| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 6, June 2016, pages 213-215
An Unusual Case of Femoral Hernia
Darren J. Portera, b, Jane Kilkennya, Zorica Vujovica
aNinewells Hospital and Medical School, Dundee, Scotland, UK
bCorresponding Author: Darren J. Porter, Ninewells Hospital and Medical School, Dundee, Scotland, UK
Manuscript accepted for publication April 25, 2016
Short title: Unusual Femoral Hernia
doi: http://dx.doi.org/10.14740/jmc2499w
| Abstract | ▴Top |
The French surgeon Rene Jacques Croissant de Garengeot first described the presence of an appendix in a femoral hernia sac in 1731. We present the case of a 75-year-old lady with an incarcerated right femoral hernia which contained an appendix vermiformis. The treatment of choice of this rare disease entity is emergency surgery with simultaneous appendicectomy and repair of the femoral hernia. Suture repair or mesh repair can be used, the choice of which depends on surgeon preference, the age of the patient and the intra-operative findings (size of the hernia and the macroscopic appearance of the appendix).
Keywords: Femoral hernia; De Garengeot’s hernia; Appendicectomy
| Introduction | ▴Top |
The presence of the vermiform appendix in a femoral hernia sac was first described by Rene Jacques Croissant de Garengeot in 1731 and has become known as de Garengeot’s hernia [1]. It is an incidental finding occurring in 0.9% of femoral hernia repairs [2]. An inflamed appendix is an even rarer finding, with an incidence of 0.08-0.13% [3].
De Garengeot’s hernia is a very rare clinical presentation. It is more common in females than in males, but this probably reflects the increased incidence of femoral hernias in female patients [3].
Pre-operative diagnosis of de Garengeot’s hernia is difficult and when present, it requires emergency surgery.
We report a case of incarcerated femoral hernia occurring in a 75-year-old lady with a non-inflamed appendix contained within the hernia sac.
| Case Report | ▴Top |
A 75-year-old lady was admitted via the emergency department with a 5-month history of right groin swelling that had become painful in the 24 h prior to admission. There was no associated abdominal distension, no vomiting, no constipation, no fever, no anorexia and no systemic upset.
The patient had a background medical history of bronchiectasis, and her only surgical history was a vaginal hysterectomy performed 4 years prior to presentation.
Of note, the patient had recently attended her GP regarding the groin lump and an ultrasound of her right inguinal region had been performed (Fig. 1). She was awaiting review at surgical clinic. The patient did admit to significant weight loss in the 6 months leading up to admission.
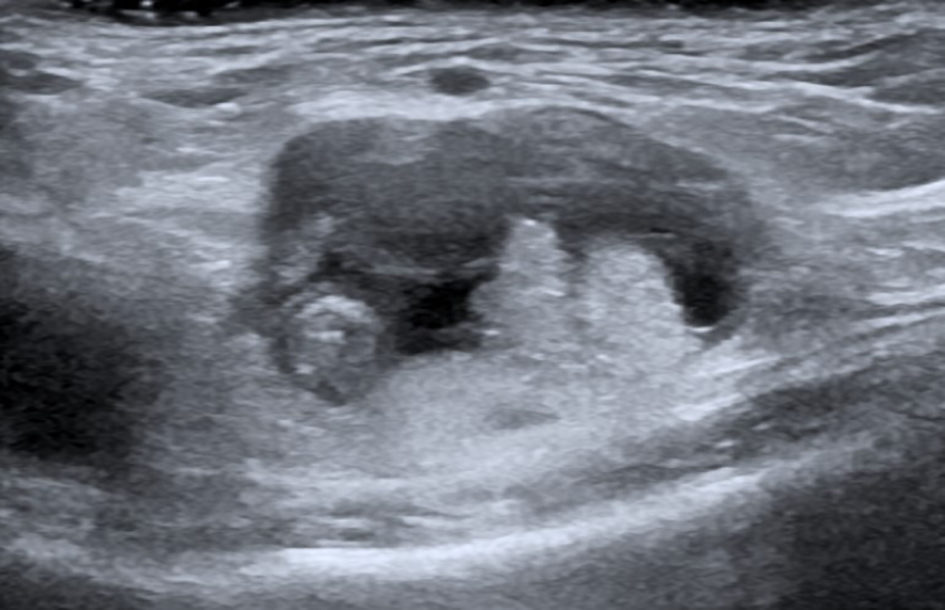 Click for large image | Figure 1. Ultrasound scan of the right inguinal region demonstrating a femoral hernia, evidenced by small bowel loops and fluid within the right femoral canal. |
On examination, the patient appeared clinically well, although there was evidence of recent weight loss. Admission observations were unremarkable; in particular, there was no tachycardia and the patient was apyrexic.
Abdominal examination revealed no surgical scars and no abdominal distension. There was a 3 cm in diameter hard lump in the right groin, which was tender, irreducible with a negative cough impulse and no overlying skin changes. Percussion demonstrated a resonant abdomen and auscultation demonstrated normal bowel sounds.
Admission bloods were notable only for an acute kidney injury with a slightly elevated urea but normal inflammatory markers. Plain film of the abdomen was also unremarkable.
A diagnosis of femoral hernia was made and the patient was fasted for theater with intravenous fluids administered to correct the acute kidney injury pre-operatively.
A low Lockwood approach was favored and a right groin incision was made. An irreducible right femoral hernia was confirmed intra-operatively; however, when the sac was opened, a non-inflamed appendix was found within the sac. To facilitate reduction of the hernia, an appendicectomy was performed. A McVay hernioplasty using a 1 Ethibond suture was performed. Local anesthetic was administered and the skin was closed with interrupted absorbable sutures.
Post-operatively, the patient had no surgical complications; however, she developed a chest infection and she was discharged home on day 6.
