| ||||||||||||
| Case Report | ||||||||||||
| Volume 5, Number 10, October 2014, pages 545-548 | ||||||||||||
Troponin I Elevation Due to Alcoholism in Absence of Acute Coronary Syndrome: A Case Report Hongxiu Luoa, b, Nilma Malika, Qiang Naia, Naureen Jessania, Mahmood Alama, Mohammed A. Islama, Abdalla Yousifa aDepartment of Internal Medicine, Raritan Bay Medical Center, Perth Amboy, NJ, USA Manuscript accepted for publication July 29, 2014
Cardiac troponin I (cTnI), a sensitive and specific marker for myocardial injury, has been utilized for the diagnosis of an acute myocardial infarction. However, a variety of clinical scenarios without evidence of acute coronary syndrome (ACS), such as pulmonary embolism, sepsis, renal failure or stress-induced cardiomyopathy may also cause the elevation of cTnI. We described a 55-year-old Hispanic male with abnormal elevations of cTnI without objective evidence of myocardial infarction damage. We hypothesized that his long-term chronic alcoholic intoxication is causing the myocardial injury, responsive for cTnI elevation. We proposed that alcohol-induced early myocardial damage, independent of alcoholic cardiomyopathy, might be related to alcohol-induced cTnI elevation in this patient. This is the first report suggesting that the abnormal elevations of cTnI can be seen in patients with chronic alcoholism without objective evidence of myocardial infarction. Keywords: Troponin I; Alcoholism; Acute coronary syndrome; Cardiomyopathy
Troponin is a regulatory protein complex located on the thin filament of striated muscles. It consists of three subunits: C, I and T. Troponin I has three isoforms, each controlled by different gene. One is cardiac and the other two are slow skeletal and fast skeletal isoforms. Cardiac troponin I (cTnI) is a sensitive and specific marker for myocardial injury [1, 2] and has equivalent diagnostic accuracy for acute myocardial infarction to troponin T, superseding the creatine kinase myocardial band (CK-MB) [3]. cTnI has also shown to be elevated in a variety of clinical scenarios without evidence of acute coronary syndrome (ACS), such as pulmonary embolism, sepsis, renal failure, stress-induced cardiomyopathy [4, 5] or acute rejection of heart transplants [6]. In addition, continuous cTnI elevation has been recently reported to occur in a substantial proportion of patients with Fabry disease, a rare X-linked disorder affecting homozygous males and heterozygous females [7]. Paroxysmal supraventricular tachycardia may induce elevations in cTnI in the absence of coronary artery disease (CAD) [8, 9]. However, elevation of high sensitivity cTnI has not been reported with chronic alcoholism without alcoholic cardiomyopathy. The objective of this article was to describe, for the first time, the elevation of cTnI in a patient with alcoholism who had no objective evidence of myocardial damage.
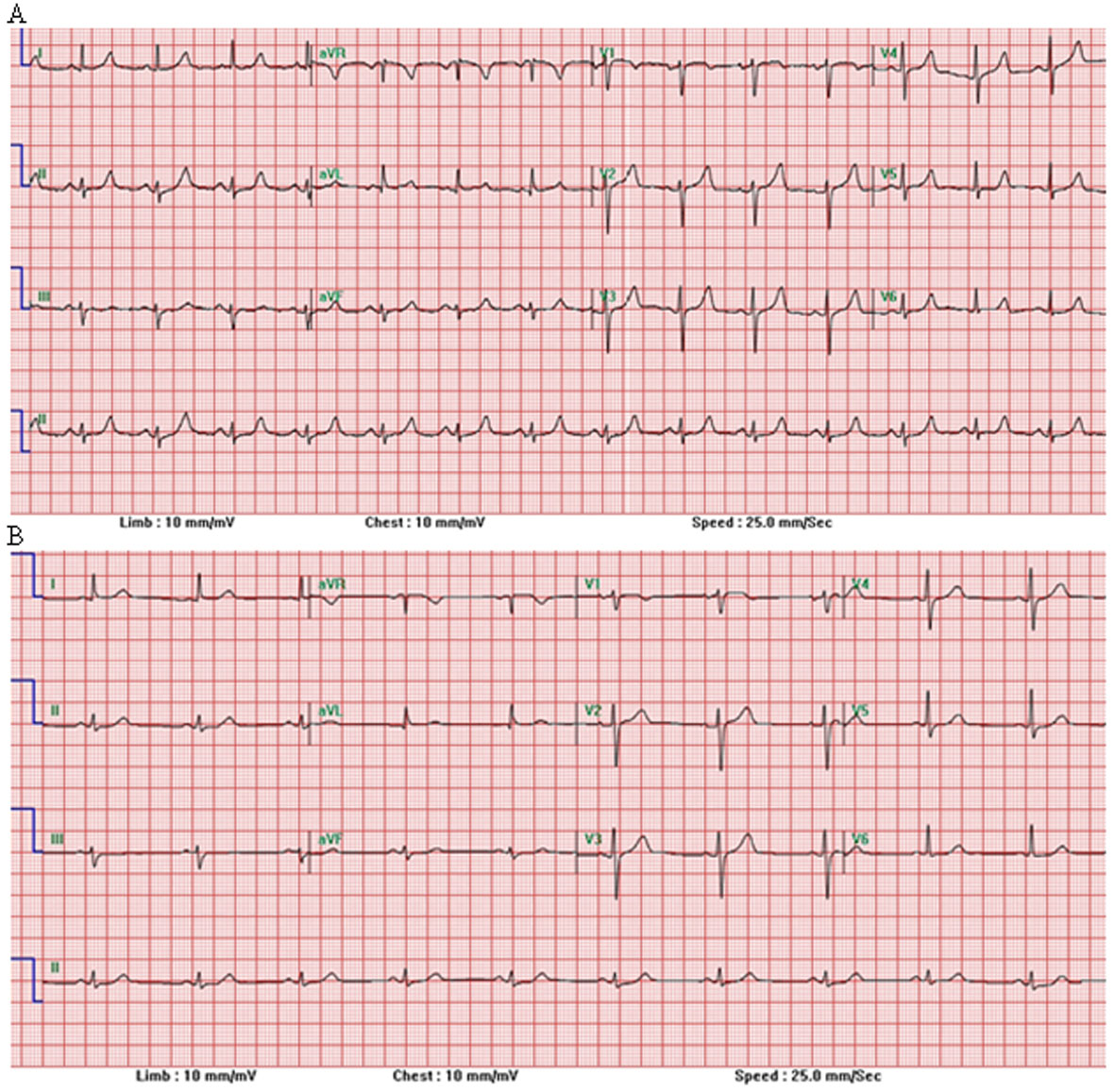
We present a case of a 55-year-old Hispanic male who was admitted for alcoholic intoxication. He has hypertension for 5 years, which has been well controlled with medication. He has been drinking alcohol for about 10 years (about 43 g per day). On his first admission to the hospital because of alcohol intoxication, patient denied symptoms of chest pain, shortness of breath or palpitations. The alcohol level was 375.2 mg/dL (normal range < 10 mg/dL). The liver function and renal function tests were normal. Urine drug screen test was negative. Laboratory determinations showed the increase of cTnI up to 0.42 ng/mL (normal range < 0.3 ng/mL) and CK levels up to 592 IU/L (normal range 20 - 200 IU/L) (Table 1). Serial electrocardiograms (EKGs) did not show any dynamic ST-segment changes (Fig. 1A). He had normal left ventricle function on his echocardiogram (Fig. 2A). The single-photon emission computed tomography (CT) pharmacological stress testing was also normal (data not shown). Therefore, cardiac