| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 2, Number 6, December 2011, pages 265-267
Endoscopic Polypectomy Using Double-balloon Enteroscopy is Useful for the Treatment of Peutz-Jeghers Syndrome Even in Children
Tatsuya Mikamia, Yoshihiro Sasakib, Tadashi Shimoyamaa, d, Manabu Sawayaa, Norihiro Hanabataa, Hiroshi Kijimac, Shinsaku Fukudaa
aDepartment of Gastroenterology, Hirosaki University Graduate School of Medicine, Hirosaki, Japan
bDepartment of Medical Informatics, Hirosaki University Hospital, Hirosaki, Japan
cDepartment of Pathology and Bioscience, Hirosaki University Graduate School of Medicine, Hirosaki, Japan
dCorresponding author: Tadashi Shimoyama, Department of Gastroenterology, Hirosaki University Graduate School of Medicine, 5 Zaifu-cho, Hirosaki, 036-8562 Aomori, Japan
Manuscript accepted for publication September 5, 2011
Short title: Double-balloon Enteroscopy and Peutz-Jeghers Syndrome
doi: https://doi.org/10.4021/jmc309w
| Abstract | ▴Top |
Patients suffering Peutz-Jeghers syndrome (PJS) have had to undergo frequent laparotomies because of intestinal obstruction by small intestinal hamartomatous polyps. Double-balloon enteroscopy (DBE) is now a useful device for the treatment of small intestinal polyps in adults. Here we report a successful use of DBE in the case of small intestinal polypectomy performed on an 11-year-old child with PJS, and do not expect her to have to undergo laparotomies.
Keywords: Peutz-Jeghers syndrome; Double balloon enteroscopy; Polypectomy
| Introduction | ▴Top |
Peutz-Jeghers syndrome (PJS) is an autosomal dominant inherited disease, characterized by multiple gastointestinal (GI) hamartomatous polyps and mucocutaneous pigmentation [1, 2]. To date, patients suffering from this condition have had to undergo frequent laparotomies because of intestinal obstruction by small intestinal polyps. Double-balloon enteroscopy (DBE) is now a useful device for the diagnosis and treatment of small intestinal diseases [3]. Some studies have demonstrated successful endoscopic treatment of small intestinal polyps in adults with PJS [4-7]. We now report a successful use of DBE in the case of small intestinal polypectomy performed on an 11-year-old female child with PJS, and do not expect her to have to undergo unnecessary laparotomies in the future.
| Case Report | ▴Top |
An 11-year-old female child visited our hospital because of iron-deficient anemia (Hb 8.4 g/dL, MCV 60.8 fl) and frequent abdominal pain after meals. Her grandfather and mother had previously been diagnosed as PJS and have received laparotomies previously for intussusception of small intestinal polyps. Recently, her mother underwent small intestinal polypectomy using DBE in our hospital. The child, however, had no past history although she had pigmentation on her lips and toes, suggesting PJS (Fig. 1).
 Click for large image | Figure 1. Pigmentation on the lips and the oral mucosa. |
Initially, we performed endoscopic polypectomy for colorectal polyps, using intravenous analgesics (pentazocine 15 mg and hydroxyzine 25 mg). Three polyps were resected, the largest being 2 cm in size. The pathology was compatible with PJ-type polyps. Two weeks later, the patient underwent oral DBE after obtaining informed consent. We performed DBE carefully in the same manner as we would for an adult, except under general anesthesia. Many polyps were found in the jejunum, the largest 3 cm in size (Fig. 2). Almost all the polyps were pedunculated, and 10 polyps were removed. In view of the low rates of carcinomatous change of PJ-type polyps [8], we retrieved only 2 large polyps in order to obtain pathological samples. The pathology revealed that these polyps were compatible with the PJ-type polyps, and had no adenomatous or carcinomatous components (Fig. 3). Although small polyps remained in the ileum, patient’s family did not want removal at that time. She was well after the polypectomy and discharged 6 days later.
