| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 8, Number 8, August 2017, pages 241-242
Ultrasonographic Findings of Uterine Artery Pseudoaneurysm
Sayuri Kondoa, Shunji Suzukia, b
aDepartment of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, Tokyo, Japan
bCorresponding Author: Shunji Suzuki, Department of Obstetrics and Gynecology, Japanese Red Cross Katsushika Maternity Hospital, 5-11-12 Tateishi, Katsushika-ku, Tokyo 124-0012, Japan
Manuscript submitted June 26, 2017, accepted July 7, 2017
Short title: Uterine Artery Pseudoaneurysm
doi: https://doi.org/10.14740/jmc2867w
| Abstract | ▴Top |
A 30-year-old woman, gravid 1, para 1 underwent an emergency cesarean section (CS) at 40 weeks of gestation because of intrauterine infection. Seven hours after CS, sudden massive vaginal bleeding of 1,500 mL occurred. Transvaginal ultrasonography with color Doppler revealed the presence of low density cyst with a diameter of 4 cm with spiral pulsating blood flow in the cavity of the cyst in the vicinity of the ascending branches of the left uterine artery. We diagnosed it as uterine artery pseudoaneurysm, and total hysterectomy was performed because of unstable vital signs under transfusion.
Keywords: Uterine artery pseudoaneurysm; Cesarean section; Transvaginal ultrasonography
| Introduction | ▴Top |
Pseudoaneurysm is a dilation of an artery with partial or full disruption of the vessel wall [1-4]. Uterine artery pseudoaneurysm (UAP) is rare but a potentially life-threatening lesion. Although many clinical interventions have been postulated to be responsible for development of UAP, cesarean section (CS) has seemed to be the most frequent cause of UAP because CS has possibilities of causing vessel injuries involving branches of uterine arteries [3]. The initial usefulness of ultrasonography for suspecting UAP has been well documented [1, 2, 4]. The unexpected appearance of uterine anechoic lesions at ultrasonography can suggest the presence of UAP. The utilization of color Doppler seems to assist the confirmed diagnosis of UAP. Within the UAP, in addition, swirling arterial flow with different directions and velocities has been reported to be observed like the current case [2]. We present here a case of UAP following emergency CS diagnosed by ultrasonography.
| Case Report | ▴Top |
A 30-year-old woman, gravid 1, para 1 with no previous disease or family history underwent an emergency CS at 40 weeks of gestation because of intrauterine infection and fetal asphyxia. A male infant weighing 2,922 g was born with Apgar scores of 8 and 9 at 1 and 5 min, respectively. Histopathology of the placenta did not demonstrate any abnormal findings except acute funisitis with chorioamnionitis. Total blood loss during surgery was 500 mL. The clinical course until several hours after CS was uneventful without any further complications. Seven hours after CS, sudden massive vaginal bleeding of 1,500 mL occurred. The hemoglobin concentration decreased to 6.6 g/dL. And then, genital bleeding of about 1,000 mL/h persisted for 2 h. Transvaginal ultrasonography with color Doppler revealed the presence of low density cyst with a diameter of 4 cm with spiral pulsating blood flow in the cavity of the cyst in the vicinity of the ascending branches of the left uterine artery (Fig. 1). The arterial blood flows like a jet into the cavity during systole were also observed (Fig. 2).