Histopathology confirmed a non-inflamed appendix with an incidental finding of a “sessile serrated lesion without conventional dysplasia”; however, all margins were clear.
| Discussion | ▴Top |
Rene Jacques Croissant de Garengeot first described the presence of the vermiform appendix in a femoral hernia sac in 1731 [1].
De Garengeot’s hernia is a rare entity, and is seen more frequently in females than in males, by a ratio of 3:1.
The incidence of this disease is estimated to be 0.9% during femoral hernia repairs [4] and the mean age of patients with this condition is 55 years [5].
Many theories have been suggested for the pathogenesis of de Garengeot’s hernia. The most widely accepted is the congenital theory, where pelvic localization of the appendix and a rigid femoral ring predispose to its development [6]. The evolution of inflammation in the appendix is thought to be secondary to the engagement of the appendix in the hernia sac.
Although there are occasional cases diagnosed pre-operatively, typically the appendix is found incidentally during repair without any pre-operative signs or symptoms as in the case presented [7].
The clinical picture of this condition is one of incarcerated femoral hernia and includes vague abdominal pain and tenderness and an erythematous groin lump. The signs of appendicitis are overshadowed by a tight femoral hernia neck and pelvic rigidity; this anatomical feature prevents the spread of inflammation to the peritoneal cavity [8].
Plain film of the abdomen does not aid in the diagnosis of de Garengeot’s hernia. The condition is usually diagnosed intra-operatively as in this study; however, computed tomography (CT) and ultrasound have been successfully used for pre-operative evaluation. CT has been reported to have 98% specificity and sensitivity for confirming or excluding appendicitis in Garengeot’s hernia [9].
The treatment of choice for de Garengeot’s hernia is emergency surgery, with simultaneous appendicectomy through the hernia incision and primary hernia repair [1]. A low Lockwood approach, as performed in this case provides adequate exposure for both the femoral canal exploration and intra-abdominal access; however, alternative approaches, such as Cooper’s ligament repair and a pre-peritoneal approach have been described in the literature [10].
Once the appendicectomy has been performed, the surgeon must decide how best to fix the femoral hernia. A prosthetic mesh should be avoided in a contaminated field due to the obvious risk of infection but a few reports have described mesh repair even in the presence of an inflamed appendix with no post-operative infection [11].
The risk versus benefit of mesh repair must be considered especially in cases with large hernia defects to reduce the risk of hernia recurrence; however, if the appendix has perforated, the use of mesh for repair of the hernia defect is contraindicated.
Recent studies have supported prosthetic mesh repair, as there is less recurrence of the hernia and no increased rate of wound infection but only in the absence of appendiceal perforation or abscess formation. In the presence of perforation or abscess, the femoral hernia is repaired with non-absorbable sutures and the increased risk of hernia recurrence is accepted [6].
The most common complication of de Garengeot’s hernia repair is wound infection with a rate reaching 29%. Some cases of necrotizing fasciitis and even death have been reported but these are most likely related to the delay in diagnosis and the older age and other co-morbidities of these patients [6].
Conclusion
Although the incidence of de Garengeot’s hernia is extremely low, its possibility must be considered in cases of femoral hernia and systemic signs of inflammation given the lack of abdominal signs of appendicitis as this is a serious and potentially lethal complication and always requires emergency surgery.
CT can be useful in the diagnosis of de Garengeot’s hernia in the absence of clinical signs of appendicitis but this should not cause any delay in the surgical management of this condition.
Early clinical diagnosis and surgical intervention are the best way to reduce the potential complications of this condition. Appendicectomy with mesh-free hernia repair is an acceptable treatment for de Garengeot’s hernia but in cases of large hernia defects or in older patients, mesh repair of the hernia can be considered but only in the absence of perforation.
Grant
None.
Conflicts of Interest
We have no conflict of interest to declare.
| References | ▴Top |
- Akopian G, Alexander M. De Garengeot hernia: appendicitis within a femoral hernia. Am Surg. 2005;71(6):526-527.
pubmed - Tanner N. Strangulated Femoral Hernia Appendix with Perforated Sigmoid Diverticulitis. Proc R Soc Med. 1963;56:1105-1106.
pubmed - Rajan SS, Girn HR, Ainslie WG. Inflamed appendix in a femoral hernial sac: de Garengeot's hernia. Hernia. 2009;13(5):551-553.
doi pubmed - Gurer A, Ozdogan M, Ozlem N, Yildirim A, Kulacoglu H, Aydin R. Uncommon content in groin hernia sac. Hernia. 2006;10(2):152-155.
doi pubmed - Sharma H, Jha PK, Shekhawat NS, Memon B, Memon MA. De Garengeot hernia: an analysis of our experience. Hernia. 2007;11(3):235-238.
doi pubmed - Nguyen ET, Komenaka IK. Strangulated femoral hernia containing a perforated appendix. Can J Surg. 2004;47(1):68-69.
pubmed - Zissin R, Brautbar O, Shapiro-Feinberg M. CT diagnosis of acute appendicitis in a femoral hernia. Br J Radiol. 2000;73(873):1013-1014.
doi pubmed - Fukukura Y, Chang SD. Acute appendicitis within a femoral hernia: multidetector CT findings. Abdom Imaging. 2005;30(5):620-622.
doi pubmed - Rao PM, Rhea JT, Novelline RA, Mostafavi AA, McCabe CJ. Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med. 1998;338(3):141-146.
doi pubmed - Cordera F, Sarr MG. Incarcerated appendix in a femoral hernia sac. Contemp Surg. 2003;59:35-37.
- Barbaros U, Asoglu O, Seven R, Kalayci M. Appendicitis in incarcerated femoral hernia. Hernia. 2004;8(3):281-282.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


