| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 6, Number 7, July 2015, pages 287-289
Carcinomatosis Meningitis Presenting as Third Nerve Palsy
Avidesh Pandaya, d, Dale Maharajb, Robbie Rampersadc
aDepartment of Medicine, Eric Williams Medical Sciences Complex, Mt Hope, Trinidad, WI, Trinidad and Tobago
bDepartment of Surgery, St. Clair Medical Centre, St. Clair, POS, Trinidad and Tobago
cDepartment of Radiology, Eric Williams Medical Sciences Complex, Mt Hope, Trinidad, WI, Trinidad and Tobago
dCorresponding Author: Avidesh Panday, Department of Medicine, Eric Williams Medical Sciences Complex, Mt Hope, Trinidad, WI, Trinidad and Tobago
Manuscript accepted for publication May 11, 2015
Short title: Carcinomatosis Meningitis
doi: http://dx.doi.org/10.14740/jmc2149w
| Abstract | ▴Top |
Carcinomatosis meningitis is associated with 5-8% of patients with malignancy. The diagnosis is usually suspected in patients with known malignancy and based on clinical symptoms as well as supportive cerebrospinal fluid studies. We present a case of carcinomatous meningitis where no suspicion of malignancy was evident and where the clinical course and laboratory investigations were atypical for the diagnosis.
Keywords: Breast cancer; Leptomeningeal carcinomatosis; Visual loss; Cranial nerve palsy; Osteosclerotic
| Introduction | ▴Top |
We present a case of a pupil involving third nerve palsy as well as subtle features of meningism occurring acutely in a previously healthy lady as a result of carcinomatous meningitis. While carcinomatous meningitis is a known etiology of this, it is rarely the presenting manifestation and furthermore usually only suspected in patients with established cancer. This case highlights carcinomatous meningitis where no suspicion of malignancy was evident and where the clinical course and laboratory investigations were atypical for the diagnosis.
| Case Report | ▴Top |
A 67-year previously well female presented with a 2-day history of reduced visual acuity, intermittent diplopia as well as severe bifrontal headache. There was also a 2-month history of neck stiffness as well as a witnessed generalized tonic clonic convulsion 4 days prior to admission. There was no other significant past medical history and there was no other medication usage or significant family history. On examination, she was noted to have diplopia with a pupil involving right third nerve palsy as well as bilateral papilledema as well as reduced visual acuity with the OD 20/100, OS 20/80. Otherwise her mental status was normal with full orientation and cognitive function.
Her hospital course was complicated with significant fluctuating cognitive deficits as well as visual hallucinations but no further seizures were noted. Her visual acuity progressively worsened to appreciation to light only.
An initial MRI/angiogram/venogram revealed a communicating hydrocephalus with some mild diffuse cerebral vasospasm but no other abnormalities apart from some age white matter changes. A further MRI brain with gadolinium did not reveal any enhancement. The patient then went on to have a CT and conventional cerebral angiogram which showed no evidence of an aneurysm in the circle of Willis. An initial lumbar puncture was significant for an opening pressure of 41 mm H2O. Two subsequent repeat cerebrospinal fluid (CSF) studies showed normalization of the opening pressure with elevated protein at 280 - 310 mg/dL with low CSF glucose 20 - 33 mg/dL. Apart from RBCs no other cells were noted on cytology at each lumbar puncture. The patient was HIV and VDRL negative and repeated septic screens were negative. Additionally HSV 1 and 2 titres within the CSF were negative. An autoimmune screen inclusive of ANA, dsDNA as well as inflammatory markers inclusive of CRP and ESR was normal. Apart from mild slowing of the background, there was no focal slowing or epileptiform activity on multiple EEGs.
A contrast enhanced CT abdomen, pelvis and chest did not reveal any organomegaly or masses but multiple mixed predominantly osteosclerotic lesions were noted in the pelvis as well as thoracic vertebrae (Fig. 1). A mammogram revealed a mass in the right breast which after biopsy revealed a mixture of intra-ductal as well as invasive carcinoma (Fig. 2).
