| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 7, Number 9, September 2016, pages 403-405
Cytomegalovirus Hepatitis in HIV Infection
Abeer Albaadania, Salwa Alhumaidib, Shuaa Asiric
aDivision of Infectious Disease, Department of Medicine, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
bDepartment of Medicine, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
cHistopathology Department, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
dCorresponding Author: Abeer Albaadani, Division of Infectious Disease, Department of Medicine, Riyadh Prince Sultan Military Medical City, Riyadh, Saudi Arabia
Manuscript accepted for publication August 10, 2016
Short title: CMV Hepatitis in HIV
doi: http://dx.doi.org/10.14740/jmc2618w
| Abstract | ▴Top |
Human immunodeficiency virus (HIV) is a virus spread through certain body fluids that attacks the body’s immune system, specifically the CD4 cells, often called T cells. This damage to the immune system makes it harder and harder for the body to fight off infections. acquired immunodeficiency virus (AIDS) is the stage of infection that occurs when the immune system is badly damaged and becomes more vulnerable to opportunistic infections. Cytomegalovirus (CMV) infection is one of the major causes of morbidity and mortality in patients with AIDS, mainly at very low CD4 count of < 50 cells/mm3 with particular involvement of the retina causing chorioretinitis. Nevertheless, the involvement of other organs is unusual in AIDS patients. Here we present a case of HIV with CMV-related hepatitis which is considered a very rare presentation.
Keywords: CMV hepatitis; AIDS; HIV
| Introduction | ▴Top |
Cytomegalovirus (CMV) is a known opportunistic pathogen among immune-compromised patients with various spectra of manifestations which most of the time depend on the underlying immune suppression status. In solid organ or hematopoietic stem cell transplant, CMV has a predilection to invade the allograft leading to graft rejection or invasive disease such as pneumonitis, colitis or bone marrow suppression [1]. On the other hand, CMV is a manifestation of advanced retroviral disease with predominant involvement of the retina causing retinitis. We describe a case of CMV hepatitis as immune reconstitution inflammatory syndrome (IRIS) in a retroviral human immunodeficiency virus (HIV) patient.
| Case Report | ▴Top |
A 43-year-old gentleman known to have HIV, hypothyroidism, type 1 DM and vitiligo presented with poor oral intake and generalized fatigability 2 weeks before presentation. He had no history of fever, night sweats, chills, cough, chest pain, shortness of breath, vomiting, abdominal or genitourinary symptoms.
He was diagnosed recently with HIV when he was admitted to another hospital as a case of chest infection and discovered to have acquired immunodeficiency virus (AIDS) with very low CD4 counts of 4. He was started on truvada and efavirenz with pneumocystis (PCP) prophylaxis. Later on, after discharge, patient became more depressed, and neglected himself living alone till he was brought by one relative to us.
Examination
He was conscious, alert, and oriented but looked dehydrated, pale and jaundice, and cachectic with hypopigmented patches over his face, hand, and trunk. There was no lymphadenopathy but with extensive oral thrush. Vital signs showed temperature 37.6 °C, BP 99/65 mm Hg, HR 80 bpm, and RR 20 bpm. Chest was clear. Cardiovascular system was unremarkable. Abdomen was soft, lax with mild hepatosplenomegaly but no stigmata of liver disease. Funduscopic examination showed no evidence of retinitis.
Laboratory results
WBC was 2.9 × 109/L (4.0 - 11.0), Hb was 9 g/dL (12.5 - 18.0), and platelet was 232 × 109/L (150 - 450). Baseline liver profile showed total bilirubin 72 (2 - 21), ALT 54 (0 - 42), alkaline phosphatise 619 (40 - 129) U/L, GGT 952 (8 - 61), LDH 247 (135 - 225) U/L, albumin 26 (35 - 52) g/L, direct bilirubin 95 μmol/L (0 - 5), NA 128 mmol/L (136 - 145), K 4.5 mmol/L (3.5 - 5.1), urea 3.7 mmol/L (2.8 - 8.1), creatinine 45 μmol/L (59 - 104), CRP 35, CMV IgG positive/IgM negative, CD4 41 cells/mm3 (29 - 59), and HIV PCR quantitative 9,974 copies. Toxoplasma IgG was negative, syphilis screening was negative, and hepatitis A, B, C was negative. No infiltration was seen in chest X-ray. CT CAP (chest, abdomen and pelvis) showed generalized meditational, subcarinal lymphadenopathy, right upper lobe ground glass opacity with mild hepatosplenomegaly. Based on these findings, the patient was worked up to rule out opportunistic infection (TB-Mycobactrium avium complex) or lymphoma. ART had been continued with switching of efavirenz to raltegravir along with prophylactic daily dose septrin. At the same time, given his liver derangement, he was put empirically in modified anti-tuberculosis (anti-TB) drugs covering both possibilities of MTB and NTB mainly ethambutol, moxifloxacin, amikacin and clarithromycin. Shortly after the patient underwent US-guided liver biopsy, he was sent for AFB stain, TB and fungal culture, TB PCR and histopathology. During the hospital stay, the patient experienced episode of shortness of breath which then improved on antibiotics coverage (piperacillin-tazobactam) and anti-TB.
