| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 9, Number 3, March 2018, pages 92-95
The Effect of Sprayable Adhesion Barriers in Revisional Obesity Surgery
Ahmed Arifur Rahman
St George Hospital, Kogarah, NSW 2217, Australia
Manuscript submitted January 23, 2018, accepted January 29, 2018
Short title: Effect of Adhesive Barrier
doi: https://doi.org/10.14740/jmc3008w
| Abstract | ▴Top |
Revision bariatric surgery is technically demanding and associated with high morbidity rates due to formation of adhesions and distortion of proximal gastric anatomy. Two cases of failed gastric band were presented who required gastric sleeve. The patient who received adhesive barrier during removal of the band had less adhesion during the second procedure. This finding leads to a study to assess whether the application of an adhesion barrier film onto the operative field after the removal of the gastric band had any impact on the number and amount of adhesions at the time of the revision surgery after failed gastric banding. A study with 19 patients having band removal followed by sleeve gastrectomy 3 months later was performed. The patients were randomized to either a control group (11 patients) who received band removal only or an active group (eight patients) who had a sprayable adhesion barrier applied at the time of band removal. The second procedures for both groups were independently graded for adhesions. All procedures were recorded and were assessed in a blind fashion as to the severity of adhesions (grade 1 - 5). The total adhesion score for the control group (n = 11) was 32 (mean 2.82). The active group (n = 8) had a total adhesion score of 12 (mean 1.5). Statistical adhesion scored P = 0.05. The average operative time for the control group and active group was 73 and 56 min (P = NS). In our study, an adhesion barrier leads to a statistically significant reduction in adhesion formation and operative time. This warrants consideration of a larger trial to assess whether adhesion barriers may reduce morbidity in re-operative bariatric surgery.
Keywords: Adhesion barrier; Adhesion; Obesity surgery
| Introduction | ▴Top |
Revision bariatric surgery is technically demanding and associated with high morbidity rates due to formation of adhesions and distortion of proximal gastric anatomy. Adhesion can vary from minor to complex fibrotic tissue that leads to loss of surgeons’ ability to definitive anatomical tissue plane that can cause increased operative time and risk of surgical trauma. There are different consequences of adhesion. For bariatric procedures involved foregut, abdominal pain and bowel obstruction from adhesion are uncommon but adhesion may cause increased operative time and surgical risk [1].
| Case Reports | ▴Top |
Typical cases
Case 1
A 45-year-old female presented with reflux and failure to weight loss 14 months after gastric banding. Decision was made to precede for gastric sleeve. Gastric band was removed initially as primary procedure followed by gastric sleeve after 3 months. During the second procedure (gastric sleeve), significant adhesion was found in upper abdomen that made the procedure difficult and prolonged.
Case 2
Another 35-year-old female presented with failed gastric band. Adhesive barrier was used during removal of gastric band. During the second procedure (gastric sleeve) after 3 months, there was less adhesion in comparison to the first case.
Considering these two cases, a study was conducted on similar cases to observe the effect of adhesive barriers on revision bariatric surgery.
Case series study
Participants
The actual study was introduced to 30 patients undergoing removal of gastric band. Nineteen have gone through the study having band removal followed by sleeve gastrectomy 3 month later (Table 1). Others were waiting for further procedures or follow-up or had other bariatric procedures rather than sleeve gastrectomy.
 Click to view | Table 1. Participants of the Study |
Design
A prospective, single-center, controlled, single-blinded, randomized study was conducted. Patient blinding was performed intra-operatively through a third person with externally prepared randomization using envelopes. To blind the reviewer to subject and treatment, all videos were assigned a unique blind code.
Interventions
The patients were randomized intra-operatively when they had their gastric band removed to either a control group (11 patients) who received band removal only or the active group (eight patients) who had a sprayable adhesion barrier applied at the time of band removal, using not more than one kit [2]. The second procedures (sleeve gastrectomy) for both groups were independently graded for adhesions. All procedures were recorded and were assessed in a blind fashion as to the severity of adhesions (grade 1 - 5).
Outcome
The primary outcome with respect to efficacy was the incidence, severity of adhesion and time required for the second procedure (sleeve gastrectomy) scored by a single reviewer.
Statistical analysis
The primary endpoint was the severity of adhesion and duration of second procedure. We calculated means and standard deviations and used a two-sample t-test to identify differences in means between participants in each group. P < 0.05 was considered significant for all comparisons. Statistical analyses were performed using SPSS.
