| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 7, July 2016, pages 286-290
A Case of Bilateral Ectopic Pregnancy Following Intra-Uterine Insemination
Wen Shan Sima, c, Elis Yuexian Leeb, Pamela Yu Fen Tana
aDepartment of Obstetrics & Gynecology, KK Women’s and Children’s Hospital, Singapore
bYong Loo Lin School of Medicine, National University of Singapore, Singapore
cCorresponding Author: Wen Shan Sim, Department of Obstetrics & Gynecology, KK Women’s and Children’s Hospital, 100, Bukit Timah Road, Singapore 229899, Singapore
Manuscript accepted for publication April 18, 2016
Short title: Bilateral Ectopic Pregnancy
doi: http://dx.doi.org/10.14740/jmc2484w
| Abstract | ▴Top |
We describe a case of a 31-year-old lady with primary subfertility who conceived only after her third intra-uterine insemination. She was diagnosed to have a right ectopic pregnancy which failed methotrexate treatment. Diagnostic laparoscopy confirmed bilateral ectopic pregnancies. A review was conducted for any consensus reached on diagnosis and optimal management of bilateral ectopic pregnancies after artificial reproductive techniques (ARTs). A search on Pubmed was carried out for publications in peer-reviewed journals with the following keywords: bilateral tubal ectopic pregnancy, heterotopic. Ten suitable publications were retrieved. Bilateral tubal ectopic pregnancy is rare, often missed on radiology and an unexpected finding at surgery. There should be a high index of suspicion for bilateral ectopic pregnancies after ART. Poor correlation with B-hCG levels further confuses diagnostic accuracy. It is prudent to ensure accurate diagnosis of bilateral ectopic pregnancies and appropriate intervention to reduce morbidity and mortality. Salpingostomy should be considered in patients with subfertility to preserve the possibility of future pregnancies.
Keywords: Artificial reproductive techniques; Bilateral tubal ectopic pregnancy; Heterotopic
| Introduction | ▴Top |
Artificial reproductive techniques (ARTs) have helped infertile couples worldwide to have children which otherwise would not have been possible. Though these new technologies provide hope and possibilities, complications of ART including ectopic pregnancies are on the rise. Ectopic pregnancies remain to be one of the main causes of maternal death and morbidity in modern obstetrics, with a majority of these deaths associated with substandard care. Bilateral ectopic pregnancies are a rare clinical condition as a result of ART. No consensus had been reached on the diagnosis and management of bilateral ectopic pregnancies after ART because of its rarity. The following case report aimed to report the definite possibility of bilateral ectopic pregnancies from ART, highlight the difficulties in diagnosis and touch on ethical considerations in management.
| Case Report | ▴Top |
She was first seen in 2012. She was 29 years old and trying to conceive for 3 years. She had no previous pregnancies. She had a known medical history of hypothyroidism on thyroxine 100 μg once a day. She reported regular periods at an interval of 28 - 30 days affected by dysmenorrhea. Her husband was a healthy 36-year-old man who smoked 1 - 2 sticks per day. She had been on a trial of ovulation induction medication for 6 - 7 cycles in India with no success.
A hysterosalpingogram was performed which showed a right hydrosalpinx with loculated spill. The left fallopian tube showed intra-peritoneal spillage. Her pelvic ultrasound was normal and her anti-Mullerian hormone (AMH) level was 8.3 ng/mL. Her husband’s sperm analysis revealed mild hypospermia and teratozoospermia. Intra-uterine insemination (IUI) with letrozole was offered and insemination was performed on day 15 of the cycle with one mature follicle. It was unsuccessful.
The couple proceeded to have a diagnostic laparoscopy in India. Intra-operative findings were that of a clean pelvis with a patent right tube and a spasmic left tube. The couple underwent a second IUI attempt in July 2013 with ovulation induction by follicular stimulating hormone (Puregon). Three follicles more than 16 mm were seen on the ultrasound. She conceived after the procedure but miscarried during the first trimester.
A third IUI was performed in December 2014 after ovarian stimulation with follicular stimulating hormone (Puregon) timed with the production of two mature follicles on follicular tracking. Her hCG level 17 days after procedure was 273.3 IU/L.
