| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 8, Number 3, March 2017, pages 98-101
Advantages of Post-Mastectomy Proton Beam Therapy in a Breast Cancer Patient With Pectus Excavatum
Bryeson Rodgersa, Dawn E. Jaroszewskia, c, Jonathan B. Ashmanb, William G. Ruleb, Terence T. Siob, Sameer R. Keoleb
aDepartment of Cardiothoracic Surgery, Mayo Clinic Arizona, 5777 E Mayo Blvd, Phoenix, AZ 85054, USA
bDepartment of Radiation Oncology, Mayo Clinic Arizona, 5777 E Mayo Blvd, Phoenix, AZ 85054, USA
cCorresponding Author: Dawn E. Jaroszewski, Department of Cardiothoracic Surgery, Mayo Clinic Arizona, 5777 E Mayo Blvd, Phoenix, AZ 85054, USA
Manuscript accepted for publication February 23, 2017
Short title: Post-Mastectomy PBT in Pectus Excavatum
doi: https://doi.org/10.14740/jmc2781w
| Abstract | ▴Top |
Pectus excavatum (PE) is a chest wall deformity that can complicate the delivery of radiation therapy (RT) for breast cancer. This case report highlights the potential benefits of proton beam therapy (PBT) for these patients. We describe a case of a 79-year-old woman with PE who required post-mastectomy chest wall RT. Treatment plans were generated to deliver 45 Gy in 25 fractions with either PBT or conventional conformal photon RT. A 10-Gy boost to the post-mastectomy scar was used for both plans. A dosimetric benefit was observed for organs at risk with the PBT plan compared to the photon plan. PBT reduced mean doses to the lungs by more than 70% and to the heart by greater than 95%. The patient was treated with PBT with minimal acute toxicities. With the challenging chest anatomy of PE, PBT was selected as the treatment of choice for post-mastectomy radiation. The superior dosimetry can decrease the risks of post-treatment cardiac and pulmonary toxicities.
Keywords: Proton therapy; Breast cancer; Pectus excavatum; Funnel chest wall deformity; Particle beam therapy
| Introduction | ▴Top |
Pectus excavatum (PE) is the most common chest wall deformity with an incidence of 1 in 300 - 1,000 live births and a male to female ratio of 5:1 [1]. The defect is characterized by an inward sunken sternum and costal cartilages, which may compress the right heart and anterior mediastinal structures. Pectus patients with breast cancer undergoing traditional radiation therapy (RT) to the chest wall may have considerable risk of increased toxicity due to the proximity of the underlying cardiac structures [2, 3]. RT target volumes in breast cancer tumor sites are located immediately anterior to the organs and structures of the thorax, and decreasing radiation toxicity to these organs at risk is a foremost priority. The rate of major coronary events is reported to increase linearly by 7.4% with every Gray of mean heart dose [4]. The risk of clinically significant symptomatic radiation pneumonitis is 5-10% and 1-5% following irradiation of cancers of the mediastinal lymphatics and breast, respectively [5].
The use of proton beam therapy (PBT) for treatment of breast cancer has been increasing over the past decade due to dosimetric advantages over conformal photon RT [6, 7]. For many post-mastectomy RT patients, photon RT techniques result in increased radiation of normal structures in the chest compared with PBT plans [3, 7, 8]. PBT may offer greater benefits for breast cancer patients with PE as the abnormality of the chest wall can cause the tumor sites to move more anterior to the heart, lungs, left anterior descending coronary artery, as well as other important structures. This case report presents the novel use of PBT in a patient with breast cancer and the PE chest wall deformity.
| Case Report | ▴Top |
Patient and methods
A 79-year-old female patient initially presented with a 2-cm poorly differentiated, high-grade adenocarcinoma (ER+, PR-, HER-2/neu-) of the left breast with clinically positive axillary nodal metastasis diagnosed 11 months prior. Breast cancer risk factors included 14 years of prior estrogen replacement therapy. The patient had no significant documented past medical, surgical, gynecologic, or family history. Notably, she had never been officially diagnosed with PE, although this deformity had been present since her childhood (Fig. 1).
