| |||||||||||
| Case Report | |||||||||||
| Volume 5, Number 10, October 2014, pages 532-534 | |||||||||||
Massive Pulmonary Embolism as a Complication of Coronary Angiography and Its Successful Treatment With Half-Dose Alteplase Orcun Gurbuza, d, Hakan Ozkanb, Abdulkadir Ercana, Gencehan Kumtepea, Ilker Hasan Karalc aDepartment of Cardiovascular Surgery, School of Medicine, Balikesir University, 10010 Balikesir, Turkey Manuscript accepted for publication August 27, 2014
A 64-year-old woman was admitted to our emergency room for shortness of breath, chest pain and syncope. Her symptoms started suddenly 2 hours before admission when she was resting at home. She had a history of coronary angiography 2 weeks ago and undergone surgical repair of femoral pseudoaneurysm. She was diagnosed with massive pulmonary embolism and successfully managed with half-dose alteplase and discharged with warfarin treatment 5 days after the admission. This case is presented in order to draw attention to this rare presentation and the use of half-dose systemic thrombolytic in a patient with a history of vascular surgery within 2 weeks. Keywords: Complication of coronary angiography; Pulmonary embolism; Half-dose systemic thrombolytic therapy
Invasive coronary angiography is still the gold standard test for identifying the presence and extent of coronary artery disease, despite promising improvement in non-invasive coronary imaging. As with any invasive procedure, it has well-known major and minor complications. Major complications such as death, emergency cardiac surgery, clinical myocardial infarction, and major bleeding or need for vascular surgery occur in less than 2% of the population [1]. The incidence of pseudoaneurysm after diagnostic angiography is reported between 0.5% and 2.0%. Ultrasound-guided non-surgical treatment is currently the first-line approach for iatrogenic femoral pseudoaneurysm unless it is too large [2]. Pulmonary embolism (PE) is rarely reported following coronary angiography [3, 4]. The pressure applied to the groin or repair of access site complications after coronary angiography may cause PE. According to US Food and Drugs Administration (FDA), 2-h systemic recombinant tissue plasminogen activator (rt-PA) 100 mg infusion is recommended for patients with massive acute PE [5]. However, systemic thrombolysis significantly increased major bleeding [6, 7]. Therefore, several studies were conducted to assess the efficacy and safety of low-dose rt-PA in the treatment of acute PE and reported favorable results [8, 9].
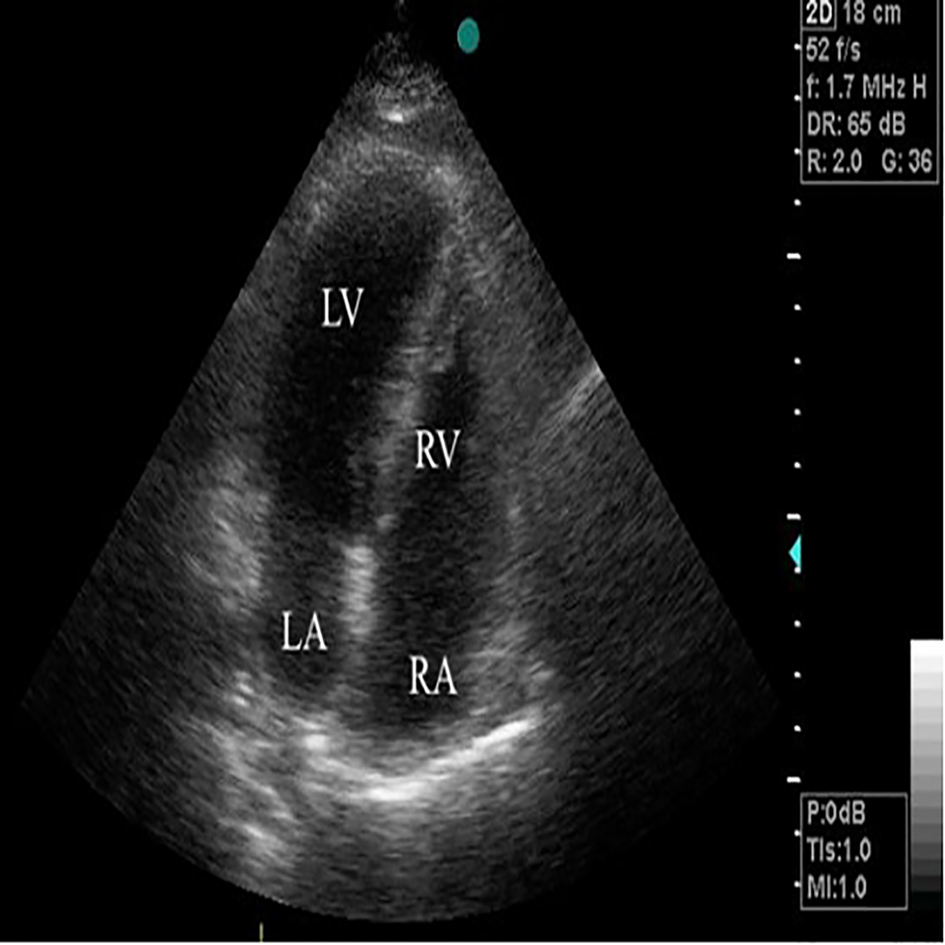
A 64-year-old woman was admitted to the emergency department for sudden onset of shortness of breath, chest pain and syncope. She had a coronary angiography in another hospital 2 weeks ago. Two days after her discharge, she had been rehospitalized to the same hospital due to swelling and pain in the right side groin area. Color Doppler ultrasound had identified a pseudoaneurysm of the right common femoral artery and surgical repair had been applied after the failure of ultrasonography-guided vascular compression therapy. Three days after her discharge she was admitted to the emergency department of our hospital with new-onset complaints of dyspnea, chest pain and syncope. On physical examination, she presented a moderate general status, with a blood pressure 80/50 mm Hg, pulse 126 beats/min, respiratory rate 30 breaths/min, and an oxygen saturation 84%. There were a 20 × 15 cm ecchymosis and a 4 cm femoral surgical incision in her right groin. Laboratory test revealed a D-dimer level of 3,900 ng/mL. The echocardiographic examination showed a large intracardiac thrombus with the expansion of the right heart chambers (Fig. 1, 2). Venous Doppler ultrasonography detected DVT in the left superficial femoral vein. Computed tomography of the chest revealed large thrombus in the main pulmonary artery.