Later on, the histopathology result of liver biopsy had shown multiple non-necrotizing granuloma with intranuclear inclusion bodies characteristics of CMV hepatitis (Figs. 1 and 2). Furthermore, CMV PCR viral load was 14,714. Based on that, he was put on intravenous ganciclovir 5 mg/kg q12h for 3 weeks with follow-up CMV viremia of 2,874, then he was switched to oral valganciclovir 900 mg q12h until his viremia was undetectable, and then he was switched to secondary prophylaxis 900 mg oral q24h which had to be till the improvement of CD4 to be more than 100 cells/mm3 for consecutive 6 months. The patient was discharged in good condition and improved liver functions on valganciclovir and septrin along with ART. However, anti-TB had been discontinued awaiting the further microbiological results. Interestingly, his liver biopsy culture after 1 month showed non-tuberculous mycobacteria for which he was started on rifampicin, ethambutol and clarithromycin.
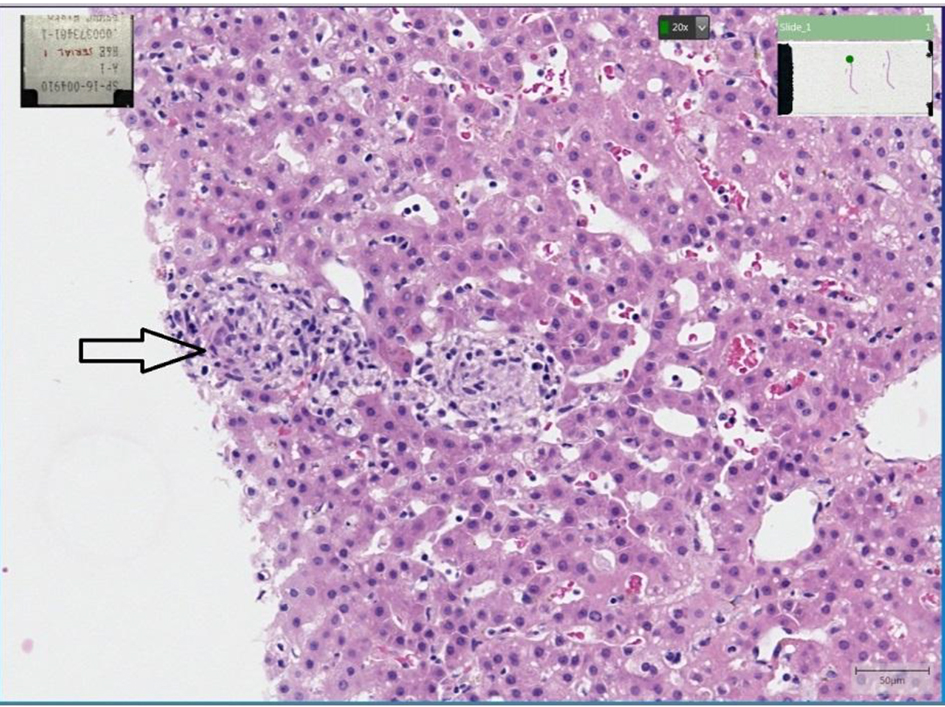 Click for large image | Figure 1. Liver tissue showing multiple granulomas (arrow), composed of aggregates of histocytes, lymphocytes and plasma cells. |
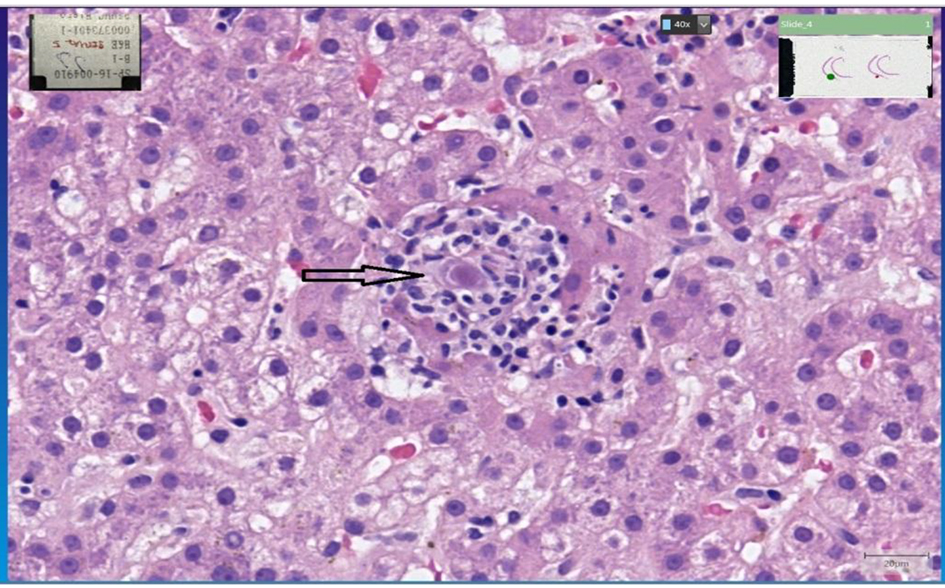 Click for large image | Figure 2. Deeper levels show cells of characteristic intranuclear and intracytoplasmic inclusions (CMV). |
| Discussion | ▴Top |
CMV is one of the herpes viruses that can stay dormant in the human body after the primary infection, and then will reactivate when the immune system is suppressed secondary to any reason including retroviral infection. Usually, it manifests at a very low level of CD4 < 50 cells/mm3 with predominant retinal involvement. After introducing ART, the rate had declined to be approximately 0.75 - 3.2 cases per 100 person-years [2]. However, some case reports had described other organ damages such as pneumonia, hepatitis, myocarditis and meningitis in the setting of primary HIV and CMV coinfection [3, 4]. CMV hepatitis is a frequent feature in liver transplant recipients. However, it is uncommon in HIV-infected patients [5]. Our patient is seropositive for CMV which considered him previously infected and, thus, his presentation represents either reactivation of latent infection or reinfection with a novel strain.
Interestingly, our patient was diagnosed to have retroviral disease and started on ART about 1 month prior to the occurrence of CMV diseases which had made the IRIS strongly possible. It is worthy to mention that similar reaction had been reported in a primary HIV patient who had been started on ART then complicated with unusual CMV colitis with colonic perforation [6].
