| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 9, Number 5, May 2018, pages 135-138
Primary Intracranial Mesenchymal Chondrosarcoma: A Case Report
Hyokrae Cho
Department of Neurosurgery, Kosin University Gospel Hospital, 262 Gamcheon-ro, Seo-gu, Busan, 602-702, Korea
Manuscript submitted March 14, 2018, accepted April 3, 2018
Short title: Intracranial Chondrosarcoma
doi: https://doi.org/10.14740/jmc3040w
| Abstract | ▴Top |
Mesenchymal chondrosarcoma is a rare malignancy characterized by a biphasic pattern of small undifferentiated round cells intermixed with island of well-differentiated cartilaginous matrix. Although this type of tumor exhibits widespread distribution in the body, intracranial mesenchymal chondrosarcoma is rare. Radical excision of intracranial mesenchymal chondrosarcoma is important for obtaining a positive prognosis but the effectiveness of chemotherapy and radiotherapy remains uncertain. An 18-year-old patient presented with generalized seizure with magnetic resonance imaging showing a large dura-attached solid mass in the frontal convexity, which was presumptively diagnosed as a meningioma. Gross total resection of tumor was achieved without postoperative deficit. The final histological diagnosis was extra-skeletal mesenchymal chondrosarcoma, grade I. There was no adjuvant treatment after surgery. Five years after surgery, the prognosis was good after gross total resection only; however, long-term follow-up is necessary in the future.
Keywords: Intracranial; Mesenchymal chondrosarcoma; Radical excision
| Introduction | ▴Top |
Intracranial mesenchymal chondrosarcomas are rare, high-grade malignant tumors with a high local recurrence rate that undergo distant metastasis, especially to the lungs and bones. These lesions arise from the synchondroses of the basilar skull bones, and also occur in association with the meninges along the falx cerebri, tentorium, and convexity [1, 2]. Due to their rarity, there is no data regarding the specific prognosis of intracranial mesenchymal chondrosarcomas. The role of chemotherapy or radiotherapy is not well established. In this case report, we described the outcome of a patient with intracranial mesenchymal chondrosarcoma that was completely removed without adjuvant therapy.
| Case Report | ▴Top |
An 18-year-old female was brought to our hospital with attack of generalized tonic type seizures. The patient had developed generalized seizures over the previous 3 years, and also occasionally suffered from severe headaches. At that time, she did not visit medical clinic without reason. The patient’s previous medical history was non-specific, and on general appearance the patient looked healthy. Her neurological status was normal. A preoperative magnetic resonance imaging (MRI) of the brain revealed a huge elliptical shaped extra-axial mass located behind the bifrontal bone with severe compression of the adjacent ventricle. The size of the lesion measured 7.5 × 5 × 7.5 cm in length. A cystic component was also identified at the center of the lesion. The lesion showed heterogeneous enhancement on MRI after gadolinium administration (Fig. 1 a, b). Computed tomography (CT) scan highlighted a spot-like calcification at the posterior margin of the tumor (Fig. 1c). An angiogram was not performed. Preoperatively, meningioma was considered as the presumptive diagnosis. A bicoronal frontal craniotomy was performed for gross total removal of the tumor. During the craniotomy, a yellow-whitish and hard tumor with an oval shape was seen after opening the dura. The tumor had good cleavage plane. They were attached to the dura and compressed the underlying brain without invading it (Fig. 2a). The tumor was completely removed.
