| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 8, Number 2, February 2017, pages 36-38
Incidental Spontaneous Coronary Artery Dissection
Jeffrey Ziffraa, c, Nathanael Trollb, Brock Cookmana
aDepartment of Cardiology, Mercy Medical Center, Mason City, IA, USA
bDes Moines University School of Osteopathic Medicine, Des Moines, IA, USA
cCorresponding Author: Jeffrey Ziffra, Mercy Medical Center, North Iowa, 1000 4th St. SW, Mason City, IA 50401, USA
Manuscript accepted for publication December 15, 2016
Short title: Spontaneous Coronary Artery Dissection
doi: https://doi.org/10.14740/jmc2722w
| Abstract | ▴Top |
Spontaneous coronary artery dissection (SCAD) is a rare diagnosis that presents both a diagnostic and therapeutic challenge. This disorder is rare but more often found in young and pregnant females. The diagnosis of SCAD is difficult as the presenting signs and symptoms may be non-specific. The treatment for SCAD may often be conservative if the patient does not have acute coronary syndrome. Patients who experience dissection are at risk for future events. We present a case of a 44-year-old male with a history of smoking and hypertension who presented with chest pain and syncope. He was found on angiogram to have an SCAD.
Keywords: Coronary artery dissection; Acute coronary syndrome; Coronary angiography
| Introduction | ▴Top |
We describe a case of a 44-year-old male with coronary artery disease risk factors who presented with chest pain and syncope. On angiogram, the patient was found to have a spontaneous coronary artery dissection (SCAD). This is a rather rare presentation in this patient subset that presents a diagnostic and therapeutic challenge. Spontaneous dissections are more often seen in young women and pregnant women as well. Clinicians must be aware of similar cases of SCAD and therapeutic options for these patients.
| Case Report | ▴Top |
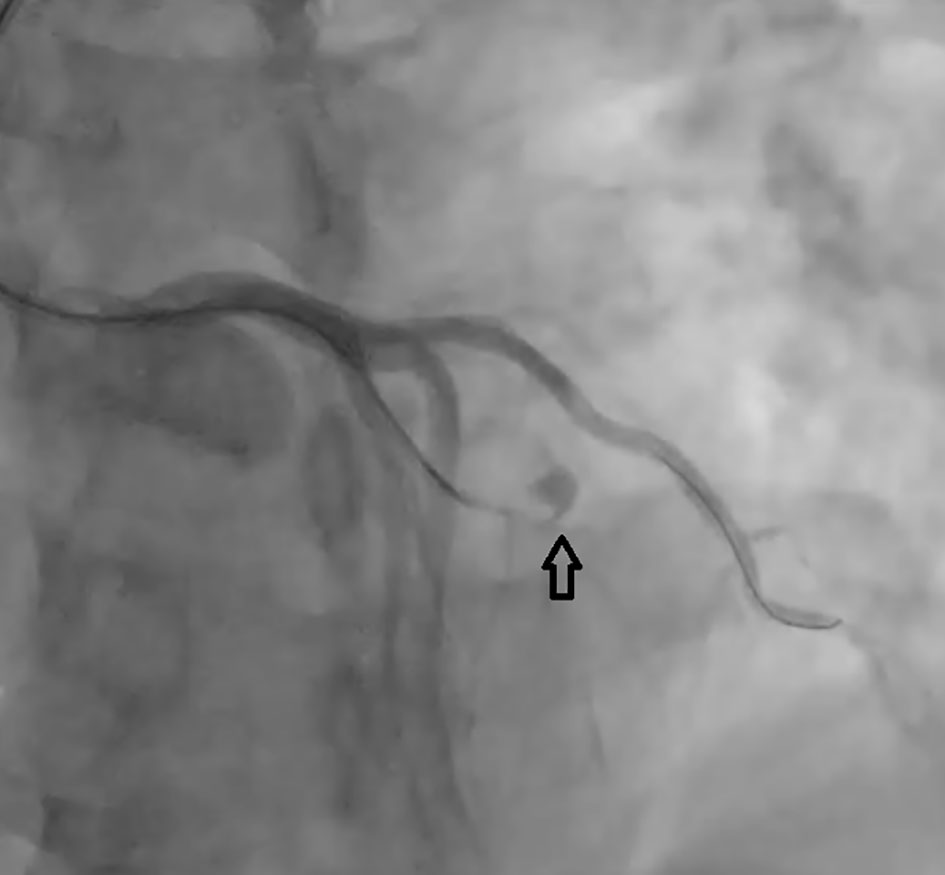
The patient is a 44-year-old male with a history of smoking and hypertension who presented to the office complaining of chest pain and episodes of recurrent syncope. Because of his presenting symptoms, he was taken for cardiac catheterization. During his angiogram, he was found to have a chronic dissection of the mid left anterior descending (LAD) artery which filled via left-to-left septal collaterals (Fig. 1). He was also found to have non-occlusive disease to his first obtuse marginal branch. He was treated conservatively with medical management. Upon follow-up, he continued to have typical angina with activity and rest. His exercise capacity was greatly limited due to ongoing chest pain.
 Click for large image | Figure 1. First angiogram revealing chronic mid LAD dissection filled by collaterals. |