catheterization was deemed unnecessary and patient was treated as non-ST segment elevation myocardial infarction and discharged home after 2 days. Five months later, this patient was, however, admitted again because of alcohol-induced pancreatitis. He did not have ACS symptoms and was hemodynamically stable. His liver and kidney function were normal. The serum alcohol and urine drug screening test were negative. The cTnI level was again found to be elevated in range of 0.31 - 0.34 ng/mL in three-set serials (< 0.30 ng/mL) (Table 1). His repeat EKGs (Fig. 1B) and echocardiogram (Fig. 2B) remained normal. One day later, patient became symptom-free with active surveillance and then discharged home.
In this case, patient had persistently elevated cTnI with normal renal function, without other medical conditions which may induce elevations in cTnI as previously reported in literature like myopericarditis, pulmonary embolism or drug abuse. Since ethanol intake has been reported to cause myocardial damage in susceptible patients [10], we postulated that chronic alcoholism may induce the elevations of cTnI in this patient. Short-term alcohol administration rarely produces heart muscle disease. However, long-term alcohol misuse or binge drinking can trigger cardiac dysfunction, termed alcoholic cardiomyopathy [10]. Alcoholic cardiomyopathy is characterized by cardiomegaly, disruption in myofibrillary architecture, reduced myocardial contractility, myocardial fibrosis as well as enhanced risk of stroke and hypertension [10, 11]. Alcoholic cardiomyopathy can present as left ventricular (LV) wall thickness and LV dilation in the echocardiogram, diastolic dysfunction and finally systolic dysfunction. In this case report, the patient had, however, no evidence of alcoholic cardiomyopathy based on his echocardiogram. We speculated that the mechanism of alcohol-induced cTnI elevation might be related to alcohol-induced myocyte injury, by direct oxidative damage, suppression of the protein synthesis and induction of apoptosis [12], leading to myocyte death, which causes very early myocardial damage, independent of alcoholic cardiomyopathy or any coronary artery disease. This hypothesis was supported by the findings that the myocardial content of cTnI was increased by approximately 40% whereas that of cTnT and cTnC remained unchanged in hearts from rats fed a diet containing alcohol for 16 weeks compared with pair-fed controls [13]. Further studies with larger numbers of patients are required to determine whether cTnI is a valid surrogate marker of cardiac involvement in patients with chronic alcoholism. In this case, even though patient had the abnormal elevated cTnI, cardiac catheterization was deemed unnecessary since patient had no any objective evidence of myocardial damage based on his EKGs, echocardiogram and SPECT pharmacological stress testing. The findings of this case report provide hypothesis for a prospective study on alcoholism and early detection of myocardial damage leading to alcohol-induced cardiomyopathy. In addition, further studies are needed to verify whether cTnI is a good predictor of the heart function in a long-term period in patients who have developed alcohol-induced cardiomyopathy. Conclusion cTnI has shown to be elevated in a variety of clinical scenarios without evidence of ACS. This is the first report suggesting that the abnormal elevations of cTnI can be seen in patients with chronic alcoholism without objective evidence of myocardial infarction. The mechanism of alcohol-induced cTnI elevation might be related to alcohol-induced early myocardial damage, unrelated to CAD, not detected by routine cardiac workup. Recognition of this will help clinicians minimize hospital stay and avoid unnecessary invasive investigations and therapeutic procedures. | ||||||||||||
| References | ||||||||||||
|
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.