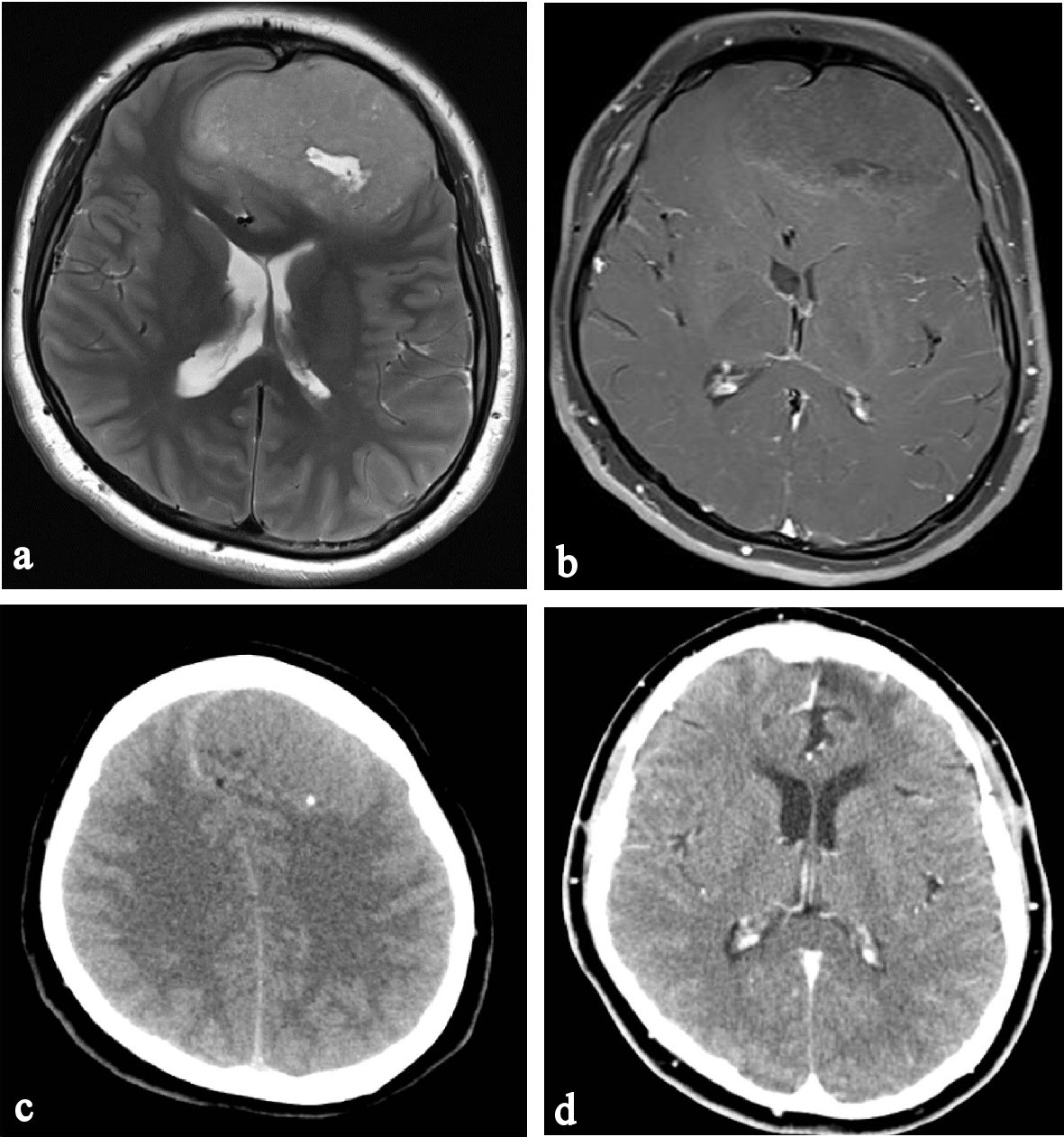 Click for large image | Figure 1. Preoperative MRI, CT and postoperative CT. (a) Cystic component at a tumor center of frontal convexity. (b) Heterogeneous enhancement of tumor after IV gadolinium. (c) Spot-like calcification of posterior tumor margin. (d) Tumor recurrence is not found on enhanced axial CT image 4 years post surgery. |
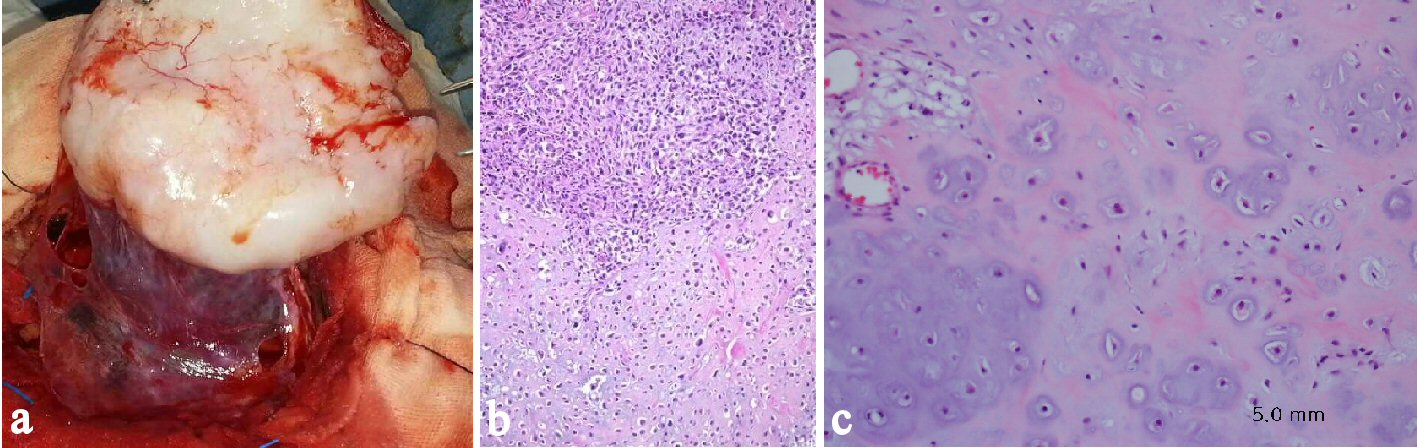 Click for large image | Figure 2. Intraoperative photograph and histological findings. (a) The tumor margin is clear without invasion. (b) The specimen showing a biomorphic appearance-area of well-differentiated hyaline cartilage juxtaposed to undifferentiated stroma (H&E × 100). (c) The cartilaginous components are composed of atypical chondrocytes with nuclear pleomorphism and mitosis in lacunae (H&E × 200). |
Histological examination of the tumor revealed a well-differentiated extra-skeletal mesenchymal chondrosarcoma, grade I (Fig. 2b, c). The postoperative course was non-eventful. A PET scan was also performed to detect primary origin or secondary lesion, the findings of which were normal. Postoperative radiotherapy and adjuvant chemotherapy was not administered. There was no recurrence of CT at 5 years postoperatively (Fig. 1d).
| Discussion | ▴Top |
Intracranial mesenchymal chondrosarcoma accounts for less than 0.16% of all intracranial neoplasms. This type of tumor can occur throughout the central nervous system (CNS), and is one of three histopathologically distinct chondrosarcoma subtypes, namely, mesenchymal, classic, and myxoid variants [1]. The grading system of the World Health Organization (WHO) consists of three categories: grade I (well differentiated), grade II (moderately differentiated) and grade III (poor differentiated) [3].
The pathogenesis is believed to originate from remnants of embryonal cartilage, metaplasia of meningeal fibroblasts, or primitive multipotent mesenchymal cells within the meninges. Hence, this tumor may closely resemble a cartilage-containing meningioma [2, 4].