She presented to the emergency unit 3 weeks after IUI with per vaginal spotting. A pelvic ultrasound showed an empty uterus with no adnexal mass. B-hCG level was 2,858 IU/L. Her second B-hCG reading 48 h later suboptimally increased to 4,123.2 IU/L. A pelvic ultrasound was repeated which revealed a 1.3 × 0.7 × 0.7 cm ring-like structure containing a central cystic space with a tiny yolk sac suggestive of a right ectopic pregnancy. Options of conservative management, surgery or IM methotrexate were conveyed to the patient. Patient chose the latter and 90 mg of IM methotrexate was administered.
Four days after methotrexate treatment, pelvic ultrasound showed the mass to be 1.3 × 1.3 × 1.1 cm. No free fluid was seen. B-hCG was 6,847.5 IU/L. Patient declined any intervention at this point.
Six days later, she returned to the emergency unit with clinical features of an acute abdomen. Pelvic ultrasound showed free fluid in the pelvis and a 1.7 × 1.7 cm mass in the right adnexa. She proceeded to have a diagnostic laparoscopy performed in view of the hemoperitoneum suggesting a ruptured ectopic pregnancy. A summary of her clinical presentation, B-hCG trend and radiological findings is provided in Table 1.
 Click to view | Table 1. Summary of B-hCG Levels and Radiological Findings After IUI |
Diagnostic laparoscopy revealed 50 mL of hemoperitoneum with a large 5 cm right ectopic pregnancy. Right salpingectomy was performed. The left fallopian tube appeared abnormally dilated of 3 cm in diameter with a dusky hue and a phimosed end, visually suspected to be a left tubal ectopic pregnancy (Fig. 1). Both ovaries were normal. The husband was consulted in view of the unexpected surgical findings. Given the background of a previous diagnostic laparoscopy in Indian showing a spasmic left tube, the options of conservative management till findings were conveyed to the patient, and left salpingostomy or salpingectomy were offered. It was discussed with the husband that since the left tube may be unhealthy, leaving it behind may risk further ectopic pregnancies and compromise future plans for in vitro fertilization. It was then decided that a left salpingectomy was to be performed. The tubes were removed and labeled separately. Histopathology returned as bilateral tubes with products of conception in keeping with bilateral ectopic pregnancy.
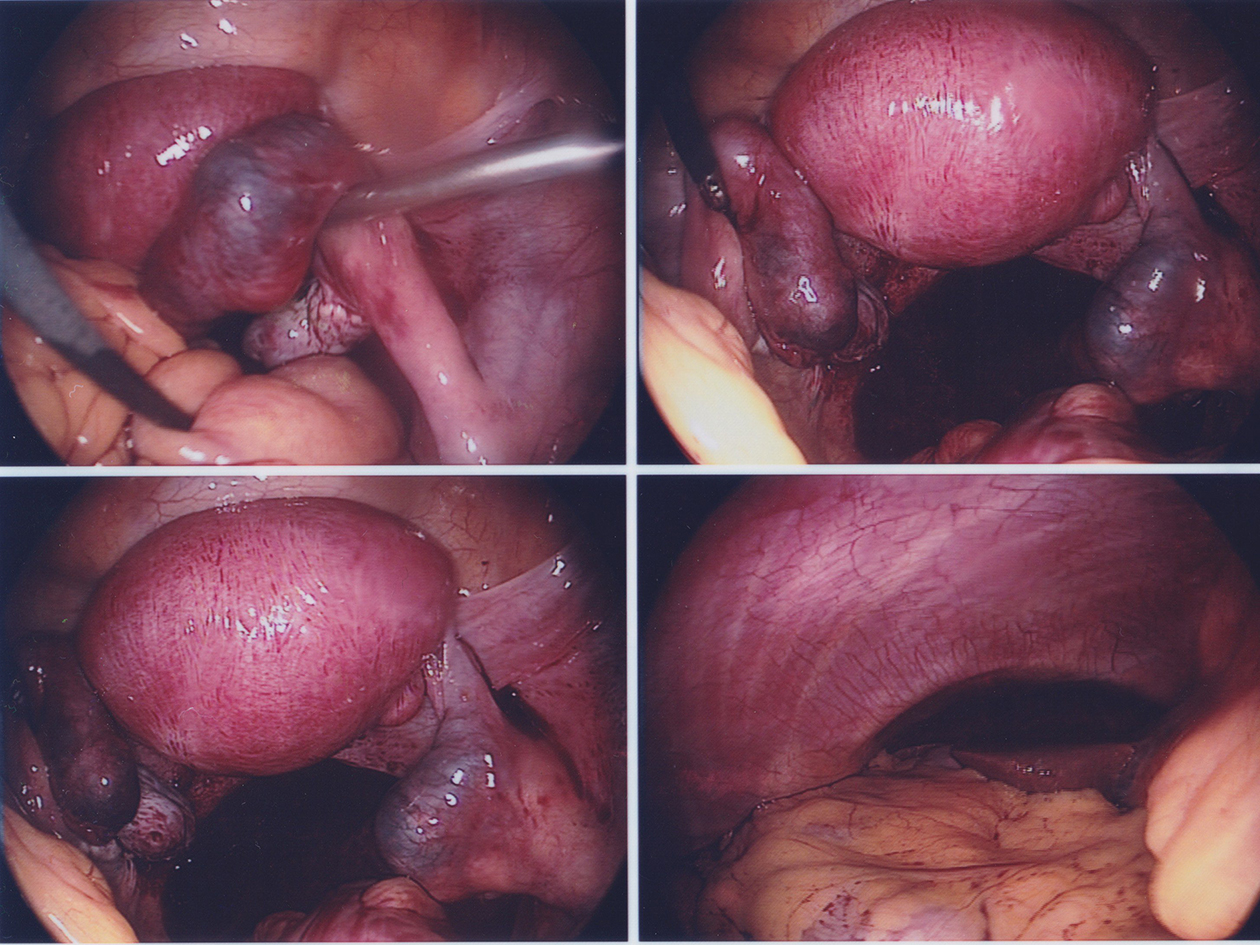 Click for large image | Figure 1. (Clockwise from top right) Right ectopic pregnancy; left tube with phimosed end likely ectopic pregnancy; hemoperitoneum from ruptured right ectopic pregnancy; view of the normal liver. |