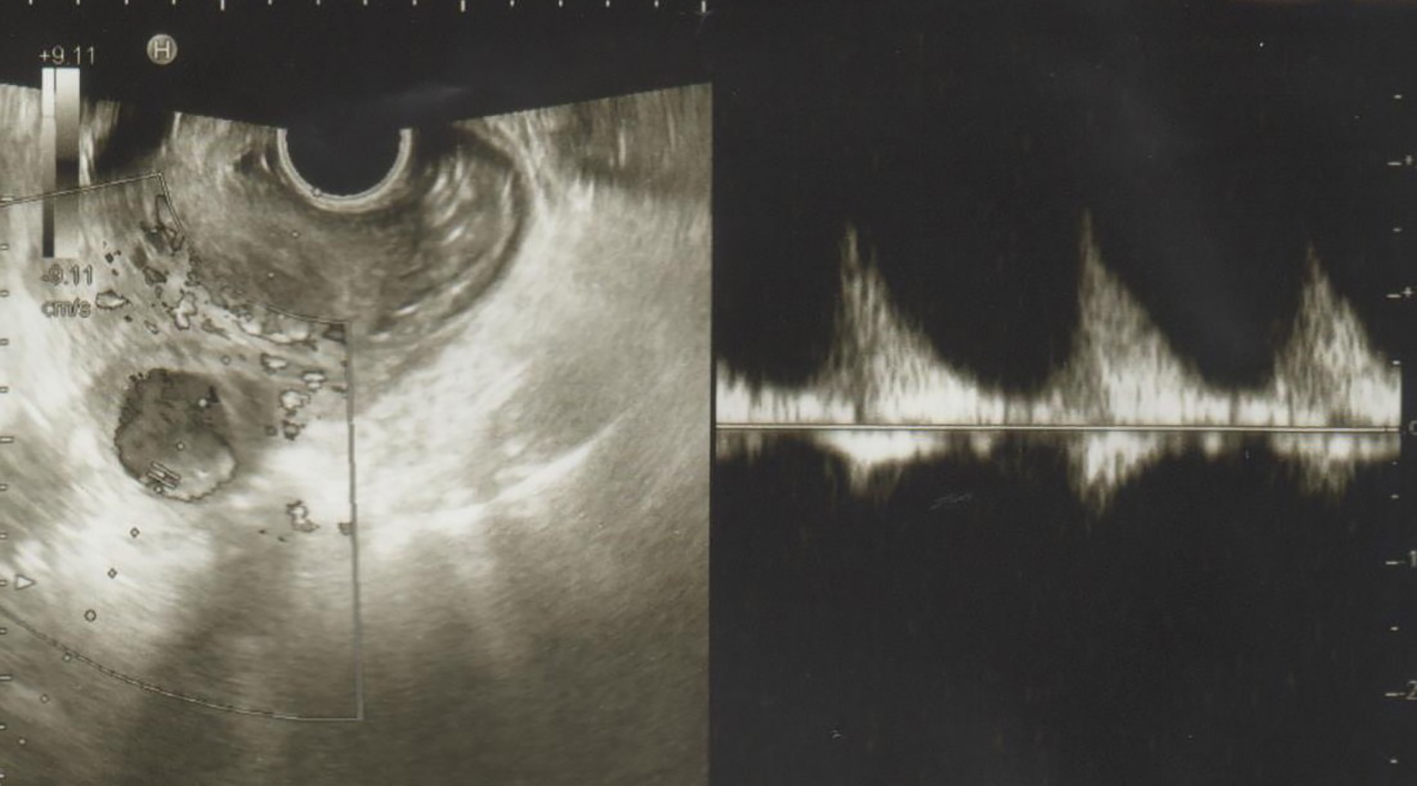 Click for large image | Figure 1. Transvaginal ultrasonography showing the presence of low density cyst with a diameter of 4 cm with spiral pulsating blood flow in the cavity of the cyst in the vicinity of the ascending branches of the left uterine artery. |
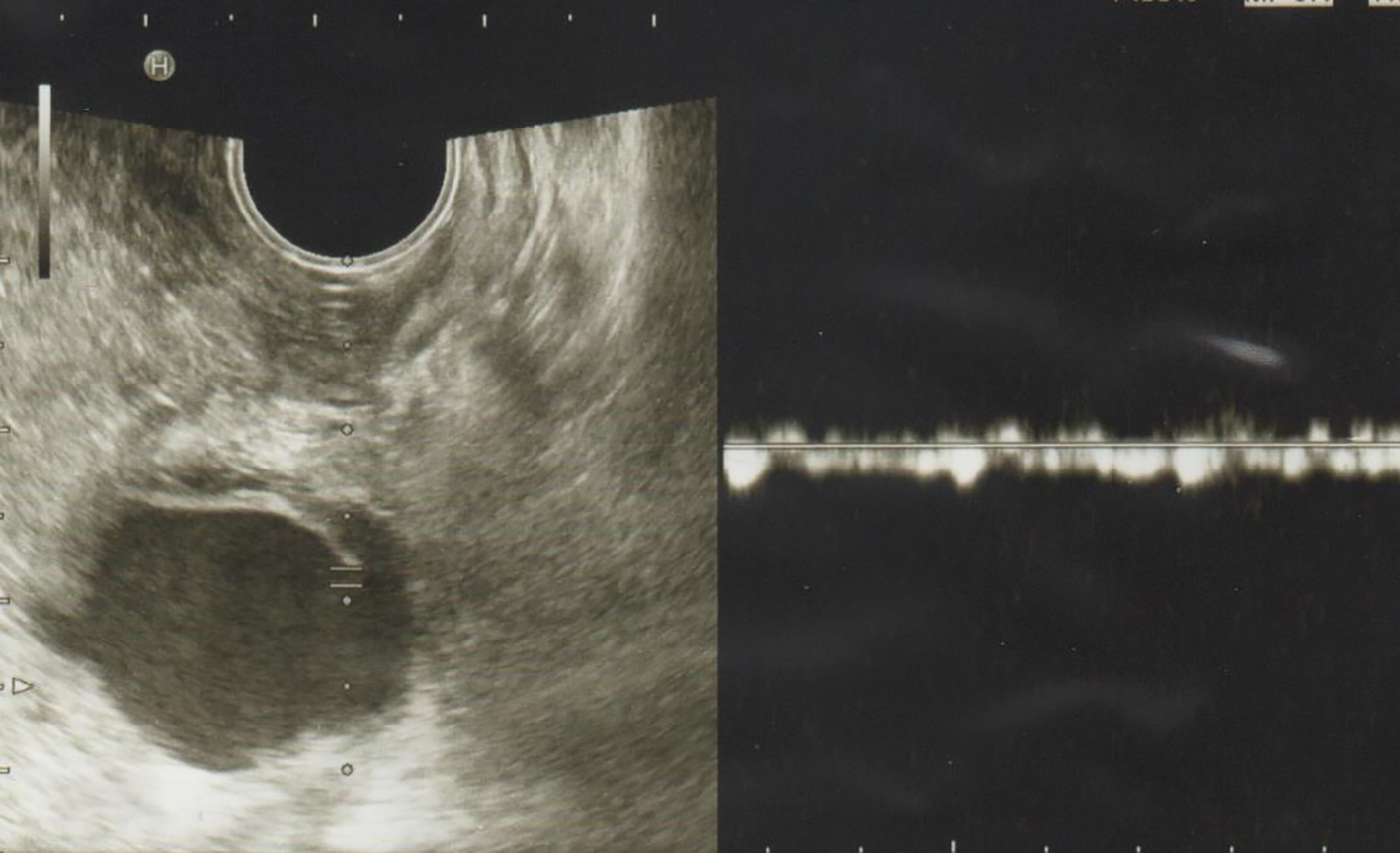 Click for large image | Figure 2. Transvaginal ultrasonography showing the arterial blood flows like a jet into the cavity during systole. |
We diagnosed it as UAP, and total hysterectomy was performed because of unstable vital signs under transfusion.
| Discussion | ▴Top |
In the current case, we were able to diagnose UAP only by ultrasonography; however, the diagnosed period seemed to be too late unfortunately. Gray-scale ultrasound findings show a well-defined complex echogenic mass different in appearance from the rest of the placenta. Prompt and accurate diagnosis should be made using color Doppler ultrasonography to avert life-threatening bleeding since it plays a significant role in demonstrating the vascular nature of this anechoic uterine lesion. If the earlier diagnosis of smaller UAP could be performed, an informed consent concerning arterial embolization might be possible to be performed. Based on the current case, we realized again the importance of prompt ultrasonographic examination in cases of massive postpartum hemorrhage.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
| References | ▴Top |
- Ciebiera M, Slabuszewska-Jozwiak A, Zareba K, Jakiel G. Management of uterine artery pseudoaneurysm: advanced ultrasonography imaging and laparoscopic surgery as an alternative method to angio-computed tomography and transarterial embolization. Wideochir Inne Tech Maloinwazyjne. 2017;12(1):106-109.
doi - Karmous N, Ayachi A, Derouich S, Mkaouar L, Mourali M. Rupture of uterine artery pseudoaneurysm: role of ultrasonography in postpartum hemorrhage management. Pan Afr Med J. 2016;25:136.
doi pubmed - Lausman AY, Ellis CA, Beecroft JR, Simons M, Shapiro JL. A rare etiology of delayed postpartum hemorrhage. J Obstet Gynaecol Can. 2008;30(3):239-243.
doi - Zimon AE, Hwang JK, Principe DL, Bahado-Singh RO. Pseudoaneurysm of the uterine artery. Obstet Gynecol. 1999;94(5 Pt 2):827-830.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