Results
Adhesion score was grade from 1 to 5 for each control group (n = 11) and active (n = 8) group. For the active group, the score was 1 to 2. On the other hand, it averaged from 3 to 5 for the control group (Fig. 1). Total adhesion score for control group was 32 and for the active group was 12 (Fig. 2). Unpaired t-test results showed P value and statistical significance. The two-tailed P value was 0.0464. By conventional criteria, this difference was considered to be statistically significant. The average operative time for control group was 73 min and for active group was 56 min (Figs. 3 and 4).
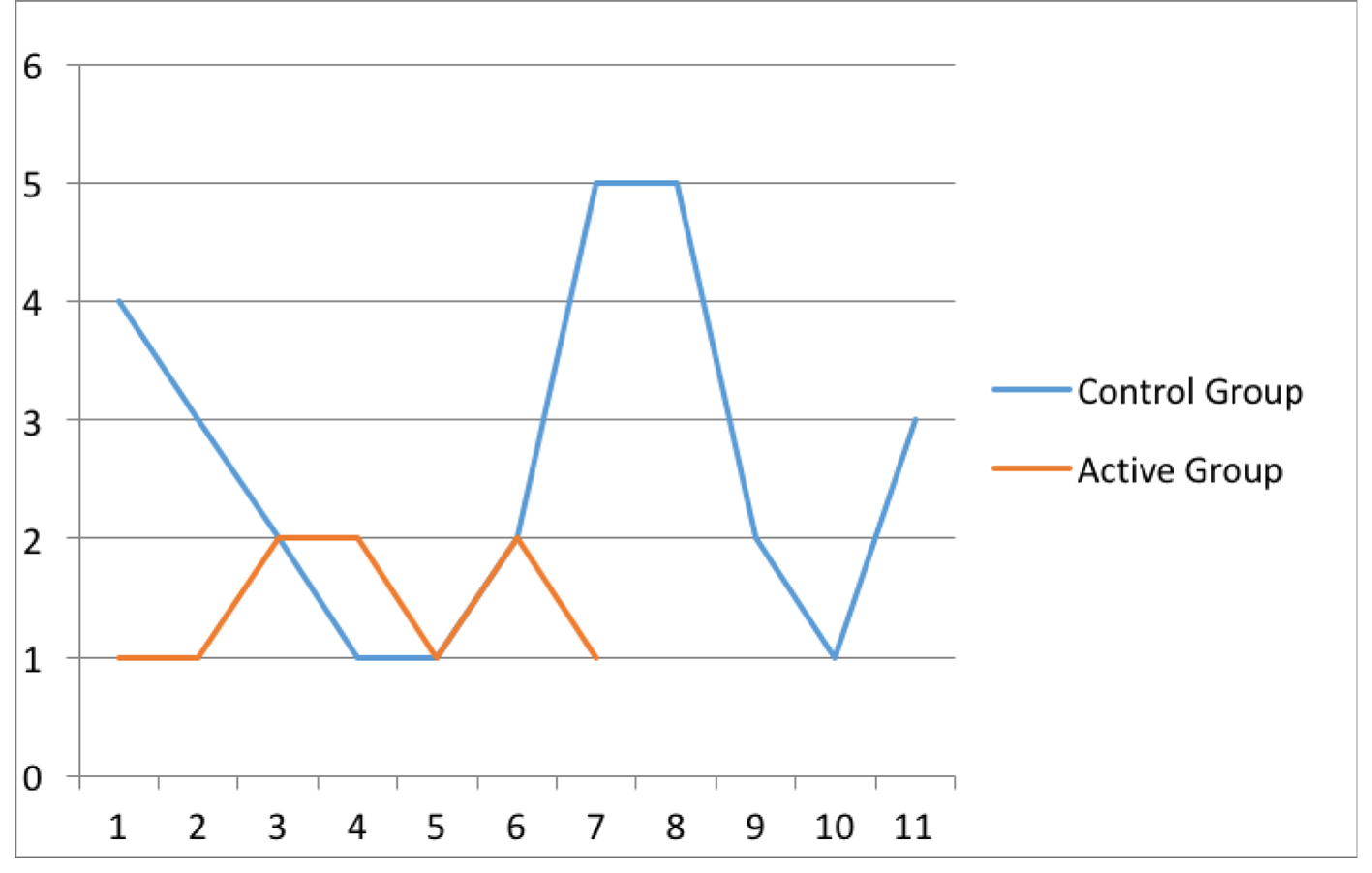 Click for large image | Figure 1. Adhesion score grade 1 - 5. |
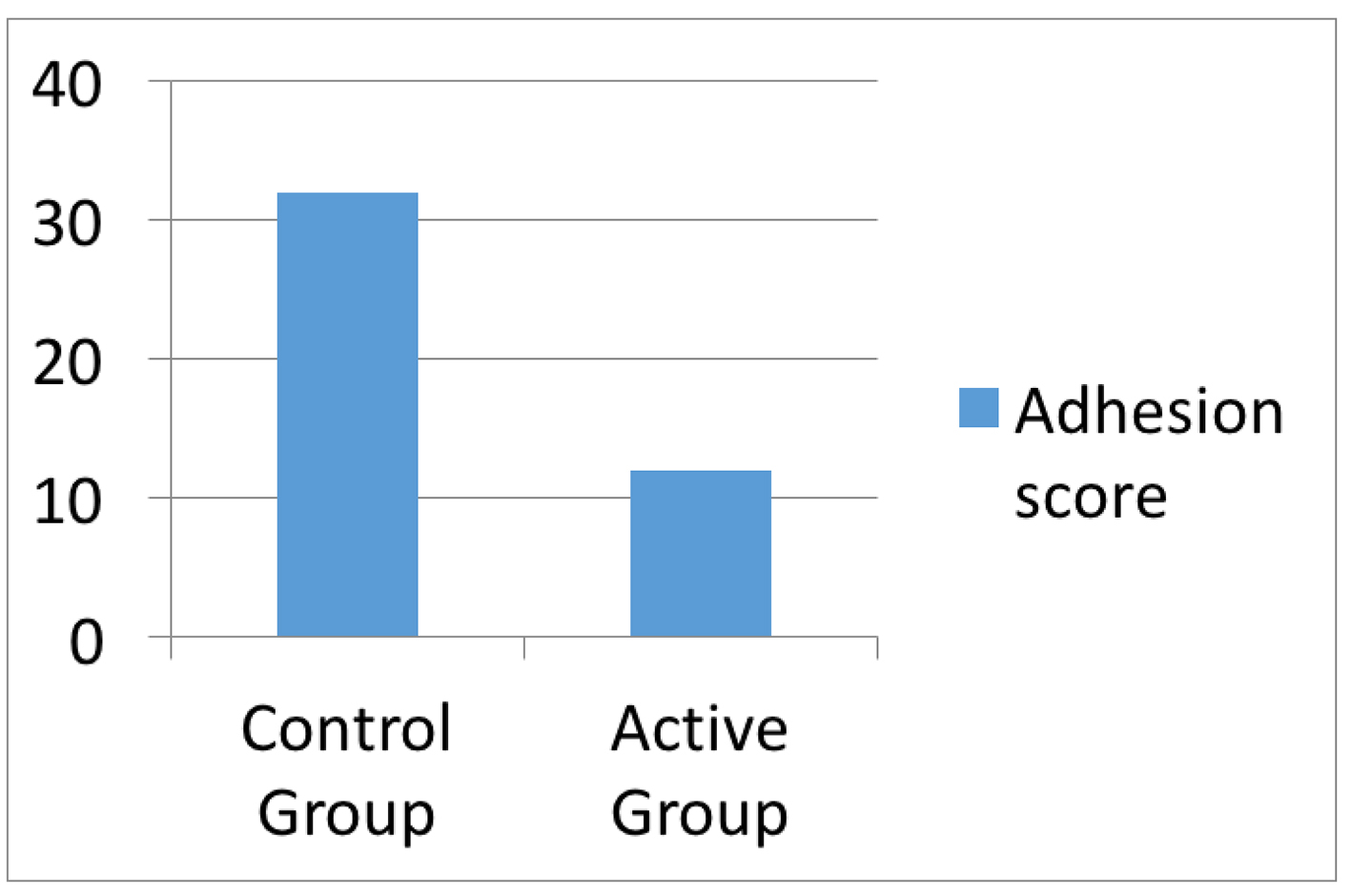 Click for large image | Figure 2. Total adhesion score. |
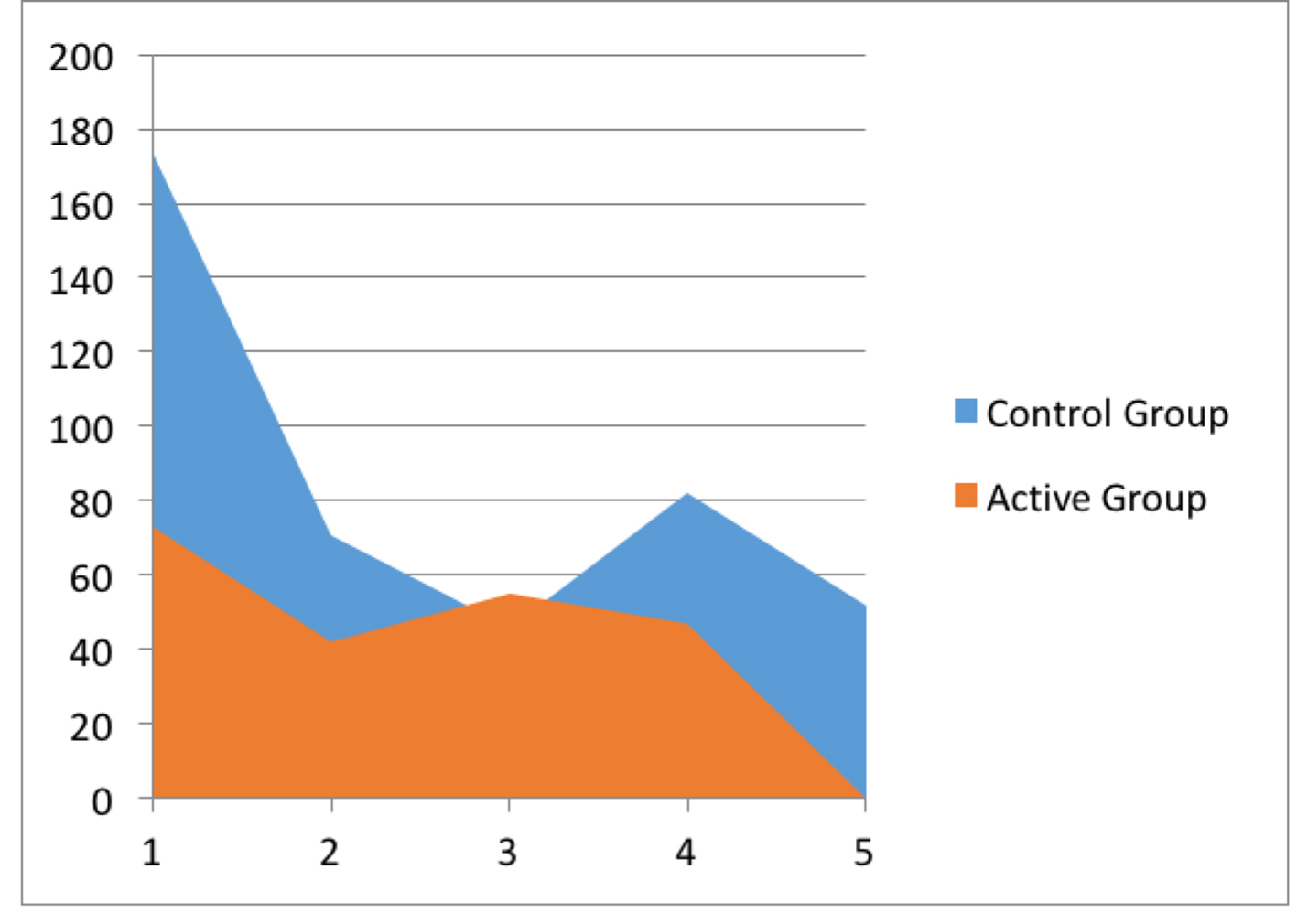 Click for large image | Figure 3. Operative time. |
 Click for large image | Figure 4. Average operative time. |
| Discussion | ▴Top |
There was a systemic review and meta-analysis for benefits and harms of adhesion barriers for abdominal surgery [3]. They searched PubMed, CENTRAL, and Embase for randomized clinical trials assessing use of oxidized regenerated cellulose, hyaluronate carboxymethylcellulose, icodextrin, or polyethylene glycol in abdominal surgery. The primary outcome was reoperation for adhesive small bowel obstruction. Their search returned 1,840 results, from which 28 trials (5,191 patients) were included. No trials reported data for the effect of oxidized regenerated cellulose or polyethylene glycol on reoperations for adhesive small bowel obstruction. Oxidized regenerated cellulose reduced the incidence of adhesions. No barriers were found to be associated with an increase in serious adverse events.
