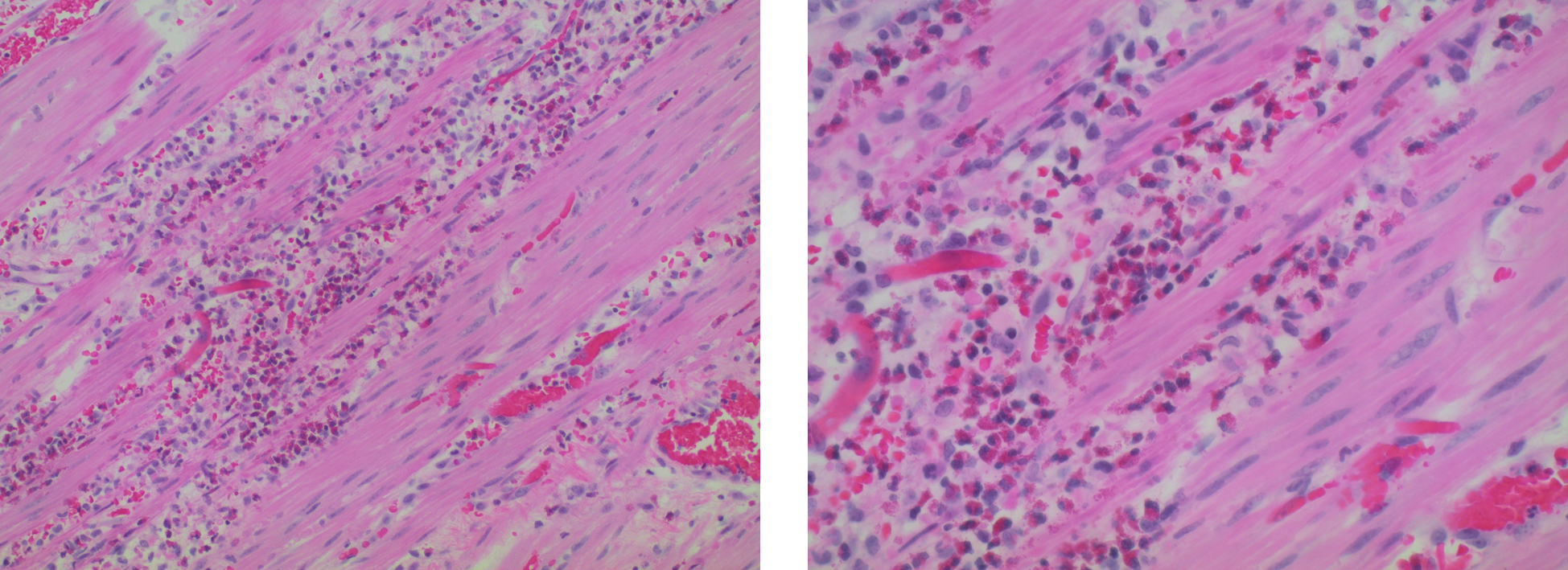 Click for large image | Figure 2. Surgical pathology: dense infiltrate of eosinophils in the muscularis propria suggests EG. |
Post-procedure course
The patient had a prolonged postoperative ileus requiring TPN for few days; however, his ileus ultimately did resolve and he was able to tolerate his diet. He was discharged home later on.
