| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 8, Number 5, May 2017, pages 167-169
Pregnant With Myocardial Infarction, How Should I Manage?
Emin Uysala, c, Suleyman Solaka, Sakir Omur Hincala, Sinan Varolb
aDepartment of Emergency Medicine, Bagcilar Research and Training Hospital, Bagcilar Egitim ve Arastirma Hastanesi Acil Tip Klinigi, Bagcilar, Istanbul 34200, Turkey
bDepartment of Cardiology, Bagcilar Research and Training Hospital, Bagcilar Egitim ve Arastirma Hastanesi Kardiyoloji Klinigi, Bagcilar, Istanbul 34200, Turkey
cCorresponding Author: Emin Uysal, Department of Emergency Medicine, Bagcilar Research and Training Hospital, Bagcilar Egitim ve Arastirma Hastanesi Acil Tip Klinigi, Bagcilar, Istanbul 34200, Turkey
Manuscript accepted for publication April 24, 2017
Short title: Pregnant MI
doi: https://doi.org/10.14740/jmc2827w
| Abstract | ▴Top |
Myocardial infarction (MI) during pregnancy is rare but has important risks for the mother and the fetus. Its prevalence is 1/10,000 - 30,000. A 38-year-old woman at the 37th gestation week was admitted to the emergency department with the complaint of chest pain. She had undergone mitral valve replacement previously. Her electrocardiograph and clinic are in line with ST elevation inferior MI. A thrombus was identified by angiography at posterolateral of circumflex artery. The patient was followed up with medical treatment, and she had normal birth without any complications. The mother and the baby were discharged from hospital to their home after the follow-up period. In conclusion, emergency intervention should be considered for the pregnant women with MI that can be rare but fatal for the mother and the baby.
Keywords: Pregnancy; Myocardial infarction; Emergency
| Introduction | ▴Top |
Myocardial infarction (MI) during pregnancy is rare but important since its mortality is 37-50% [1]. Its prevalence is 1/10,000 - 30,000. Approximately 30% of the cases had normal coronary arteries [2, 3]. This condition is associated with acute coronary thrombosis induced by hypercoagulability [3]. Our aim in this case is that acute myocardial infarction (AMI) management should be considered for the pregnant women who were admitted to emergency department with the complaints of chest pain and diagnosed as ST elevation myocardial infarction (STEMI).
| Case Report | ▴Top |
A 38-year-old woman at the 37th gestation week of her second child was admitted to the emergency department with the complaint of chest pain. Her chest pain has begun about 1 h before the admission. The patient had retrosternal, not widespread pressure style chest pain. She had not a history of a coronary artery disease. She had undergone mitral valve replacement 4 years ago. She had been using 5 mg/day warfarin tablets perorally after the replacement. The history revealed that she discontinued warfarin tablets, and started no low-molecular weight heparin when she became pregnant. No feature was found in her family history. She was conscious and her general condition was good in the emergency department. Arterial blood pressure was 90/60 mm Hg, pulse rate was 83 beats/min, respiratory rate was 18/min and SpO2 was 92%. Heart was rhythmic and a metallic heart sound was heard. An incision scar due to valve replacement was present on the front side of the thorax. Uterus was optimal for the gestation week. The other system examinations were normal. In electrocardiography, there was sinus rhythm, ST segment elevation > 2 mm on DII, DIII and aVF derivations, 0.5 - 1 mm elevation on V5, V6 and reciprocal change of ST segment depression on aVL (Fig. 1). Blood samples were taken. Cardiology consultation was done and 100 mg acetylsalicylic acid was given perorally and 5,000 units heparin was given intravenously in the emergency department. She was referred to coronary angiography unit and coronary artery angiography was performed with the abdominal protection by lead vest. Coronary angiography identified a total distal obstruction in the posterolateral (PL) branch of right circumflex artery (RCA) (Fig. 2). The obstruction was decided to be followed up medically without a stent or percutaneous transluminal coronary angioplasty. During angiography, amniotic pouch ruptured spontaneously and after the cardiac stabilization she was consulted with an obstetrician. Then the patient was taken to the delivery room. Oxytocin infusion was started and 600 mg misoprostol was given rectally. Normal vaginal delivery with cephalic presentation was performed. No retro and preplacental hemorrhage was observed. No complication was observed. The baby was referred to neonatal unit, and the mother was referred to coronary intense care unit. Heparin 100 unit/h infusion was started to the patient at the first day, and 100 mg acetylsalicylic acid once a day, 50 mg metoprolol once a day, 40 mg atorvastatin once a day, 40 mg pantoprazole once a day were administrated. At the second day, heparin infusion was continued, and clopidogrel and warfarin were administrated. At the fifth day, she was referred to cardiology department from the intensive care unit. During the follow-up period, cardiac enzyme levels increased gradually and then decreased. Troponin T value was 0.023 ng/mL (0 - 0.014) in the blood sample at admission, and the peak value was 0.149 ng/mL. Serum creatine kinase (CK) and CK-MB values were 49 U/L (20 - 170) and 34 U/L (1 - 25), respectively in the blood sample during admission, and the peak values were 197 and 36 U/L. Fasting blood sugar, blood urea nitrogen (BUN), creatinine, especially INR, aPTT and PT time were in normal range. She was followed up for 9 days, and then discharged with the treatment of warfarin 5 mg per day and metoprolol 25 mg per day. The baby was stable in the neonate unite, and discharged with the mother.