Although mesenchymal chondrosarcoma was first described in 1959 [5], Dahlin et al [6] first used the word “mesenchymal chondrosarcoma” and reported a first case of intracranial mesenchymal chondrosarcoma in 1962. Bingaman et al reviewed 26 case reports of intracranial extraskeletal mesenchymal chondrosarcomas reported in the English language literature from 1962 to 1999 [7]. According to their analysis, these tumors exhibit a slight predominance in females (11 men and 15 women) and have a peak incidence in the second and third decades of life (mean age 22.5 years). The most frequently affected site is the dura, typically supratentorial, located most often in the frontoparietal region.
CT or MRI scans are very important tools for making decisions regarding therapeutic strategy. Intracranial mesenchymal chondrosarcomas appear on CT as heterogeneous soft tissue densities with patch calcification shadows. On MRI, these tumors appear as a well-defined lobulated soft tissue mass with heterogeneous hypointensities on T1WI, and non-uniform hyperintensities on T2WI and FLAIR. On contrast-enhanced MRI, intracranial mesenchymal chondrosarcomas display significant enhancement indicative of their abundant blood supply. These types of tumors also exhibit growth characteristics of dura attachment, quite similar to imaging findings of meningioma [8]. Therefore, intracranial mesenchymal chondrosarcomas may be misdiagnosed radiologically when they arise in the cerebral falx, tentorium, or convexity.
Histologically, intracranial mesenchymal chondrosarcomas exhibit a biphasic pattern of small undifferentiated cells and scattered islands of well differentiated cartilage. In areas of undifferentiated tissue, this type of tumor often mimics other tumors, including hemangiopericytomas and cartilage-containing meningiomas. This feature can render histological diagnosis difficult, especially when the biopsy specimen is small and the areas of hyaline cartilage are not visualized. On immunohistochemical examination, the undifferentiated mesenchymal cells are positive for vimentin staining, but negative for glial fibrillary acidic protein and neuron-specific enolase staining, which allows for identification and differentiation from meningiomas and hemangiopericytomas [8].
Radical surgical resection is considered the optimal treatment for intracranial mesenchymal chondrosarcoma because it offers the greatest opportunity for a long-term and recurrence-free period for patients, although long-term outcomes may be disappointing. Clear resection margins predict less frequent local recurrence.