| Discussion | ▴Top |
EG is a rare, chronic relapsing inflammatory disease of the bowel characterized by the presence of peripheral eosinophilia and eosinophilic infiltration of one or more layers of the intestinal wall [5]. Clinical features depend upon the most prominent layer of visceral wall involvement by eosinophils, i.e. mucosal, muscular or serosal [6]. Approximately 57.5% have mucosal, 30% muscular and 12.5% (sub) serosal disease, respectively [7]. Although the disease may affect all ages, typical presentations are in the third through fifth decades. EG tends to have an equal gender distribution, 50% of patients may be atopic and 50% may have a history of food intolerance of allergy [8]. Mucosa-predominant disease is manifested as non-specific abdominal discomfort, malabsorption and protein-losing enteropathy [9], whereas muscularis-predominant disease leads to bowel wall thickening and intestinal obstruction. Cramping and abdominal pain associated with nausea and vomiting occur frequently. It can also present as an obstructing cecal mass or intussusception [1, 9]. In contrast, subserosa-predominant disease more commonly results in eosinophilic ascites and markedly elevated counts of eosinophils in peripheral blood [9]. Peripheral eosinophilia occurs in a variable number of EG patients (20-90%), and is not a reliable prerequisite for diagnosis [10]. The endoscopic appearance in EG is non-specific, including erythematous, friable, nodular and occasional ulcerative changes [6]. In the muscular form, endoscopy may appear normal. Most EG cases have been diagnosed on surgical, full-thickness biopsy or resection performed for obstruction or suspicion of malignancy [7, 11]. Radiographically, there is no pathognomonic appearance of EG, the appearance being identical to Crohn’s enterocolitis, with thickening and flattening of the valvulae conniventes (most common), strictures, filling defects, ulceration, polypoid lesions and rigidity of the ileocecal valve [10]. The mainstay of treatment in non-obstructive disease is a trial of dietary avoidance of food allergens, but if the symptoms persist or are severe, then corticosteroid therapy is recommended [7, 9]. Prednisone at a dose of 20 - 40 mg daily for 8 weeks can yield a good response. Budesonide is an alternative steroid with fewer systemic side effects [7]. Surgical treatment is required for patients with intestinal perforation and/or obstruction [2, 10].
In our case, the patient had small bowel obstruction due to a stricture and small bowel wall thickening caused by EG requiring surgical intervention. The patient was followed up later on with complete resolution of his symptoms.
In conclusion, eosinophilic enteritis should be considered in the differential diagnosis of ileitis. Patients, with muscular form of EG, usually present with symptoms of intestinal obstruction due to small bowel wall thickening and rarely stricture formation. Surgery is the treatment of choice in the presence of obstruction. To our knowledge, very few cases with this entity have been reported.
Conflict of Interest
The authors declare no conflict of interest.
| References | ▴Top |
- Ingle SB, Hinge Ingle CR. Eosinophilic gastroenteritis: an unusual type of gastroenteritis. World J Gastroenterol. 2013;19(31):5061-5066.
doi pubmed - Oh HE, Chetty R. Eosinophilic gastroenteritis: a review. J Gastroenterol. 2008;43(10):741-750.
doi pubmed - Koutroubakis IE. Eosinophilic gastroenteritis; the Greek experience. Annals of Gastroenterology. 2002;15(2):104-105.
- Mendez-Sanchez N, Chavez-Tapia NC, Vazquez-Elizondo G, Uribe M. Eosinophilic gastroenteritis: a review. Dig Dis Sci. 2007;52(11):2904-2911.
doi pubmed - Antunez ID, Costas PJ, Jesus RD, Baez MTF. Ascites de novo: an unusual presentation of eosinophilic gastroenteritis. Am J Gastroenterol. 2003;98:S168.
doi - Kshirsagar AY, Jagtap SV, Kanojiya RP, Langade YB, Shinde SL, Shekhar N. Eosinophilic enteritis presenting as a rare cause for ileo-ileal intussusception. World J Gastroenterol. 2007;13(47):6444-6445.
doi pubmed - Yan BM, Shaffer EA. Primary eosinophilic disorders of the gastrointestinal tract. Gut. 2009;58(5):721-732.
doi pubmed - Gonsalves N. Food allergies and eosinophilic gastrointestinal illness. Gastroenterol Clin North Am. 2007;36(1):75-91, vi.
doi pubmed - Wolpin BM, Weller PF, Katz JT, Levy BD, Loscalzo J. Clinical problem-solving. The writing on the wall. N Engl J Med. 2009;361(14):1387-1392.
doi pubmed - Shweiki E, West JC, Klena JW, Kelley SE, Colley AT, Bross RJ, Tyler WB. Eosinophilic gastroenteritis presenting as an obstructing cecal mass-a case report and review of the literature. Am J Gastroenterol. 1999;94:3644-3645.
pubmed - Mori A, Enweluzo C, Grier D, Badireddy M. Eosinophilic gastroenteritis: review of a rare and treatable disease of the gastrointestinal tract. Case Rep Gastroenterol. 2013;7(2):293-298.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