 Click for large image | Figure 1. Electrocardiography of patient. |
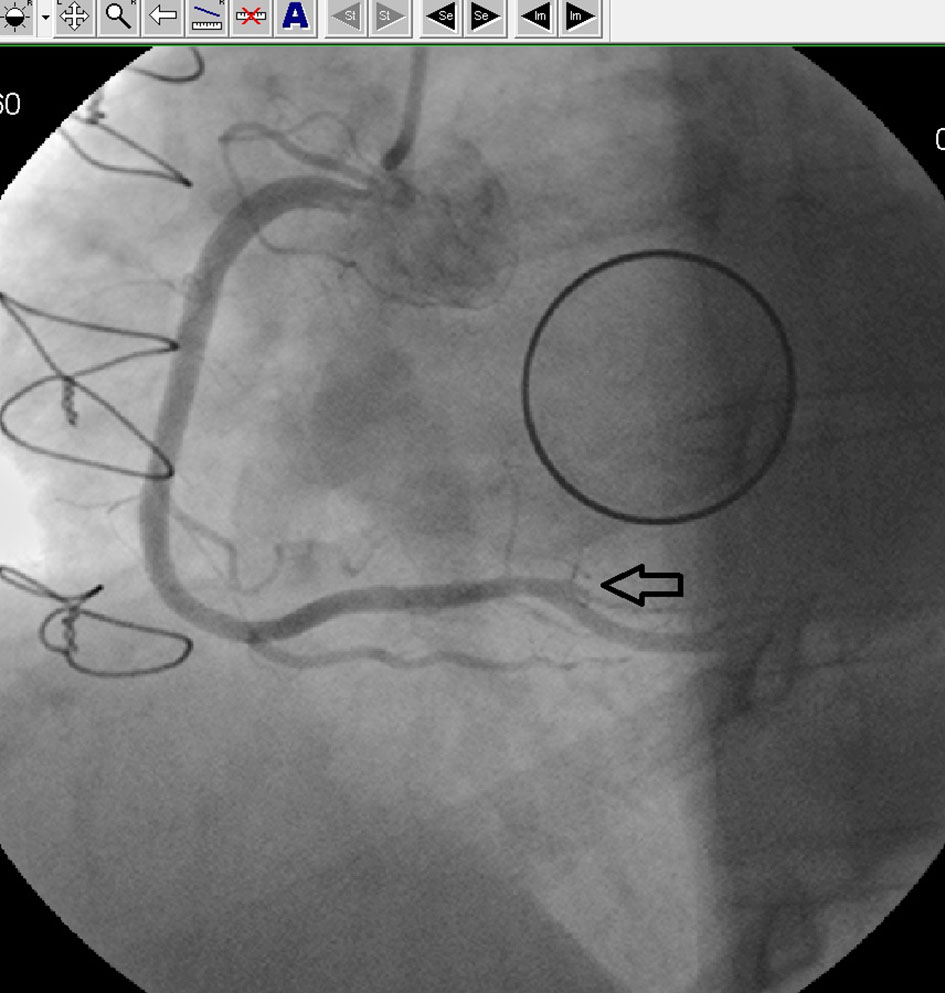 Click for large image | Figure 2. Coronary angiography of patient. |
| Discussion | ▴Top |
AMI may be observed in all trimesters of the pregnancy, but is more common in the third trimester and in the pregnant woman older than 33 years. Pregnancy MI is most common in the multigravida, and mostly localized at anterior wall. Twenty-nine percent of the coronary angiography patients had normal coronary arteries [4]. Atherosclerosis is the most common etiology of MI in the pregnancy, and observed in less than the half of the patients who had undergone coronary anatomy imaging [3]. According to the coronary angiography, our patient had a distal obstruction in PL branch of RCA. The other possible etiologies include thrombosis, coronary artery spasm, coronary artery dissection, Kawasaki disease, collagen vascular diseases, cocaine use, aortic and mitral prosthetic valve thrombosis and pheochromocytoma [5]. A study showed that 58% of the pregnant MI patients had cardiac risk factors. Smoking (20%) and hypertension (25%) are the most common risk factors, and the prevalence of diabetes mellitus (gestational or pregestational) is 3-5%. The prevalence of other risk factors including hypercholesterolemia, hyperlipidemia and obesity is less than 5% [1]. In our case, the etiology was identified as mitral prosthetic valve thrombosis which is an identified risk factor for MI during pregnancy. Therefore, oral anticoagulant was added to the treatment. Lower dose of aspirin can be used safely for MI during pregnancy [6]. There are no adequate data associated with abciximab and ticlopidine. ADP inhibitors cause platelet dysfunction in the fetus, and increase the risk of neonatal intracranial hemorrhage during vaginal delivery [7]. ST segment elevation MI is more common during pregnancy, but non-ST segment elevated MI was observed in only one case [8]. Our case was ST segment elevation inferior MI.
