| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 2, Number 4, August 2011, pages 156-158
Internal Juguler Vein Trombosis as an Initial Presentation of Signet-Ring Cell Adenocarcinoma of Unknown Origin
Gediz Murat Serina, e, Abdullah Soydan Mahmutoglub, Şenol Polatc, Elif Aksoyd, Hasan Tanyeric
aAcıbadem Health Care Group, Bakırköy Hospital, Department of Otorhinolaryngology, Istanbul, Turkey
bBaskent University Istanbul Hospital, Department of Radiology, Istanbul, Turkey
cAcıbadem University, Medical Faculty, Department of Otorhinolaryngology, Istanbul, Turkey
dAcıbadem Health Care Group, Maslak Hospital, Department of Otorhinolaryngology, Istanbul, Turkey
eCorresponding author: Acıbadem Health Care Group, Bakırkoy Hospital, Department of Otorhinolaryngology, Halit Ziya Uşaklıgil Cad. No:1, Bakırkoy 34140 Istanbul, Turkey
Manuscript accepted for publication May 26, 2011
Short title: Internal Juguler Vein Trombosis of Adenocarcinoma
doi: https://doi.org/10.4021/jmc225w
| Abstract | ▴Top |
Internal jugular vein (IJV) thrombosis is a rare entity. Cases of IJV thrombosis associated with malignancy have been reported. Signet-ring cell adenocarcinoma is a unique subtype of mucin-producing adenocarcinoma that usually develops in the gastrointestinal tract. We report signet-ring cell adenocarcinoma (SRCAC) presented initially with an IJV thrombosis prior to the discovery of the neoplasm.
Keywords: Internal juguler vein; Thrombosis; Signet-ring cell adenocarcinoma
| Introduction | ▴Top |
Internal jugular vein (IJV) thrombosis is a rare entity. Drug abuse, trauma and venous catheterization are the most common causes of IJV thrombosis [1, 2]. IJV thrombosis is less commonly seen secondary to malignancies, infection, hypercoagulopaty conditions, functional neck dissections and ovarian hyperstimulation syndrome [2-5]. It may also occur spontaneously.
We describe signet-ring cell adenocarcinoma (SRCAC) presented initially with an IJV thrombosis.
| Case Report | ▴Top |
A 41-year-old man attended to an emergency unit with neck pain, nausea and fatique and discharged after non-spesific treatment. The following day, he fainted at an international airport after a three hours flight. He was taken to the nearest hospital and discharged again on the same day without any spesific diagnosis. The next day, he attended to our otolaryngology department with the same complaints. Due to the neck pain and the history of faint, ultrasonography of the neck was performed. Ultrasonography revealed left IJV thrombosis. The patient was hospitalized and immediately heparinized using low moleculer weight heparine. Routine blood tests were done and they were within normal limits. Neck, thorax and abdominal computed tomography (CT) and neck, thorax CT angiography were performed. CT angiography showed thrombosis of the left jugular vein including to the subclavian vein (Fig. 1a, b). The abdominal CT showed perigastric, mesenteric and retroperitoneal paraaortic multiple enlarged lymph nodes. No abnormalities of the gastrointestinal tract were identified on imaging or endoscopy. Laparoscopic evaluation of the intraabdominal lymph nodes was performed. Histopathological findings showed metastasis of SRCAC. With the diagnosis of SRCAC metastasis of unknown origin, the patient underwent appropriate chemotherapotical treatment and he died eight months after the initial diagnosis.