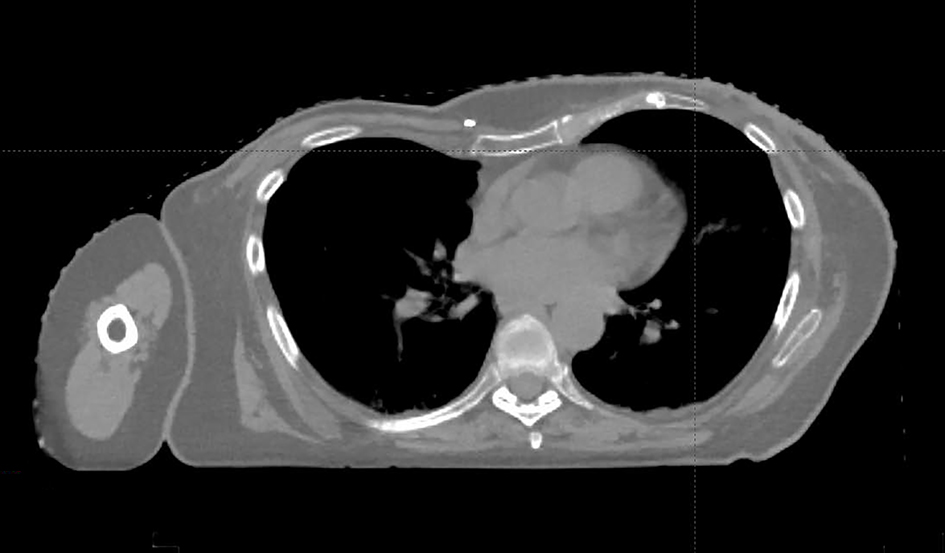 Click for large image | Figure 1. This patient’s chest deformity consistent with PE. Medial axial thoracic CT scan demonstrates the compression of heart and anterior mediastinal structures due to inward sunken sternum and costal-cartilages. |
Initial management included four cycles of neoadjuvant chemotherapy consisting of dose-dense doxorubicin and cyclophosphamide. After the third cycle, echocardiography demonstrated a decrease in ejection fraction to 45% with mild diastolic dysfunction. This decline in cardiac function was attributed to doxorubicin, and the fourth cycle was withheld. She subsequently completed 12 cycles of docetaxel. Following chemotherapy, bilateral mastectomies were performed due to personal choice and pathology demonstrated complete pathologic response within the left breast (ypT0). Metastatic high-grade infiltrating ductal carcinoma persisted in two axillary lymph nodes, including one with extra-capsular extension.
With persistent positive lymph nodes despite neoadjuvant chemotherapy, she was considered high risk for local recurrence. Comprehensive RT was recommended with fields to include the left chest wall combined with axillary, supraclavicular and internal mammary nodal regions. The prescription dose was 45 Gy to the chest wall in 25 fractions administered over 5 weeks followed by an additional 10 Gy boost in 5 fractions to the chest wall scar using electron radiation. After CT simulation for radiotherapeutic treatment planning, cardiothoracic surgeon DEJ was consulted and confirmed the presence of PE with compression of the right heart and a shift into the left thorax (Fig. 1). Given the anatomic challenges and the previously documented cardiac abnormalities, PBT was considered as an alternative to conventional photon RT. Appropriate patient consent and planning were obtained by the treating radiation oncologist (SRK). The patient was enrolled in an IRB approved registry study.
Results
Treatment planning
For this patient, comparison treatment plans were constructed with standard photon tangents versus PBT. Figure 2 displays the potential dosage plans and the difference in dose distribution. Overall coverage of the target volume was satisfactory for both the photon RT and PBT plans (legend of Fig. 3). Achieving similar coverage was critical to being able to compare the different radiation treatment plans. The images in Figure 2 display the gradient of dosages between the photon RT plan (left) and the PBT plan (right). The dose volume histogram in Figure 3 shows the decreased irradiation to the lungs and heart. Mean dose of the total lungs was reduced from 8.43 Gy with the photon RT plan to 2.21 Gy with the PBT plan, representing a 73.8% decrease in mean radiation given to the lungs. The V20Gy for the total lungs was reduced from about 15% to less than 5%. The mean dose to the ipsilateral lung was reduced from 16.49 Gy with the photon RT plan to 4.39 Gy with the PBT plan, representing a 73.4% decrease in mean radiation given to the ipsilateral lung. The V20Gy for the ipsilateral lung was reduced from about 30% to less than 5%. The mean dose to the heart was reduced from 6.53 Gy with the photon RT plan to 0.25 Gy with the PBT plan, representing a 96.2% decrease in mean radiation administered to the heart.