There is, however, no consensus as to whether additional radiation and/or chemotherapy are indicated. In a large retrospective study conducted across several medical institutes, Frezza et al [9] showed that complete resection and adjuvant therapy were very important as standard of care for localized disease. Bloch et al [3] also found that 5-year mortality among patients treated by surgery alone was 25% compared to 9% among those treated with surgery and radiotherapy (P < 0.0001). Thus, radiotherapy and chemotherapy may be considered to reduce the risk of recurrence, or to treat patients with unresectable tumors and for those in whom the surgical margins are inadequate after radical surgery. However, the benefits of radiotherapy and chemotherapy are unclear and further investigation is necessary.
Although there is no complete data on the prognosis of intracranial mesenchymal chondrosarcoma, it is considered relatively poor because of the high frequencies of early recurrence and propensity for remote metastasis. On the other hand, the reported survival rates at 5 and 10 years are 54.6% and 27.3%, respectively, which include both skeletal and extraskeletal type of mesenchymal chondrosarcomas [10]. By a systemic review of 560 patients, Bloch et al [3] pointed out that mortality at 5 years was significant greater for patients with tumors of high grade, or of the mesenchymal subtype, or who had received surgical resection alone. Metastatic diseases at diagnosis have also the strongest impact on survival. The median OS was 3 years in patient with metastases at presentation [9]. On the other hand, metastases have been reported to occur in fewer than 20% of patients (range of occurrence of metastasis, 10 months to 8 years), mostly to the bone and lung [7]. In the case of the author, no metastasis was observed at the time of diagnosis.
Conclusions
Here, we present a case of intracranial mesenchymal chondrosarcoma, which is a rare and high-grade malignant tumor with a high rate of recurrence and can form distant metastases. Radical excision of this type of tumor is very important for obtaining a good prognosis. Chemotherapy and radiotherapy may also be considered; however, in the present study, excellent results were obtained following only a complete excision of the tumor without adjuvant therapy. This outcome was attributed to the tumor having clear margins from surround tissue, absence of tumor adhesion, no metastasis at presentation and lower grade at pathological finding. Indeed, no recurrence has been observed in this patient over 5 years after surgery. However, long-term follow-up is indicated for evaluating the prognosis of this type of tumor with surgery alone.
Disclosure
The report complies with the current laws of our country, and informed consent was obtained from the patient who participated.
| References | ▴Top |
- Kan Z, Li H, Zhang J, You C. Intracranial mesenchymal chondrosarcoma: case report and literature review. Br J Neurosurg. 2012;26(6):912-914.
doi pubmed - Safaee M, Clark AJ, Tihan T, Parsa AT, Bloch O. Falcine and parasagittal chondrosarcomas. J Clin Neurosci. 2013;20(9):1232-1236.
doi pubmed - Bloch OG, Jian BJ, Yang I, Han SJ, Aranda D, Ahn BJ, Parsa AT. A systematic review of intracranial chondrosarcoma and survival. J Clin Neurosci. 2009;16(12):1547-1551.
doi pubmed - Sadashiva N, Sharma A, Shukla D, Rajalakshmi P, Mahadevan A, Devi BI. Intracranial extraskeletal mesenchymal chondrosarcoma. World Neurosurg. 2016;95:618 e611-618 e616.
- Lightenstein L, Bernstein D. Unusual benign and malignant chondroid tumors of bone. A survey of some mesenchymal cartilage tumors and malignant chondroblastic tumors, including a few multicentric ones, as well as many atypical benign chondroblastomas and chondromyxoid fibromas. Cancer. 1959;12:1142-1157.
doi - Dahlin DC, Henderson ED. Mesenchymal chondrosarcoma. Further observations on a new entity. Cancer. 1962;15:410-417.
doi - Bingaman KD, Alleyne CH, Jr., Olson JJ. Intracranial extraskeletal mesenchymal chondrosarcoma: case report. Neurosurgery. 2000;46(1):207-211; discussion 211-202.
- Xiao A, Li Z, He X, You C. A rare tentorial mesenchymal chondrosarcoma in posterior cranial fossa: case report. Neurol Neurochir Pol. 2014;48(4):287-291.
doi - Frezza AM, Cesari M, Baumhoer D, Biau D, Bielack S, Campanacci DA, Casanova J, et al. Mesenchymal chondrosarcoma: prognostic factors and outcome in 113 patients. A European Musculoskeletal Oncology Society study. Eur J Cancer. 2015;51(3):374-381.
doi pubmed - Nakashima Y, Unni KK, Shives TC, Swee RG, Dahlin DC. Mesenchymal chondrosarcoma of bone and soft tissue. A review of 111 cases. Cancer. 1986;57(12):2444-2453.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