Adhesions are the most frequent complications of abdominopelvic surgery [2] and a life-time risk of small bowel obstruction with considerable morbidity and mortality [2-5]. Adhesion increases the risk of admission to hospital for related complications following gynecological procedures and up to 56% of all patients are in need of further surgery [6]. In clinical and autopsy studies of patients who had prior laparotomies, the incidence of intra-abdominal adhesions was 70-90% [7].
Evidence-based practice of adhesive barrier is poor. There are different methods of adhesive barrier. In our study ,we used SprayShield adhesion barrier because 1) the only adhesion barrier with a unique blue color can easily be seen during laparoscopic surgery; 2) the air assisted sprayer and flow regulator provide an accurate and controlled delivery of hydrogel to the application site during surgery; and 3) it polymerizes rapidly and gently, forming a flexible, tissue adherent, smooth and lubricious adhesion barrier. The barrier allows adjacent surfaces and organs to move freely over protected areas, allowing natural healing. Though SprayShield is no longer regularly practiced and available in Australia as it is sold to other company towards the end of our study but there are other adhesive barriers available in market with similar property. This is suitable for multiple site abdominopelvic protection in laparoscopic surgery, complex anatomy and dry surfaces.
A variety of adhesion prophylaxes have been investigated to reduce occurrence and severity of adhesion formation. Antiadhesion barriers basically fall under two main categories: macromolecular solutions and mechanical devices (Table 2) [8].
 Click to view | Table 2. Adhesive Barriers |
Hydrogel spray gel, which is similar to SprayShield, and which forms a solid, flexible, absorbable hydrogel, has demonstrated efficacy in a population of patients known to be particularly at risk of adhesion formation [9].
Conclusion
In our study, an adhesion barrier leads to a statistically significant reduction in adhesion formation and operative time. There are many research projects before to see the outcome of adhesive barrier mainly for gynecological and colorectal surgeries but not for bariatric procedures. This warrants consideration of a larger trial to assess whether adhesion barriers may reduce morbidity in re-operative bariatric surgery.
Conflict of Interest
None.
Funding
This research did not receive any specific grant from funding agencies.
Ethical Declaration
Compliance with Ethical Standards.
Informed Consent
Informed consent was taken from the patients.
Author Contributions
Ahmed Arifur Rahman: data collection, analyzing and interpreting the data; writing manuscript; approving final version of the manuscript.
| References | ▴Top |
- Wilson MS, Ellis H, Menzies D, Moran BJ, Parker MC, Thompson JN. A review of the management of small bowel obstruction. Members of the Surgical and Clinical Adhesions Research Study (SCAR). Ann R Coll Surg Engl. 1999;81(5):320-328.
pubmed - Lundorff P, Brolmann H, Koninckx PR, Mara M, Wattiez A, Wallwiener M, Trew G, et al. Predicting formation of adhesions after gynaecological surgery: development of a risk score. Arch Gynecol Obstet. 2015;292(4):931-938.
doi pubmed - Ten Broek RPG, Stommel MWJ, Strik C, van Laarhoven C, Keus F, van Goor H. Benefits and harms of adhesion barriers for abdominal surgery: a systematic review and meta-analysis. Lancet. 2014;383(9911):48-59.
doi - ten Broek RP, Issa Y, van Santbrink EJ, Bouvy ND, Kruitwagen RF, Jeekel J, Bakkum EA, et al. Burden of adhesions in abdominal and pelvic surgery: systematic review and met-analysis. BMJ. 2013;347:f5588.
doi pubmed - Okabayashi K, Ashrafian H, Zacharakis E, Hasegawa H, Kitagawa Y, Athanasiou T, Darzi A. Adhesions after abdominal surgery: a systematic review of the incidence, distribution and severity. Surg Today. 2014;44(3):405-420.
doi pubmed - Ellis H. The causes and prevention of intestinal adhesions. Br J Surg. 1982;69(5):241-243.
doi pubmed - Ellis H, Moran BJ, Thompson JN, Parker MC, Wilson MS, Menzies D, McGuire A, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999;353(9163):1476-1480.
doi - Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL. Peritoneal adhesions: etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg. 2001;18(4):260-273.
doi pubmed - Mettler L, Audebert A, Lehmann-Willenbrock E, Schive-Peterhansl K, Jacobs VR. A randomized, prospective, controlled, multicenter clinical trial of a sprayable, site-specific adhesion barrier system in patients undergoing myomectomy. Fertil Steril. 2004;82(2):398-404.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