Upon examination, the patient’s vitals were a temperature of 97.9 °F, blood pressure of 123/86 mm Hg, heart rate of 56 beats per minute, respiratory rate of 16 per minute and saturating 96% on room air. He was not in acute distress, and his heart was a regular rate and rhythm without murmurs. His lungs were clear to auscultation bilaterally. He was perfusing all four extremities and they were free of lower extremity edema. Because of the progressive and limiting nature of his angina, the patient was scheduled for a repeat angiogram. During this procedure, the chronic LAD occlusion was not able to be intervened due to a perforation of the LAD (Fig. 2). A 2D echocardiogram was performed later which did not reveal a pericardial effusion. His ejection fraction was found to be normal at 60%.
 Click for large image | Figure 2. Second angiogram revealing contained LAD perforation, at site of total occlusion. |
| Discussion | ▴Top |
SCAD is a rare diagnosis that presents both a diagnostic and therapeutic challenge. The incidence has been widely reported as anywhere from 0.28% and 1.1% [1]. The amount of new cases has increased likely due to availability of coronary angiography and more awareness of the diagnosis. Also contributing to an increase in incidence is the newly described angiographic variants of SCAD. A new estimate of SCAD in patients presenting with ACS is 1.7-4% [2]. Women have been reported in over 90% of cases with many cases also reported on pregnant females. Males who have been reported tend to be younger as well [2-4].
Arterial dissection in SCAD can occur within or between any of the three layers of the arterial wall. Two possible mechanisms for the initiation of arterial dissection have been proposed. The first is the intimal tear hypothesis in which a disruption in the intimal-luminal junction creates a nidus for intramural hematoma and separation of the arterial wall. The second mechanism is the medial hemorrhage hypothesis in which a hemorrhage occurs within the arterial wall due to spontaneous rupture of the vasa vasorum. This can cause a rupture into the true lumen in an almost reverse intimal rupture. In both cases, the principle abnormality is a plane of dissection which causes compression of the true lumen and threatens distal blood flow [1, 2].
Diagnosis of SCAD is difficult as there may be many presenting signs and symptoms that are similar to acute coronary syndrome. Electrocardiograms can be non-specific but may also show ST-segment changes, ventricular tachycardia, or ventricular fibrillation arrest [3]. Echocardiogram and biomarkers may be useful but can also be non-specific as well. Generally, cardiac angiogram is the diagnostic modality of choice. There may be a clear appearance of dissection with a false lumen [1]. Data show a higher incidence of spontaneous dissections, many found post-mortem, than are reported on angiography. The use of intravascular ultrasound may be added to find dissections not easily found on angiography. Ultrasound increases the sensitivity of detection of medial dissection, hematoma, or small plaques [5]. The ability of these tools has increased the diagnosis of SCAD as much of the presentation may be non-specific in patients who may not have coronary risk factors [2].
