| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 5, Number 9, September 2014, pages 486-487
Congenital Adrenal Hyperplasia: A Possible Risk Factor for Neonatal Adrenal Hemorrhage
Sota Iwatania, b, Emiko Takeokaa, Masami Mizobuchia, Seiji Yoshimotoa, Hideto Nakaoa
aDepartment of Neonatology, Hyogo Prefectural Kobe Children’s Hospital Perinatal Center, 1-1-1 Takakuradai, Suma-Ku, Kobe-Shi, Hyogo 654-0081, Japan
bCorresponding Author: Sota Iwatani, Department of Neonatology, Hyogo Prefectural Kobe Children’s Hospital Perinatal Center, 1-1-1 Takakuradai, Suma-Ku, Kobe, Hyogo 654-0081, Japan
Manuscript accepted for publication August 7, 2014
Short title: Congenital Adrenal Hyperplasia
doi: https://doi.org/10.14740/jmc1909w
| Abstract | ▴Top |
Here, we describe the first case of neonatal adrenal hemorrhage (AH) complicated with congenital adrenal hyperplasia (CAH). Our findings suggest that adrenal glands that have enlarged due to CAH are more susceptible to hemorrhaging during labor, and therefore, that CAH could be a risk factor for AH.
Keywords: Congenital adrenal hyperplasia; Adrenal hemorrhage; Ultrasound; Adrenal gland
| Introduction | ▴Top |
The etiology of adrenal hemorrhage (AH) is unknown, but the adrenal cortex at birth is relatively large, extremely vascular, and prone to trauma; venous engorgement has been proposed as a mechanism. Here, we demonstrate the first case of neonatal AH complicated with congenital adrenal hyperplasia (CAH).
| Case Report | ▴Top |
A 3,150 g newborn male was delivered after an uncomplicated pregnancy via vaginal delivery as the second child of unrelated healthy parents. His brother was healthy. At 3 h after birth, he was admitted for tachypnea and dusky skin discoloration. A physical examination revealed a right-sided abdominal mass. Abdominal ultrasound detected a large loculated collection of fluid in the right suprarenal region (Fig. 1A). The patient’s jaundice progressed rapidly despite intensive phototherapy, and a second ultrasound scan demonstrated that the fluid collection had reduced in size and exhibited mixed echogenicity (Fig. 1B). Abdominal computed tomography demonstrated a low-density lesion in the right suprarenal region (Fig. 2). These findings were consistent with a right AH. The left adrenal gland was enlarged (24.0 × 6.0 mm in size; normal mean size: 14.4 × 1.9 mm [1]) (Fig. 1C). Although the patient’s jaundice improved, his condition slowly deteriorated, and marked weight loss was observed. On the 10th day, a laboratory examination revealed hyponatremia (Na: 133 mEq/L) and hyperkalemia (K: 6.6 mEq/L). Furthermore, the patient’s serum 17-hydroxyprogesterone level was elevated (590 ng/dL). These results were indicative of the classical type of CAH due to 21-hydroxylase deficiency. Hydrocortisone treatment was initiated, and the patient’s condition improved markedly. He was discharged after being prescribed hydrocortisone and 9-alpha-fludrocortisone. Subsequently, mutations in the steroid 21-hydroxylase gene were detected.