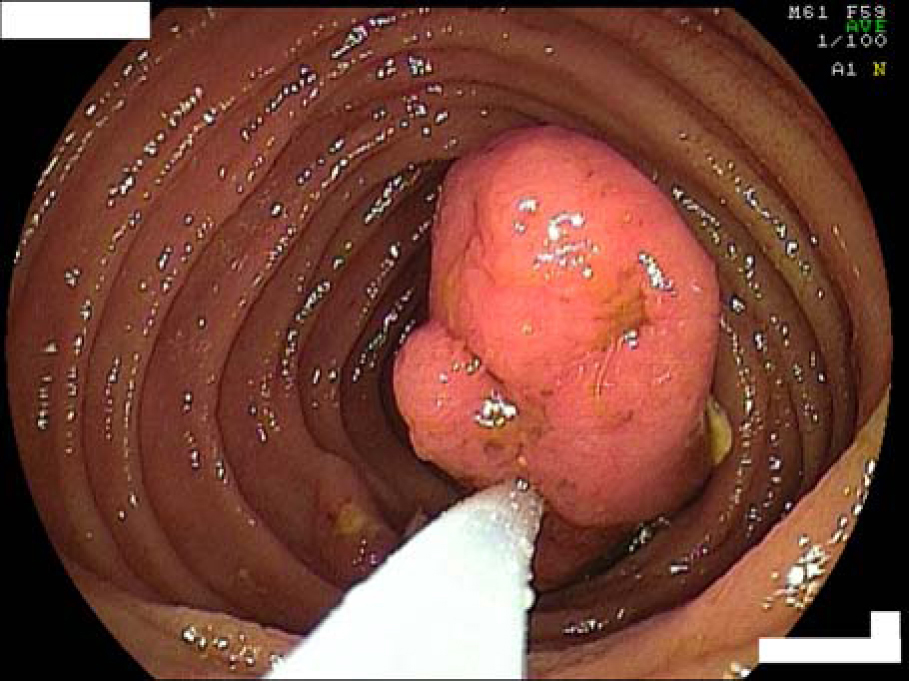 Click for large image | Figure 2. Removal of the polyp in the jejunum using DBE. |
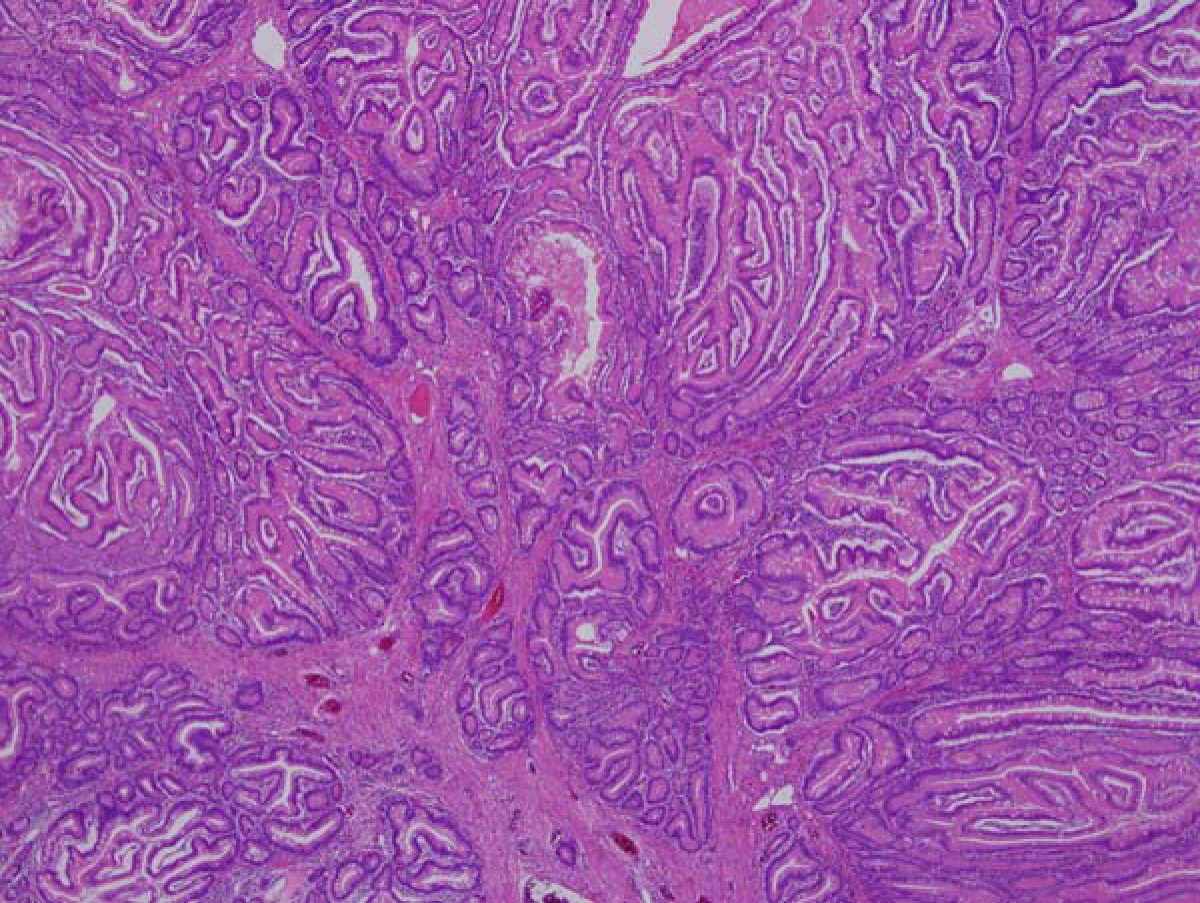 Click for large image | Figure 3. Pathology of the resected polyp. The polyp was compatible with the PJ-type and no adenomatous or carcinomatous components were found. |
| Discussion | ▴Top |
One of the characteristic features of PJS is many GI polyps, particurally in the jejunum and the ileum [1, 2]. Since there were no therapeutic strategies for PJS except surgery prior to the advent of DBE, frequent laparotomies were needed. Pathologically, PJ-type polyps are mostly hamartomatous, and those less than 3 cm in size have a low risk of carcinomatous changes [8]. If the polyps are resected without laparotomies, patients appear to have no need of surgery.