In conclusion, AMI prevalence is rare during pregnancy, but it is a serious life-threatening condition for the mother and the baby, therefore it should be noticed in the early period at the emergency department, and optimal treatment choices should be preferred for the mother and baby health.
Conflicts of Interest
We declared that we have no commercial, financial, and other relationships in any way related to the subject of this article all that might create any potential conflicts of interest.
Funding Support
None.
| References | ▴Top |
- Hankins GD, Wendel GD, Jr., Leveno KJ, Stoneham J. Myocardial infarction during pregnancy: a review. Obstet Gynecol. 1985;65(1):139-146.
pubmed - Badui E, Enciso R. Acute myocardial infarction during pregnancy and puerperium: a review. Angiology. 1996;47(8):739-756.
doi pubmed - Roth A, Elkayam U. Acute myocardial infarction associated with pregnancy. Ann Intern Med. 1996;125(9):751-762.
doi pubmed - Maekawa K, Ohnishi H, Hirase T, Yamada T, Matsuo T. Acute myocardial infarction during pregnancy caused by coronary artery spasm. J Intern Med. 1994;235(5):489-492.
doi pubmed - Iadanza A, Del Pasqua A, Barbati R, Carrera A, Gentilini R, Favilli R, Pierli C. Acute ST elevation myocardial infarction in pregnancy due to coronary vasospasm: a case report and review of literature. Int J Cardiol. 2007;115(1):81-85.
doi pubmed - Schomig A, Neumann FJ, Walter H, Schuhlen H, Hadamitzky M, Zitzmann-Roth EM, Dirschinger J, et al. Coronary stent placement in patients with acute myocardial infarction: comparison of clinical and angiographic outcome after randomization to antiplatelet or anticoagulant therapy. J Am Coll Cardiol. 1997;29(1):28-34.
doi - Valcamonico A, Foschini M, Soregaroli M, Tarantini M, Frusca T. Low dose aspirin in pregnancy: a clinical and biochemical study of effects on the newborn. J Perinat Med. 1993;21(3):235-240.
doi pubmed - G OSN, Garcia Martul M, Santana Cabrera L, Eugenio Robaina P, Hernandez Medina E, Sanchez Palacios M. [Acute coronary syndrome without ST elevation during pregnancy. A case report]. Med Intensiva. 2006;30(4):180-182.
pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


