| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 2, Number 6, December 2011, pages 262-264
Esophageal Stent Migration Into Trachea
Yi-Ying Chianga, b, Mei-Hui Yangc, Hung-Yu Changa, b, Chia-Chen Chena, b, Chia-Wen Chena, b, Kuen-Bao Chena, d, e
aDepartment of Anesthesiology, China Medical University Hospital, No.2, Yude Road, North District, Taichung City 404, Taiwan (R.O.C.)
bChina Medical University, No.91 Hsueh-Shih Road, Taichung, Taiwan 404, Taiwan (R.O.C.)
cDepartment of Anesthesia, Lin Shin Hospital, No.36, Sec. 3, Huizhong Road, Nantun District, Taichung City 408, Taiwan (R.O.C.)
dCollege of Medicine, China Medical University, No.91 Hsueh-Shih Road, Taichung, Taiwan 404, Taiwan (R.O.C.)
eCorresponding author: Kuen-Bao Chen, Department of Anesthesiology, China Medical University Hospital, No. 2, Yude Road, North District, Taichung City 404, Taiwan (R.O.C.)
Manuscript accepted for publication August 23, 2011
Short title: Esophageal Stent Migration into Trachea
doi: https://doi.org/10.4021/jmc303w
| Abstract | ▴Top |
We reported a case of esophageal cancer in which an esophageal stent was placed for treatment of a malignant stricture. A tracheoesophageal fistula and stent migration into the trachea were noted on post-procedure day 11 before the placement of a feeding gastrostomy. Because of the possibility of stent-related tracheoesophageal fistula, whether surgical feeding gastrostomy or endoscopic stent placement is of benefit for patients with malignant esophageal stenosis requires careful evaluation.
Keywords: Tracheoesophageal Fistula; Stents; Esophageal neoplasms; Esophageal stenosis; Gastrostomy
| Introduction | ▴Top |
Tracheoesophageal fistula (TE fistula) is a known comorbidity of esophageal malignancy as the disease progresses with an incidence of 5% [1, 2]. Esophageal stenting has been used to manage TE fistula [3, 4]. However, iatrogenic TE fistula due to the stenting procedure could occur with imminent threat of life [4].Through this case, we would like to emphasize that making the decision between alternative modalities to cope with esophageal malignancy with obstruction should involve serious consideration of possible complications.
| Case Report | ▴Top |
A 56-year-old male presented for feeding gastrostomy due to malignant stricture of the esophagus. Esophagogram revealed a 12.3 cm narrowing of the esophagus beginning at the level of the thoracic inlet. Endoscopic stenting was arranged 6 months after diagnosis due to progressive dysphagia not responding to concurrent chemoradiotherapy. During the procedure, stenosis was encountered at 17 cm from the incisor; the endoscope (GIF Q240, Olympus, Tokyo, Japan) with an outer diameter of 10.2 mm could not be passed. Using a wire-guided catheter technique and concurrent endoscopic and fluoroscopic monitoring [2], a 12 cm long, 28/23mm wide self-expandable metal stent (Ultraflex, Boston Scientific, Natick, MA, USA) was implanted. Post-procedure day 7, due to postprandial cough after liquid intake, feeding gastrostomy was arranged on post-procedure day 11.
The patient presented to the operating room with inspiratory stridor and supraclavicular retraction. Bronchoscope-guided nasal intubation was planned. The patient was pre-oxygenated with an O2 mask and was premedicated with intravenous midazolam 2 mg. However, as the patient became sedated, intermittent assisted mask ventilation was needed during bronchoscopy to prevent desaturation. Bronchoscopy revealed the stent to be exposed through a tracheoesophageal fistula (Fig. 1). The patient was intubated under bronchoscopy guidance and transferred to the intensive care unit (ICU). Computed tomography confirmed esophageal stent migration into the trachea via a 4 cm diameter fistula (Fig. 2). Post-procedure day 15, the family refused further treatment and the patient was discharged.