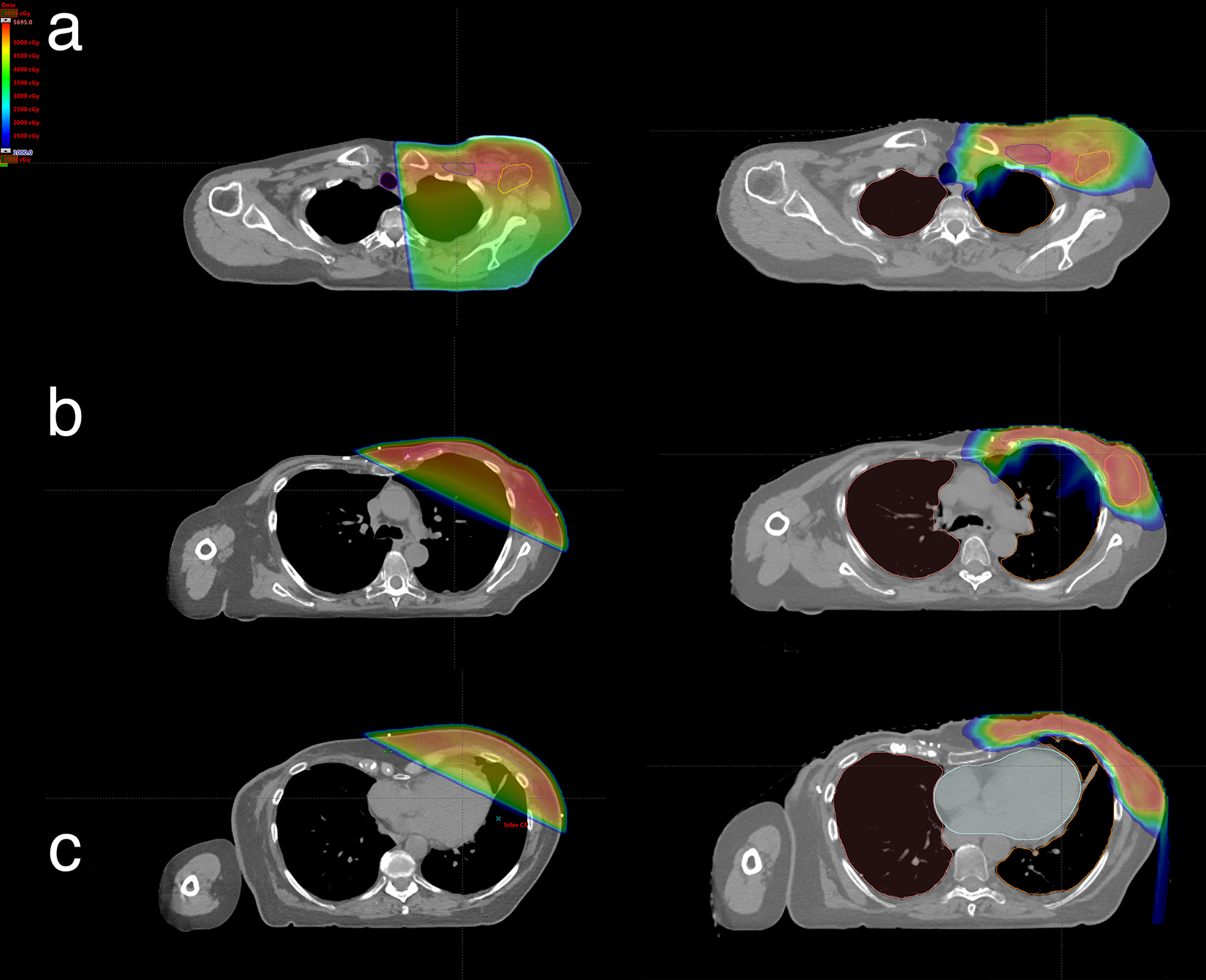 Click for large image | Figure 2. Radiation dose distribution comparisons of the superior (a), medial (b), and lower (c) axial thoracic CT levels: conformal photon RT plan (left) and PBT plan (right). |
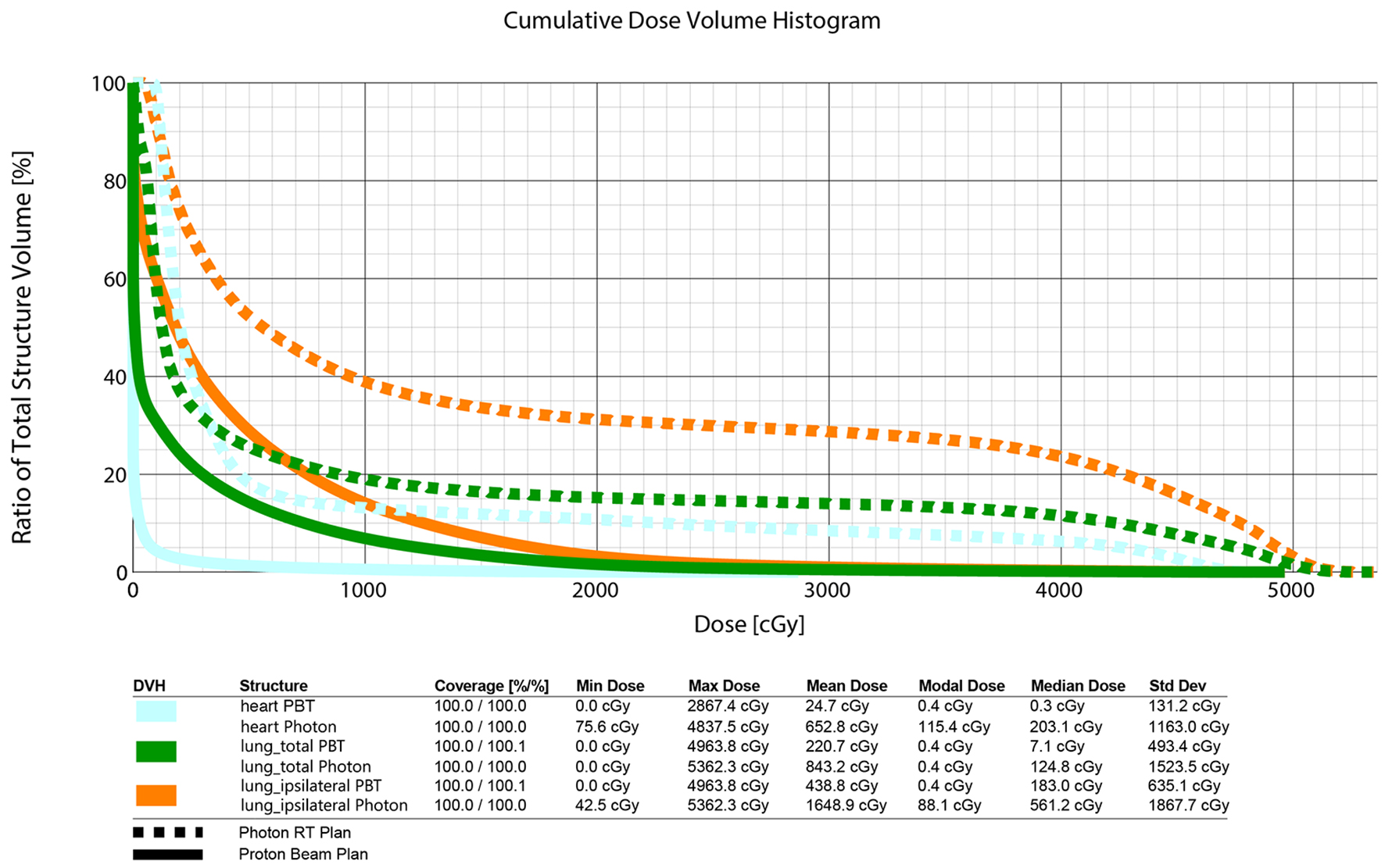 Click for large image | Figure 3. Dose volume histogram comparing photon RT plan and PBT plan. Cyan depicts heart volume; green depicts total lungs volume; orange depicts ipsilateral lung volume. |
Treatment delivery
Treatment with our institution’s scanning PBT was selected in an effort to minimize radiation dose to the already functionally depressed myocardium. The patient received comprehensive radiation via a PBT plan. She received 45 Gy in 25 fractions over 5 weeks to the chest wall and nodal regions noted above with the additional 10 Gy boost in 4 fractions to the chest wall scar utilizing enface electrons. Treatment was well tolerated with only grade 1 dermatitis noted at treatment completion. On 4-month follow-up, she was doing well without any residual dermatitis or evidence of radiation-induced complications. An echocardiogram done at 4 months status post PBT shows an ejection fraction of 62% which was improved since pretreatment.