| Discussion | ▴Top |
With the increasing use of ARTs, the incidence of ectopic and heterotopic pregnancies has been on the rise. Bilateral ectopic pregnancy is a rare clinical condition with an estimated prevalence of 1/200,000 spontaneous tubal pregnancies [1]. The prevalence is believed to be even higher in pregnancies by ART [2]. Several case reports had been published with regard to bilateral ectopic pregnancies, mostly post-ART [1-10].
Ectopic pregnancies remain to be one of the main causes of maternal death and morbidity in modern obstetrics. It is prudent to ensure early diagnosis of bilateral ectopic pregnancies with the view of early intervention to reduce morbidity and mortality for these women [9], as well as strike a balance between definitive management and future plans for conception as women who use ART are mostly those that have difficult conceiving.
Despite the number of case reports that have been published, no consensus had been reached on the diagnosis and management of bilateral ectopic pregnancies after ART. The importance of diagnosing bilateral ectopic pregnancies prior to surgical intervention could enhance pre-operative counselling in terms of suitability of tubal conservation or the need for bilateral salpingectomies as this could change the future reproductive performance of the patient.
A search of Pubmed was carried out, not restricted by language, for publications in peer-reviewed journals with the following keywords: bilateral tubal ectopic pregnancy, heterotopic, assisted reproductive techniques. Ten suitable publications, reporting a total of 11 cases, were retrieved [1-10] (Table 2).
 Click to view | Table 2. Summary of Case Reports in Terms of Their Methods of Diagnosis as Well as Subsequent Management |
We attempt to summarize the case reports in terms of their methods of diagnosis as well as subsequent management in Table 2.
There are a few learning points gathered from the 10 similar cases that we have summarized in Table 2.
1) Bilateral ectopic pregnancies are often missed on radiological investigations and are often an unexpected finding on laparoscopy/laparotomy [4, 8, 10].
2) Extremely high B-hCG levels have poor correlation with the final diagnosis of bilateral ectopic pregnancies [1], although differentials of bilateral ectopic pregnancies should be considered on top of other conditions such as a molar pregnancy [3].
3) There should be a high index of suspicion for bilateral ectopic pregnancies after pregnancies conceived after ART for both clinicians and radiologists [5], including pregnancies arising from clomiphene citrate [6, 7].