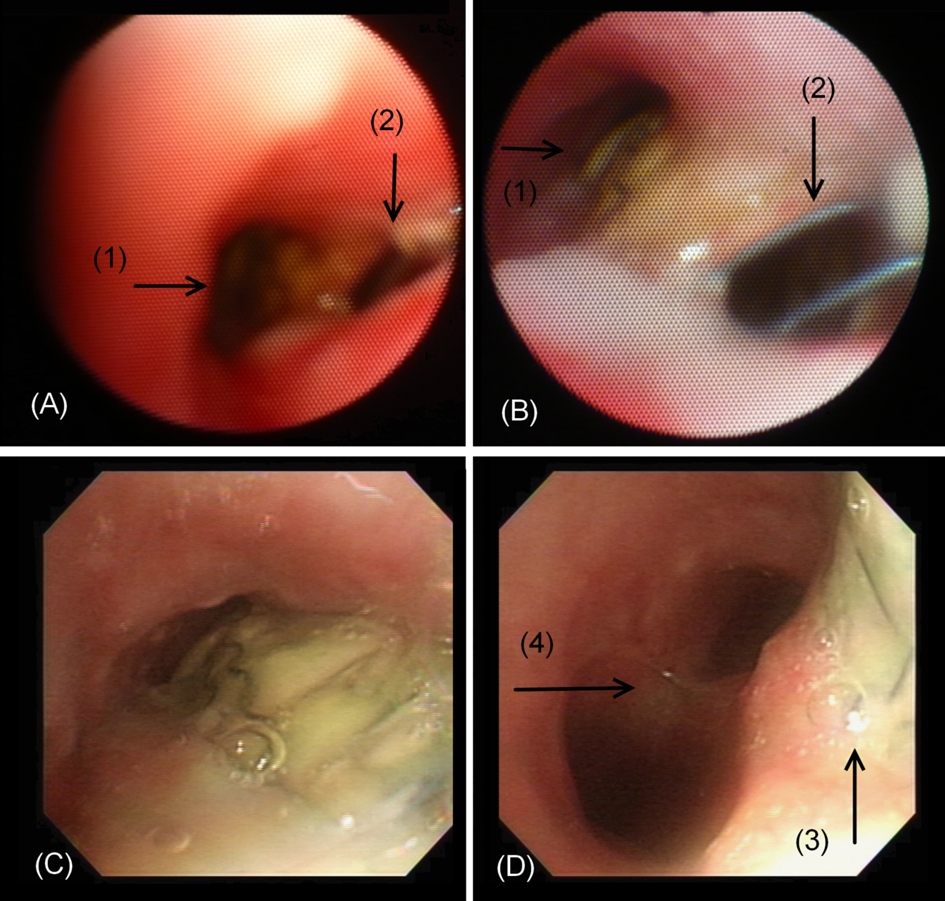 Click for large image | Figure 1. Bronchoscopy findings. (A) The bifurcation of tracheal lumen (1) and the TE fistula (2) mimicking the carina. (B) Close-up view of the tracheal lumen (1) showed the stent exposed through the TE fistula (2). (C) Advancing along the stenotic trachea lumen revealed the tracheal mucosal defect with stent exposure. (D) The tracheal mucosal defect with stent exposure (3) and the true carina (4). |
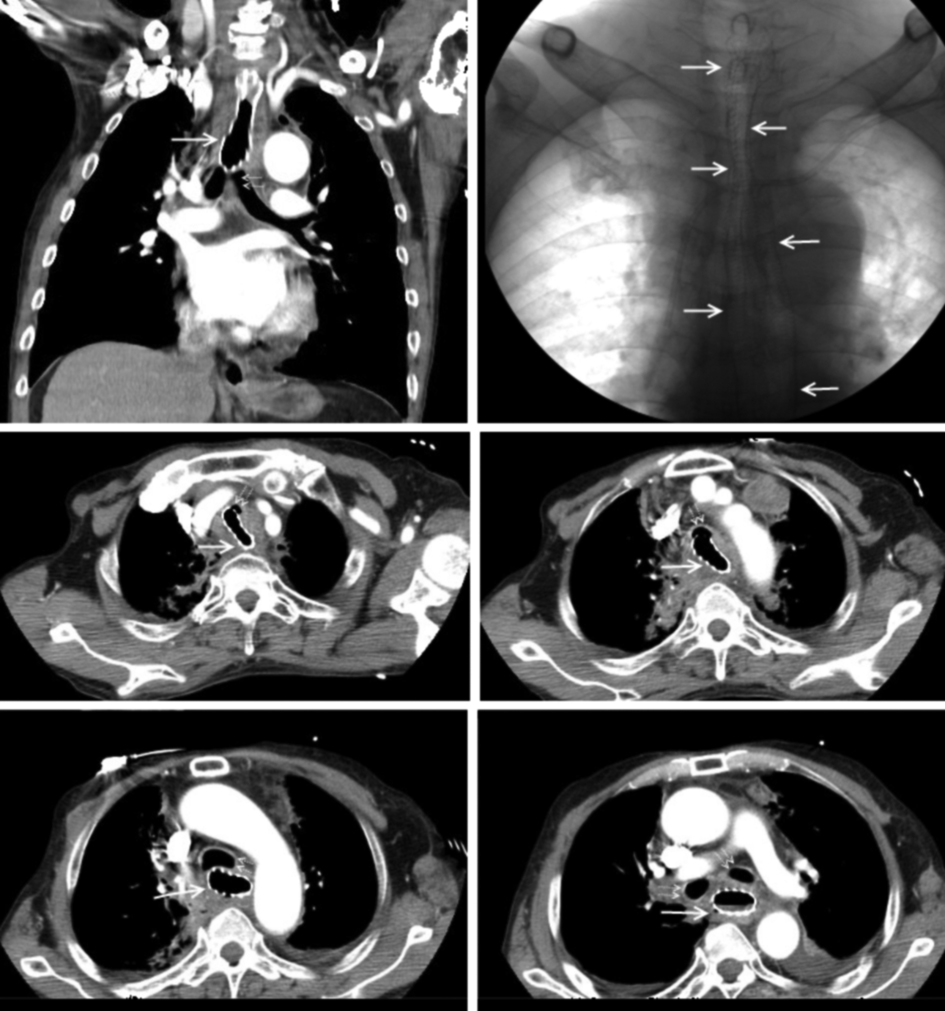 Click for large image | Figure 2. Computed tomography and fluoroscopy images (Solid arrows show the esophageal stent. Dotted double arrows indicate the airway, including the trachea and main bronchus). |
| Discussion | ▴Top |
Patients with inoperable esophageal malignancy who receive palliative stents for esophageal obstruction have a reported 120-day survival of 40% [1]. Mean time to death following stent placement ranges from 77 to 318 days [5, 6].