DBE is now available for the diagnosis and treatment of small intestinal diseases [3]. Some studies have revealed that DBE is useful to PJS, but primarily for adults [4-7]. However, it is sometimes necessary for children to undergo surgery. To date, only several children have underwent polypectomy using DBE [9]. In an infant, perforation was reported due to adhesion after polypectomy. PJS in children is associated with a high recurrence rate of small intestinal polyps in short-term follow-ups [10]. In our patient, 2 years after the first polypectomy mentioned above, we performed polypectomy safely from the anus with DBE. She appeared to have no abdominal adhesion. Our patient is approximately 140 cm in height and 47 kg in weight, which are within the mean ± 2 SD of Japanese children of the same age. In cases in which adhesion occurs following laparotomies, we often experience difficulty in inserting the scope into the small intestine. In such conditions, it is preferable to perform DBE in patients with PJS prior to surgery. The present case reveals that repeated polypectomy with DBE is safe and useful for PJS, even in children.
By perfoming repeated polypectomy with DBE, we expect that in the future there will no longer be a need for unnecessary laparotomies in case of PJS.
| References | ▴Top |
- Peutz JLA. Very remarkable case of familial polyposis of mucous membrane of intestinal tract and nasopharynx accompanied by peculiar pigmentation of skin and mucous membrane. Ned Maandschr Geneeskd 1921;10:134-46.
- Jeghers H, Mc KV, Katz KH. Generalized intestinal polyposis and melanin spots of the oral mucosa, lips and digits; a syndrome of diagnostic significance. N Engl J Med. 1949;241(26):1031-1036.
pubmed doi - Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53(2):216-220.
pubmed doi - Ohmiya N, Taguchi A, Shirai K, Mabuchi N, Arakawa D, Kanazawa H, Ozeki M, et al. Endoscopic resection of Peutz-Jeghers polyps throughout the small intestine at double-balloon enteroscopy without laparotomy.Gastrointest Endosc. 2005;61(1):140-147.
pubmed doi - Terauchi S, Snowberger N, Demarco D. Double-balloon endoscopy and Peutz-Jeghers syndrome: a new look at an old disease. Proc (Bayl Univ Med Cent). 2006;19(4):335-337.
pubmed - Gao H, van Lier MG, Poley JW, Kuipers EJ, van Leerdam ME, Mensink PB. Endoscopic therapy of small-bowel polyps by double-balloon enteroscopy in patients with Peutz-Jeghers syndrome. Gastrointest Endosc. 2010;71(4):768-773.
pubmed doi - Ullerich H, Maaser C, Domschke W, Kucharzik T. Small intestinal obstruction by a Peutz-Jeghers polyp—double-balloon enteroscopic removal. Endoscopy. 2007;39 Suppl 1:E193.
pubmed - Beggs AD, Latchford AR, Vasen HF, Moslein G, Alonso A, Aretz S, Bertario L, et al. Peutz-Jeghers syndrome: a systematic review and recommendations for management. Gut. 2010;59(7):975-986.
pubmed doi - Spahn TW, Kampmann W, Eilers M, Mueller MK, Rodeck B. Small-bowel perforation after endoscopic resection of a Peutz-Jeghers polyp in an infant using double-balloon enteroscopy. Endoscopy. 2007;39 Suppl 1:E217.
pubmed - Taguchi T, Suita S, Taguchi S, Tanaka S. Peutz-Jeghers syndrome in children: high recurrence rate in short-term follow-up. Asian J Surg. 2003;26(4):221-224.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