| Discussion | ▴Top |
Exposure of normal tissue, especially the heart and lungs, to ionizing radiation during conventional photon RT for breast cancer can result in significant long-term morbidity [4]. PBT can potentially deliver superior homogenous target coverage with a decreased dose to lung, heart, and other mediastinal structures [6]. In this case, the radiation exposure to the organs at risk was even higher due to the deformity caused by PE, which brought the heart and ipsilateral lung into even closer apposition. Reduction in cardiac dose is particularly important in high-risk patients such as this patient having coexistent chemotherapy-induced cardiomyopathy. Other methods of treatment have been proposed to solve this difficult clinical problem including volume-modulated arc therapy, intensity-modulated radiation, and deep inspiration breath-hold technique resulting in cardiac radiation reduction by anywhere from 30% to 70% [9]. But PE creates another complex scenario with the inward deformity of the chest wall causing compression of the heart, which increases not only the exposure of the heart to chest wall radiation but also exacerbates the underlying decreased cardiac output [10]. These two factors suggest that our patient would be at greater risk to the side effects of chest wall RT and would have greater clinical benefit from the demonstrated dosimetric advantages of PBT.
Conclusion
This case describes a substantial dosimetric benefit to treating the chest wall in a patient with PE deformity utilizing PBT versus conformal photon RT. PBT allowed for comparably satisfactory coverage of the target area (chest wall and regional lymph nodes) along with decreased dose to the heart (mean heart dose reduced by greater than 95%) and to the lungs (mean lung dose reduced by greater than 70%). This may significantly lower the patient’s risk of late cardiopulmonary complications and acute radiation pneumonitis.
Acknowledgments
The authors would like to thank the people involved with helping us write this case report, specifically dosimetrist Kathryn O’Leary.
Grant
None.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
| References | ▴Top |
- Sarwar ZU, DeFlorio R, O'Connor SC. Pectus excavatum: current imaging techniques and opportunities for dose reduction. Semin Ultrasound CT MR. 2014;35(4):374-381.
doi pubmed - Cendales R, Vasquez J, Arbelaez JC, Bobadilla I, Espanol R, Torres F, Gaitan A. Intensity modulated radiotherapy (IMRT) with simultaneous integrated boost (SIB) in a patient with left breast cancer and pectus excavatum. Clin Transl Oncol. 2012;14(10):747-754.
doi pubmed - Perni S, Kim SK, Chin C, Pfister NT, Tiwari A, Horowitz DP. Radiation therapy for right-sided breast cancer in a patient with pectus excavatum: A comparison of treatment techniques. Pract Radiat Oncol. 2016;6(6):383-387.
doi pubmed - Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Bronnum D, Correa C, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368(11):987-998.
doi pubmed - Marks LB, Bentzen SM, Deasy JO, Kong FM, Bradley JD, Vogelius IS, El Naqa I, et al. Radiation dose-volume effects in the lung. Int J Radiat Oncol Biol Phys. 2010;76(3 Suppl):S70-76.
doi pubmed - MacDonald SM. Proton Therapy for Breast Cancer: Getting to the Heart of the Matter. Int J Radiat Oncol Biol Phys. 2016;95(1):46-48.
doi pubmed - Verma V, Shah C, Mehta MP. Clinical Outcomes and Toxicity of Proton Radiotherapy for Breast Cancer. Clin Breast Cancer. 2016;16(3):145-154.
doi pubmed - (P004) A Comparison of Postmastectomy Radiation Therapy (PMRT) With Protons vs Photons. Oncology (Williston Park). 2016;30(Suppl).
- Stahl JM, Hong JC, Lester-Coll NH, Kann BH, Wilson LD, Higgins SA, Evans SB. Chest Wall Deformity in the Radiation Oncology Clinic. Anticancer Res. 2016;36(10):5295-5300.
doi pubmed - Chao CJ, Jaroszewski DE, Kumar PN, Ewais MM, Appleton CP, Mookadam F, Gotway MB, et al. Surgical repair of pectus excavatum relieves right heart chamber compression and improves cardiac output in adult patients - an intraoperative transesophageal echocardiographic study. Am J Surg. 2015;210(6):1118-1124; discussion 1124-1115.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