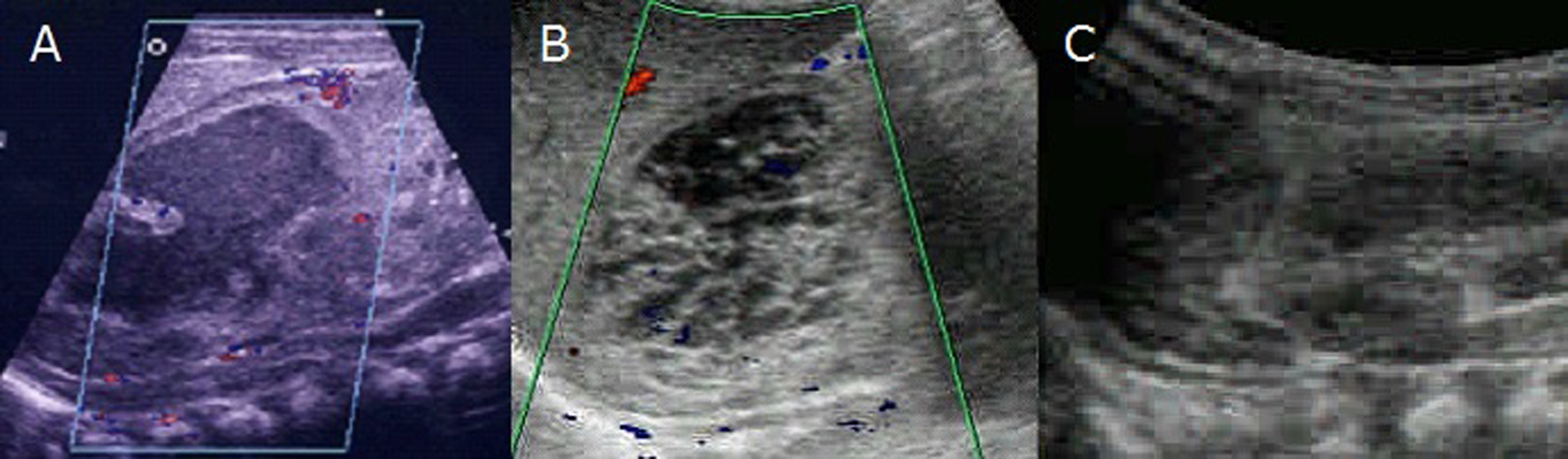 Click for large image | Figure 1. (A) Para-sagittal section through the partly liquefied right-sided adrenal hemorrhage on the day of admission. An examination of vascular flow did not detect any blood flow foci within the hemorrhagic region of the adrenal gland. (B) A follow-up examination performed at 3 days after birth demonstrated a reduction in the size of the right AH. (C) During the examination mentioned in B, it was also found that the left adrenal gland was enlarged (24.0 × 6.0 mm). |
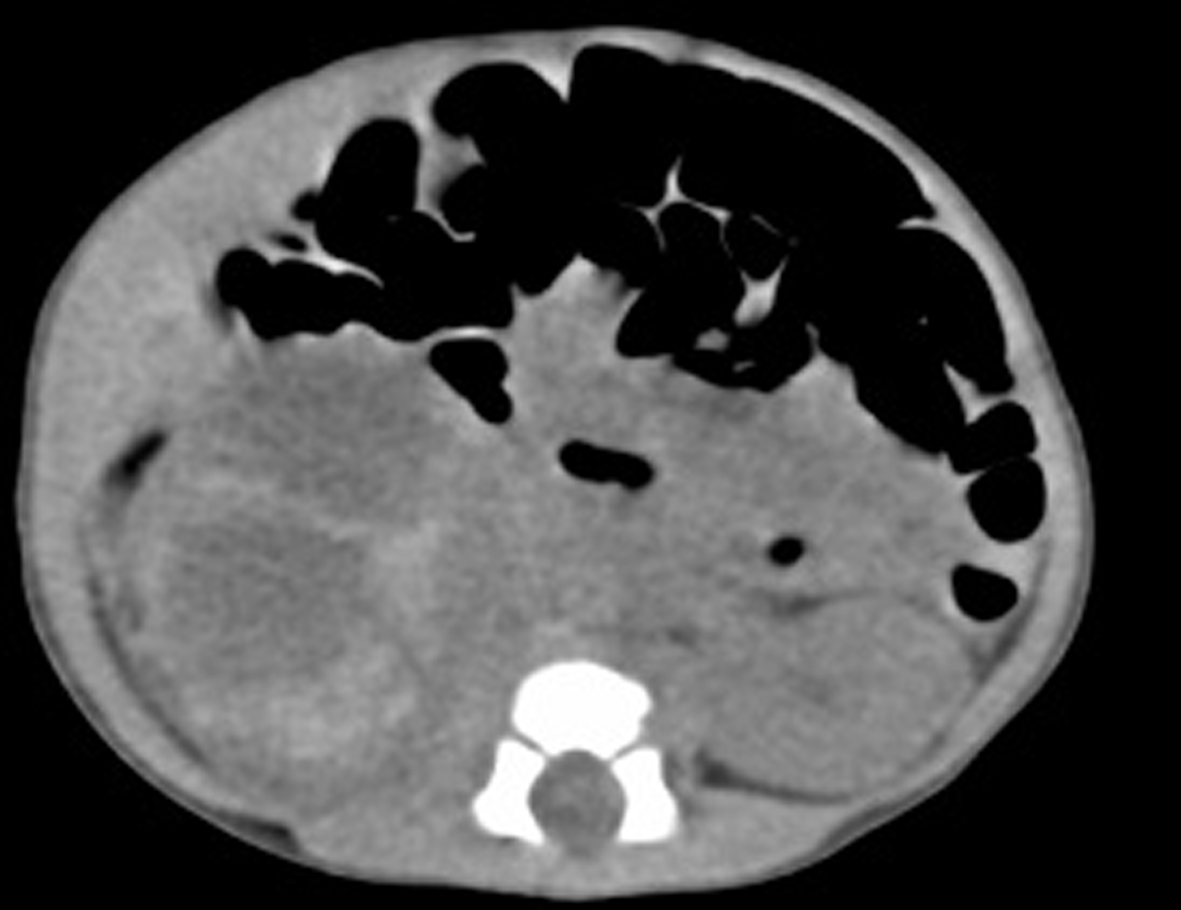 Click for large image | Figure 2. On the third day, abdominal computed tomography detected a lobulated low-density lesion in the right suprarenal region. |
| Discussion | ▴Top |
In neonates, the adrenal gland is vulnerable to hemorrhaging because of its large size and high vascularity [1]. AH is an uncommon condition in the neonatal period (incidence: 0.2%). It can be caused by a difficult labor [2]; however, in some cases its etiology is unknown [3]. The clinical features of AH are variable and non-specific [2]. AH rarely leads to transient adrenal insufficiency [2, 3]; however, no cases of AH complicated with CAH have been reported in the medical literature. We suggest that adrenal glands that have enlarged due to CAH are more susceptible to hemorrhaging during labor, and therefore, that CAH could be a risk factor for AH.
Acknowledgments
We thank the patient’s family for their kind cooperation and for giving us permission to publish this case report.
Author Contributions
Sota Iwatani M.D. and Emiko Takeoka M.D. contributed equally to this work.
Conflict of Interest
The authors have no conflicts of interest to declare.
| References | ▴Top |
- Westra SJ, Zaninovic AC, Hall TR, Kangarloo H, Boechat MI. Imaging of the adrenal gland in children. Radiographics. 1994;14(6):1323-1340.
doi pubmed - Mutlu M, Karaguzel G, Aslan Y, Cansu A, Okten A. Adrenal hemorrhage in newborns: a retrospective study. World J Pediatr. 2011;7(4):355-357.
doi pubmed - Koklu E, Kurtoglu S, Akcakus M, Koklu S. Adrenal haemorrhage with cholestasis and adrenal crisis in a newborn of a diabetic mother. J Pediatr Endocrinol Metab. 2007;20(3):441-444.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