A half-dose alteplase (50 mg), in contrast to classical treatment, was administered intravenously within 2 h. The patient’s oxygen saturation and blood pressure came to the normal levels within approximately 90 min after the initiation of treatment. The control echocardiography on the next day revealed the complete disappearance of the intracardiac thrombus and right heart dilatation (Fig. 3). The patient was carefully monitored for evidence of bleeding. Low molecular weight heparin (LMWH) and warfarin therapy were started on the second day. LMWH was continued until the INR reached 2.5. The patient had no serious complication after half-dose systemic rt-PA and was discharged with warfarin treatment 5 days after the admission.
As with any invasive procedure, coronary angiography has several complications such as death, emergency cardiac surgery, myocardial infarction, and major bleeding or need for surgical repair of vascular access [1]. The incidence of pseudoaneurysm after diagnostic angiography is reported between 0.5% and 2.0% [2]. Risk factors for the development of pseudoaneurysm include BMI ≥ 28 kg/m2, larger number of cases performed per day in a particular room, larger sheath sizes, and preprocedural platelet count < 200 × 109 L [1]. The main symptoms of femoral pseudoaneurysm are pain due to femoral nerve compression and extremity swelling secondary to venous compression which may also cause deep venous thrombosis. Acute PE is often fatal, with a mortality rate of approximately 30% unless treated as soon as possible after symptoms develop [10]. PE is rarely reported following coronary angiography [3, 4]. The pressure applied to the groin or access site complications such as hematoma or femoral pseudoaneurysm after coronary angiography may cause deep venous thrombosis which may lead to PE [3]. The recommended protocol for patients with massive acute PE or submassive PE with RV dysfunction is 100 mg rt-PA given during a 2-h infusion [5]. Transcatheter procedures or emergency surgical thrombectomy are recommended as an alternative to thrombolysis when there are contraindications for thrombolysis or when thrombolysis has failed. Recent surgery, depending on the territory involved, is not necessarily barrier to fibrinolysis [7]. However, systemic thrombolysis may increase bleeding associated with surgery [6, 7]. Recently, several studies were conducted to assess the efficacy and safety of low-dose rt-PA in the treatment of acute PE and reported similar efficacy but lower bleeding than standard dose of rt-PA [8, 9]. Considering patient clinical situation and for decreasing bleeding risk, we decided to administer 50 mg rt-PA. The thrombus in right heart chamber was resolved completely within a day and the patient’s health condition is back to normal within a day. In conclusion, we assume that the cause of PE in our patient was transient deep venous thrombosis due to inguinal hematoma or femoral pseudoaneurysm. Optimal placement of the arterial sheath, use of smaller sheaths, and careful manual compression with shorter period of immobilization, can significantly reduce the incidence of deep venous thrombosis and PE. Moreover, half-dose rt-PA may be safe and effective treatment alternative in patients with massive PE having high bleeding risk with systemic thrombolysis. Competing Interests The authors declare that they have no competing interests. Financial Disclosures This manuscript did not receive any financial aid. The authors have no disclosures regarding this manuscript. Author Contributions Orcun Gurbuz and Gencehan Kumtepe planned the study and the structure of the manuscript. Abdulkadir Ercan did the final English writing of the text. Hakan Ozkan participated and contributed to the evaluation of the case as the cardiologist. Ilker Hasan Karal aided in the collection of data from the literature. | |||||||||||
| References | |||||||||||
|
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.