 Click for large image | Figure 1. Multiple osteosclerotic lesions within the thoracic vertebral bodies. |
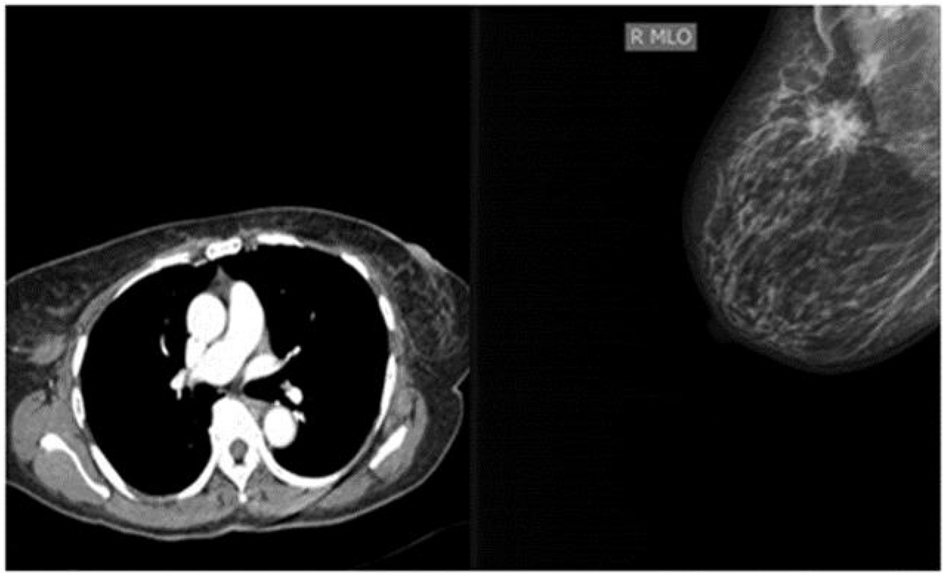 Click for large image | Figure 2. Right breast nodule shown on CT chest as well as on mammogram. |
| Discussion | ▴Top |
Leptomeningeal carcinomatosis occurs in approximately 5-8% of patients with malignancy with the most common cancers being breast, lung as well as melanomas [1, 2]. This is also seen with less frequency in certain lymphomas and leukemias. Cancer cells are thought to reach the meninges by hematogenous or lymphatic spread by growing around and along the nerve and blood vessel [2] with subsequent dissemination along the neuroaxis via CSF flow [1].
Carcinomatous meningitis has a wide array of presentations with cerebral (38%), cranial nerve (45%), spinal nerves (48%) as well as limb weakness (38%) being the most common. While bilateral visual loss is not a common presentation, the patient presented with multiple cranial neuropathies inclusive of subacute progressive bilateral visual loss as well as a third nerve involvement. While progressive bilateral visual loss is noted in carcinomatous meningitis, its mechanism is not well defined with vascular insufficiency in association with tumor cuffing of the optic nerve sheath, neuronal toxins or unknown mechanisms potential mechanisms. In our case, the raised intracranial pressure may have been contributory; however, sequential lumbar punctures revealed normal opening pressures yet there was progressively worsening visual loss.
The diagnosis of carcinomatosis meningitis proved challenging. The patient had a 2-month history of meningism but there was no clinical, laboratory or radiological evidence of infection. Subarachnoid bloods were considered but repeat CT angiography as well as conventional cerebral angiogram failed to reveal any aneurysms and repeat CSF studies did not reveal any evidence of SAH. Given the fluctuating cognitive changes, history of seizures, presumed infiltration of the third cranial nerve, non-specific white matter lesions and the patient being of Afro-Caribbean Ancestry, an infiltrative condition was considered such as SLE cerebritis but all inflammatory markers were negative as well as serial EEG. Similarly neurosarcoidosis was considered but again not in keeping with the typical presentation.
The absence of positive cytology certainly proved a confounding factor in the diagnosis as [3] CSF studies failed to show abnormal cells. However, persistently elevated protein and low glucose were noted. While the diagnosis of leptomeningeal carcinomatosis hinges on the presence of abnormal CSF cytology, with 73-90% of patients having abnormal cells on initial tap [2], there can be persistently negative cytology in 10% of patients [3]. Otherwise the biochemical analysis was within the range of that seen in leptomeningeal carcinomatosis.
As with the CSF studies, the diagnosis of the primary tumor was not straightforward. A CT abdomen, pelvis and chest did not reveal any abnormal masses or organomegaly but multiple mixed osteolytic but predominantly osteosclerotic lesions were noted in the thoracic vertebrae. While it is well known that bone metastases from breast cancer are predominantly osteolytic [4], there has been an increasing prevalence of mixed and osteosclerotic lesions.
Conclusion
This case highlights the neurological manifestations of breast cancer as well as its temporal association with the diagnosis as it predated the clinical diagnosis of cancer in our patient. Additionally the patterns of bone metastases were not typical in this case with the manifestations of osteosclerotic lesions. It also serves to highlight carcinomatous meningitis as a case of a pupil involving third nerve palsy.
| References | ▴Top |
- Grossman SA, Krabak MJ. Leptomeningeal carcinomatosis. Cancer Treat Rev. 1999;25(2):103-119.
doi pubmed - Jayson GC, Howell A. Carcinomatous meningitis in solid tumours. Ann Oncol. 1996;7(8):773-786.
doi - Teare JP, Whitehead M, Rake MO, Coker RJ. Rapid onset of blindness due to meningeal carcinomatosis from an oesophageal adenocarcinoma. Postgrad Med J. 1991;67(792):909-911.
doi pubmed - Quattrocchi CC, Piciucchi S, Sammarra M, Santini D, Vincenzi B, Tonini G, Grasso RF, et al. Bone metastases in breast cancer: higher prevalence of osteosclerotic lesions. Radiol Med. 2007;112(7):1049-1059.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