4) For pregnancies after ART with a diagnosed unilateral ectopic pregnancy going for surgery, a close inspection at the contralateral tube [8] during laparoscopy/laparotomy is crucial as ultrasonography for early ectopic pregnancies may be difficult [4].
5) Salpingostomy should be considered for unruptured bilateral ectopic pregnancies [9] in patients with history of subfertility to preserve the possibility of future pregnancies. Patients should be counselled on the pros and cons of salpingostomy which include need for longer follow-up for persistent trophoblastic disease as well as recurrent ectopic pregnancies.
From our case study, we also extrapolated that failed methotrexate treatment in an ectopic pregnancy which arises after ART may signify the possibility of bilateral ectopic pregnancy. This information should be provided to the radiologist or sonographer so that a closer look at the contralateral tube can be performed [5, 8, 9].
Conclusion
Ectopic pregnancy is a gynecological emergency. Due to the use of assisted reproductive techniques, the incidence of bilateral ectopic pregnancies is on the rise. It is often only diagnosed during laparoscopy [4], as it may be missed on transvaginal sonography. Beta-hCG trends can be misleading [1]. No consensus has been reached with regard to diagnosis and management of bilateral tubal ectopic pregnancies. Salpingostomy should be considered for unruptured bilateral ectopic pregnancies [9] in patients with history of subfertility to preserve the possibility of future pregnancies. Successful conception is still possible in the future with IVF treatment, even in patients who underwent bilateral salpingectomies [1]. Future studies can look into how to enhance diagnosis of bilateral ectopic pregnancies pre-operatively, so as to optimize management of this condition. Ethical considerations include obtaining valid consent for management of an unexpected finding of a bilateral ectopic pregnancy during surgery which will impact on a woman’s future reproductive performance. We believe that this case would add value to the growing literature on bilateral ectopic pregnancies following ARTs.
Conflicts of Interest
The authors have no conflicts of interest relevant to this article.
| References | ▴Top |
- Polat M, Boynukalin FK, Yarali I, Yarali H. Bilateral ectopic pregnancy following ICSI. BMJ Case Rep. 2014;2014.
- Kovachev E, Kozovski I, Ivanov S, Kornovski Y, Mircheva N, Koleva P, Tsonev A, et al. [A case of bilateral tubal pregnancy after IVF - ET]. Akush Ginekol (Sofiia). 2013;52(4):33-37.
- Arab M, Neda Kazemi S, Vahedpoorfard Z, Ashoori A. A rare case of bilateral ectopic pregnancy and differential diagnosis of gestational trophoblastic disease. J Reprod Infertil. 2015;16(1):49-52.
pubmed - Zhu B, Xu GF, Liu YF, Qu F, Yao WM, Zhu YM, Gao HJ, et al. Heterochronic bilateral ectopic pregnancy after ovulation induction. J Zhejiang Univ Sci B. 2014;15(8):750-755.
doi pubmed - Jamilian M. Bilateral tubal ectopic pregnancy following intra uterine insemination (IUI): A case report. Iran J Reprod Med. 2014;12(2):155-158.
pubmed - Terzic MM, Bila JS, Pilic IZ, Kocijancic DM. Bilateral ampulary pregnancy after clomifen citrate and intrauterine insemination - a unique case report. Gynecol Endocrinol. 2013;29(6):619-621.
doi pubmed - Pehlivanov BK, Amaliev GI, Malinova ML, Amaliev IG. Bilateral simultaneous isthmic ectopic pregnancy after clomiphene induction. Folia Med (Plovdiv). 2012;54(4):78-79.
doi - Ghaffari F, Eftekhari Yazdi P, Kiani K. A case report of bilateral tubal ectopic pregnancy following day 5 embryo transfer. Arch Med Sci. 2011;7(6):1087-1088.
doi pubmed - Altinkaya SO, Ozat M, Pektas MK, Gungor T, Mollamahmutoglu L. Simultaneous bilateral tubal pregnancy after in vitro fertilization and embryo transfer. Taiwan J Obstet Gynecol. 2008;47(3):338-340.
doi - Yarali H, Bukulmez O, Gurgan T. Combined bilateral ectopic and intrauterine pregnancy following ovulation induction with the low-dose step-up protocol in a patient with polycystic ovary syndrome. Arch Gynecol Obstet. 2000;264(1):37-38.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