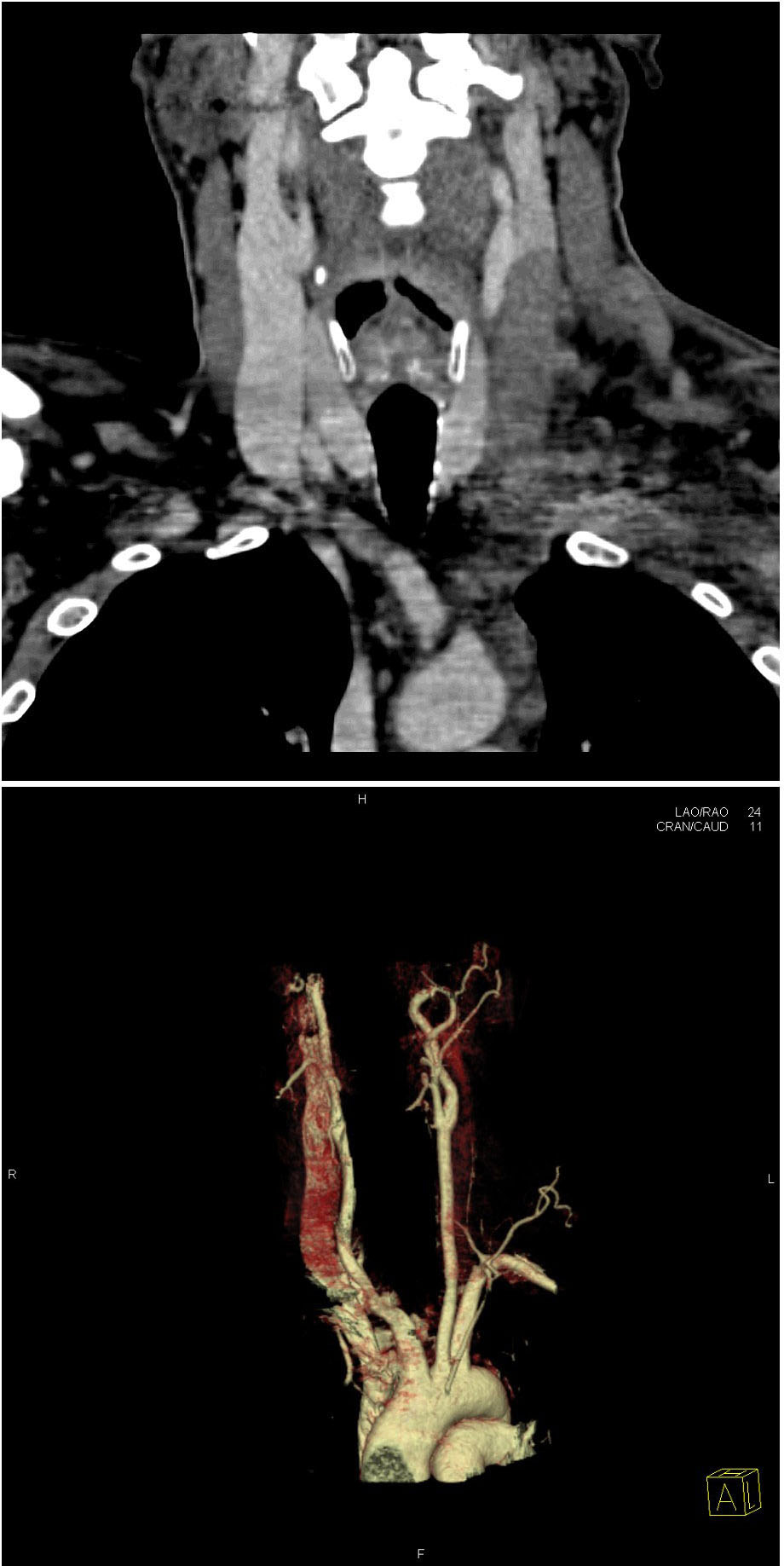 Click for large image | Figure 1. (a, b). CT angiography showed thrombosis of the left jugular vein. |
| Discussion | ▴Top |
The diagnosis of IJV trombosis can be overlooked. Clinical manifestations such as neck pain with or without a tender swelling in the neck can be misleading. Without a particular previous history of some predisposing factors of IJV trombosis, such as drug abuse, venous catheterization or trauma, a clinician has to be suspicious to diagnose IJV thrombosis.