The presence of CMV viremia is known to have little positive predictive value in patients with HIV and does not mandate presence of invasive disease, even at low CD4 T-lymphocyte counts [7]. In our patient CMV hepatitis was detected by hepatic histopathological examination. As reported from the previous studies, the detection of CMV infection by PCR is correlated with the development of CMV disease and death in the future [8]. Ganciclovir had been started at baseline CMV viral load of 14,714, and then was continued till his plasma CMV level had decreased to the reference level.
Our case highlights the importance of CMV as a potential pathogen causing extraretinal disease in a patient with HIV infection.
Abbreviations
CMV: cytomegalovirus; HIV: human immunodeficiency virus; AIDS: acquired immunodeficiency virus; anti-TB: anti-tuberculosis
| References | ▴Top |
- Razonable RR, Humar A. Cytomegalovirus in solid organ transplantation. Am J Transplant. 2013;13(Suppl 4):93-106.
doi pubmed - Salzberger B, Hartmann P, Hanses F, Uyanik B, Cornely OA, Wohrmann A, Fatkenheuer G. Incidence and prognosis of CMV disease in HIV-infected patients before and after introduction of combination antiretroviral therapy. Infection. 2005;33(5-6):345-349.
doi pubmed - Hong KW, Kim SI, Kim YJ, Wie SH, Kim YR, Yoo JH, Han NI, et al. Acute cytomegalovirus pneumonia and hepatitis presenting during acute HIV retroviral syndrome. Infection. 2011;39(2):155-159.
doi pubmed - Kim JY, Singer EJ, Bonelli L, Klausner JD. A case of primary HIV type 1 and cytomegalovirus coinfection presenting with widespread clinical disease. J Int Assoc Provid AIDS Care. 2014;13(3):196-199.
doi pubmed - Razonable RR. Cytomegalovirus infection after liver transplantation: current concepts and challenges. World J Gastroenterol. 2008;14(31):4849-4860.
doi pubmed - von Both U, Laffer R, Grube C, Bossart W, Gaspert A, Gunthard HF. Acute cytomegalovirus colitis presenting during primary HIV infection: an unusual case of an immune reconstitution inflammatory syndrome. Clin Infect Dis. 2008;46(4):e38-40.
doi pubmed - Masur H. Management of opportunistic infections associated with human immunodeficiency virus infection. In: Mandell GL, BennettJE, Dolin R, editors. Principles and practice of infectious diseases. 7th ed. Philadelphia: Churchill Livingstone; 2009. p. 1875-1877.
- Deayton JR, Prof Sabin CA, Johnson MA, Emery VC, Wilson P, Griffiths PD. Importance of cytomegalovirus viraemia in risk of disease progression and death in HIV-infected patients receiving highly active antiretroviral therapy. Lancet. 2004;363(9427):2116-2121.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