Treatment for SCAD can be either conservative or invasive in nature and is often based on presentation. Medical therapy may be appropriate in clinically stable patients with a limited dissection and small area of myocardium at risk. In a prospective study of 168 patients by Almeda et al, patients treated conservatively did develop spontaneous healing of their dissection [3]. Conservative therapy has been proven in several trials to have an excellent long-term prognosis [6]. Several cases have reported need for revascularization including a patient with cocaine abuse who had a left main artery dissection extending distally to the LAD and circumflex artery requiring four vessel coronary artery bypass grafting [7]. Percutaneous coronary intervention (PCI) has often been preferred to bypass grafting; however, thrombolytics have not been suggested for theoretical concerns [1, 8]. PCI does have a higher rate of complication than conservative therapy and may not prevent recurrent SCAD from occurring [9].
In conclusion, our patient was having episodic angina but was hemodynamically stable without EKG changes. He was treated conservatively initially; however, he returned to the clinic with worsening symptoms. Upon reevaluation, he was found to be worsening and a repeat angiogram was performed without intervention. Conservative management, with medical treatment, was correctly given upon initial discovery of the patient’s chronic spontaneous coronary artery dissection. When the patient’s symptoms worsened, it is reasonable to believe the patient failed medical therapy. Clinicians need to be aware of SCAD because it can occur in patients with minimal or no cardiac risk factors. More research needs to be performed on methods to treat patients who fail medical therapy.
Conflicts of Interest
None of the authors have financial disclosures or conflicts of interest.
Grant
None.
| References | ▴Top |
- Bezgin T, Elveran A, Dogan C, Karagoz A, Kulahcioglu S, Canga Y, Esen AM. Chronic spontaneous right coronary artery dissection. Herz. 2014;39(3):397-399.
doi pubmed - Saw J, Mancini GB, Humphries KH. Contemporary Review on Spontaneous Coronary Artery Dissection. J Am Coll Cardiol. 2016;68(3):297-312.
doi pubmed - Almeda FQ, Barkatullah S, Kavinsky CJ. Spontaneous coronary artery dissection. Clin Cardiol. 2004;27(7):377-380.
doi pubmed - Eleid MF, Guddeti RR, Tweet MS, Lerman A, Singh M, Best PJ, Vrtiska TJ, et al. Coronary artery tortuosity in spontaneous coronary artery dissection: angiographic characteristics and clinical implications. Circ Cardiovasc Interv. 2014;7(5):656-662.
doi pubmed - Maehara A, Mintz GS, Castagna MT, Pichard AD, Satler LF, Waksman R, Suddath WO, et al. Intravascular ultrasound assessment of spontaneous coronary artery dissection. Am J Cardiol. 2002;89(4):466-468.
doi - Alfonso F, Paulo M, Lennie V, Dutary J, Bernardo E, Jimenez-Quevedo P, Gonzalo N, et al. Spontaneous coronary artery dissection: long-term follow-up of a large series of patients prospectively managed with a "conservative" therapeutic strategy. JACC Cardiovasc Interv. 2012;5(10):1062-1070.
doi pubmed - Eskander KE, Brass NS, Gelfand ET. Cocaine abuse and coronary artery dissection. Ann Thorac Surg. 2001;71(1):340-341.
doi - Zupan I, Noc M, Trinkaus D, Popovic M. Double vessel extension of spontaneous left main coronary artery dissection in young women treated with thrombolytics. Catheter Cardiovasc Interv. 2001;52(2):226-230.
doi - Tweet MS, Eleid MF, Best PJ, Lennon RJ, Lerman A, Rihal CS, Holmes DR, Jr., et al. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv. 2014;7(6):777-786.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