SRCAC is a unique subtype of mucin-producing adenocarcinoma that usually develops in the gastrointestinal tract. However, it is infrequently seen in other organs such as the lung, thyroid and prostate. In general, the prognosis is poor for patients with adenocarcinoma of unknown primary, and it is difficult to select the optimal type of chemotherapy [6-8].
Several cases of IJV thrombosis associated with malignancy have been also reported [3]. This case illustrated an unusual presentation of a rare condition. After several diagnostic tests, and eliminating the other probable causes we came to the conclusion that the cause of IJV trombosis was malignancy according to histopathological findings of abdominal lymph nodes. Malignant neoplasms can be associated with IJV trombosis through two mechanisms. This may occur from a primary or metastatic local tumor mass obstructing the jugular blood flow by compression to result in stasis and thrombosis or even direct invasion into the vein. In our case, ultrasonography revealed multiple lymph nodes around the IJV showing no sign of compression to the vein. This apperance could also result from a migratory thrombophlebitis known to occur in association with various malignancies [9]. The pathophysiology is postulated to be a hypercoagulable state related to elevated levels of factor VIII and accelerated production of thromboplastin [10].
Lieberman et al. reported the correlation between thrombophlebitis and cancer in a group of 81 patients [9]. Thrombophlebitis was recognized prior to the discovery of the neoplasm in 60% of the patients. Metastatic adenocarcinoma induces a migratory thrombophlebitis secondary to the hypercoagulable state of cancer. Therefore, thrombophlebitis may be the first indication that an occult neoplasm is present [9, 10].
This case demonstrated an unusual presentation of a rare condition. Every patient with thrombophlebitis must undergo a careful history, a complete physical examination, and a thorough investigation to avoid misdiagnosis of an ocoult malignancy. Clinicians should be alert of such pathology in similar patients, in order to ensure early investigations and treatment of primary disease.
| References | ▴Top |
- Cohen JP, Persky MS, Reede DL. Internal jugular vein thrombosis. Laryngoscope. 1985;95(12):1478-1482.
pubmed doi - Chowdhury K, Bloom J, Black MJ, al-Noury K. Spontaneous and nonspontaneous internal jugular vein thrombosis. Head Neck. 1990;12(2):168-173.
pubmed doi - Pata YS, Unal M, Gulhan S. Internal jugular vein thrombosis due to distant malignancies: two case reports and literature review. J Laryngol Otol. 2008;122(3):318-320.
pubmed doi - De Sena S, Rosenfeld DL, Santos S, Keller I. Jugular thrombophlebitis complicating bacterial pharyngitis (Lemierre's syndrome). Pediatr Radiol. 1996;26(2):141-144.
pubmed - Martinelli I, Cattaneo M, Panzeri D, Taioli E, Mannucci PM. Risk factors for deep venous thrombosis of the upper extremities. Ann Intern Med. 1997;126(9):707-711.
pubmed - Akamatsu S, Takahashi A, Ito M, Ogura K. Primary signet-ring cell carcinoma of the urinary bladder. Urology. 2010;75(3):615-618.
pubmed doi - Sakai Y, Kanomata N, Itami H, Kajimoto K, Sakuma T, Ohbayashi C. Signet-ring cell carcinoma of the stomach metastasizing to renal cell carcinoma: a case report and review of the literature. Kobe J Med Sci. 2010;55(6):E122-131.
pubmed - Veit JA, Reichelt U, Tesche S. Signet ring cell adenocarcinoma of the oropharynx: presentation of a rare case and review of the literature. Auris Nasus Larynx. 2009;36(6):717-720.
pubmed doi - Lieberman JS, Borrero J, Urdaneta E, Wright IS. Thrombophlebitis and cancer. JAMA. 1961;177(542-545.
pubmed - Amundsen MA, Spittell JA, Jr., Thompson JH, Jr., Owen CA, Jr. Hypercoagulability associated with malignant disease and with the postoperative state. Evidence for elevated levels of antihemophilic globulin. Ann Intern Med. 1963;58(608-616).
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