Once the TE fistula had developed, the feeding gastrostomy under general anesthesia became difficult because airway management was challenging due to the fistula. Positive pressure ventilation was another problem encountered due to the fistula. Complications occur in 26.8% of patients who undergo self-expanding metal stents placement for esophageal malignancies [7]. Procedure-related mortality is reported to be 4.8% [7], and mortality related to the complications of stent placement is approximately 15% [7, 8]. The Ultraflex stent has a lower overall complication rate as compared to the Gianturco stent or Wallstent [8].
Wang et al [8] reported a higher incidence for life-threatening complication in patients with stent placement in the proximal third of the esophagus, while Sarper et al [7] reported a higher complication rate for stent placement in the distal third. The incidence of post-stenting TE fistula has not been shown to differ between types of stents [2]. In patients in whom TE fistula occurs, survival from the diagnosis of TE fistula rarely exceed 30 days [2]. Taking the risk of stent-related complications into consideration, further investigation is needed to identify the risk factors for stent-related TE fistula to properly select candidates of esophageal stenting for malignant stenosis.
Malignant stenosis is a complication of esophageal cancer as the disease progresses. TE fistula may also occur in advanced cases. Endoscopic stenting is used for both malignant stenosis and TE fistula. However, it may lead to iatrogenic TE fistula formation with stent migration, a fatal complication. Although an endoscopic procedure is a less invasive palliative procedure, the risk-benefit should be weighted carefully against surgical feeding gastrostomy.
Conflict of Interests
We declare that the content has not been previously published and has been submitted solely to Journal of Medical Cases. All authors have participated sufficiently in the intellectual content and the analysis of data. Each author has reviewed the final version of the manuscript and approves it for publication. We declare no conflict of interest.
| References | ▴Top |
- Christie NA, Buenaventura PO, Fernando HC, Nguyen NT, Weigel TL, Ferson PF, Luketich JD. Results of expandable metal stents for malignant esophageal obstruction in 100 patients: short-term and long-term follow-up. Ann Thorac Surg. 2001;71(6):1797-1801; discussion 1801-1792.
pubmed - Saranovic D, Djuric-Stefanovic A, Ivanovic A, Masulovic D, Pesko P. Fluoroscopically guided insertion of self-expandable metal esophageal stents for palliative treatment of patients with malignant stenosis of esophagus and cardia: comparison of uncovered and covered stent types. Dis Esophagus. 2005;18(4):230-238.
pubmed doi - Ott C, Ratiu N, Endlicher E, Rath HC, Gelbmann CM, Scholmerich J, Kullmann F. Self-expanding Polyflex plastic stents in esophageal disease: various indications, complications, and outcomes. Surg Endosc. 2007;21(6):889-896.
pubmed doi - Cwikiel W, Tranberg KG, Cwikiel M, Lillo-Gil R. Malignant dysphagia: palliation with esophageal stents—long-term results in 100 patients. Radiology. 1998;207(2):513-518.
pubmed - De Palma GD, di Matteo E, Romano G, Fimmano A, Rondinone G, Catanzano C. Plastic prosthesis versus expandable metal stents for palliation of inoperable esophageal thoracic carcinoma: a controlled prospective study. Gastrointest Endosc. 1996;43(5):478-482.
pubmed doi - Lee SH. The role of oesophageal stenting in the non-surgical management of oesophageal strictures. Br J Radiol. 2001;74(886):891-900.
pubmed - Sarper A, Oz N, Cihangir C, Demircan A, Isin E. The efficacy of self-expanding metal stents for palliation of malignant esophageal strictures and fistulas. Eur J Cardiothorac Surg. 2003;23(5):794-798.
pubmed doi - Wang MQ, Sze DY, Wang ZP, Wang ZQ, Gao YA, Dake MD. Delayed complications after esophageal stent placement for treatment of malignant esophageal obstructions and esophagorespiratory fistulas. J Vasc Interv Radiol. 2001;12(4):465-474.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


