| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 10, Number 1, January 2019, pages 18-20
Takayasu Arteritis in Chronic Migraine
Miguel Angel Medina Pabon
Cancer Institute of the Americas Diagonal 75B No. 2A-80/140 Medellin, Antioquia, Colombia
Manuscript submitted December 22, 2018, accepted December 27, 2018
Short title: Takayasu Arteritis in Chronic Migraine
doi: https://doi.org/10.14740/jmc3238
| Abstract | ▴Top |
Takayasu arteritis (TA) is a systemic granulomatous vasculitis of large vessels with low incidence and nonspecific symptoms, and late diagnosis and management lead to complications such as stroke, acute myocardial infarction or peripheral ischemia. This case illustrates the complexity of TA diagnosis because its symptomatology is frequently mistaken as chronic migraine. Therefore, without a syndromic approach, it is more likely to increase comorbidity and progression of the disease. This paper deacribes a 25-year-old woman with chronic migraine for 8 years, with recurrent admissions to emergency service, and specialist outpatient consultations. The patient has a history of fugax amaurosis, hypertension and claudicating chest pain that required treatment with corticoid, hydroxychloroquine, methotrexate and neflunomide, due to a stenosis of 50-70% of the left carotid artery and thickening of the walls of the distal thoracic aorta and the proximal abdominal aorta, corresponding to TA, with improvement of its subsequent symptomatology to treatment for rheumatology.
Keywords: Chronic migraine; Headache; Fleeting amaurosis; Hypertension; Takayasu arteritis
| Introduction | ▴Top |
Takayasu arteritis (TA) is a granulomatous, idiopathic, inflammatory disease of large vessels, which predominates in women of fertile age, and it affects the aorta, most often its arteries of the main branch carotid and subclavian arteries [1, 2]. It is formerly referred to as an aortic arch syndrome, pulseless disease, idiopathic aortitis, stenosing aortitis, aortoarteritis, and occlusive thrombotic arteriopathy. TA incidence has been estimated to be 2/1,000,000 per year [3]. It is more prevalent in Central and South America, Africa, India, and the Far East [4]. In a recent study, the mortality rate of TA was estimated to be 2.5 × 100,000 inhabitants due to the association of this arteritis with premature deaths [5, 6].
Chronic migraine is a relatively recent disease, defined as a pulsatile headache, of moderate to severe intensity, associated with nausea, vomiting, and disability to perform daily activities, in a period of 15 days for more than 3 months [7]. In addition, the excessive use of analgesic in this population can be confused as a chronic headache.
Here, a case of TA that had chronic migraine criteria without improvement with medications is described. However, the presence of nonspecific signs and symptoms confused physicians, delaying the diagnosis and management of TA. This case reflects the complexity of its diagnosis and the ability of the clinician to analyse the clinical history, through the collection of symptoms in a syndrome. The most important results are the remission and prevention of the consequences related to the disease. Although these goals are achieved in the majority of patients receiving modern therapies, prevention related to late diagnosis and adverse effects of glucocorticoids remain to be a headache for these patients [8].
| Case Report | ▴Top |
The 25-year-old Colombian Caucasian woman is an odontology student, with a history of cholecystectomy for cholelithiasis 2 years ago, and hypertension associated with pregnancy 3 years ago. Before her admission to the headache program at the Regional Clinic of the Aburra Valley National Police, Envigado, Antioquia, Colombia, she presented amaurosis in the left eye for a week 5 years ago. The patient does not smoke or consume alcohol, she has a child through vaginal delivery, and had an abortion (G2P1A1C0V1). She takes oral contraceptives, nifedipine 30 mg daily, hydrochlorothiazide 25 mg daily, propranolol 40 mg every 12 h, paracetamol, and naproxen, depending on pain.
There were multiple queries of the patient due to an intense headache, with a history of pulsatile hemicranial headache, associated with nausea, dizziness, photophobia, and sonophobia, of severe intensity, with more than eight episodes per month in the last 3 months. Additionally, the abuse of analgesics when taking acetaminophen with codeine, naproxen more than 15 doses per month, and patient assessment by emergency, outpatient and specialist services, she was referred to the headache program at the same clinic.
The patient also reported episodes of fatigue, intermittent muscle fatigue, paresthesias in the hands and feet that was improved when lying on the right side, in addition to intermittent chest pain of severe intensity of short duration, mainly in the supine position, one episode per month. This was associated with episodes of a severe headache since 7 years ago.
Physical assessment showed that she had an adequate general condition, divergent blood pressure in both arms (TA: 150/100 in the left arm, TA: 100/65 in the right arm) with left radial pulse parvus tardus, a left carotid murmur, and no heart murmurs. Retinal inspection was not evaluated, no focalization signs were found, and rest of exploration showed no findings of interest.
Diagnostic test results are shown as follows. Carotid Doppler ultrasound shows stenosis of approximately 50-70% of the left common carotid artery. Bilateral, permeable vertebral circulation was found. Subsequently, a contrast tomography of the head and neck was performed without evidence of lesions, after 3 months of treatment with rheumatology, indicating her clinical improvement. An angioresonance was also ordered with neck and chest contrast, finding a decrease in the caliber of the left common carotid before the bifurcation and another decrease in the origin of the right brachiocephalic trunk and a thickening of the walls of the distal thoracic aorta and the proximal abdominal aorta, that could correspond to TA, confirming its diagnostic image (Fig. 1).
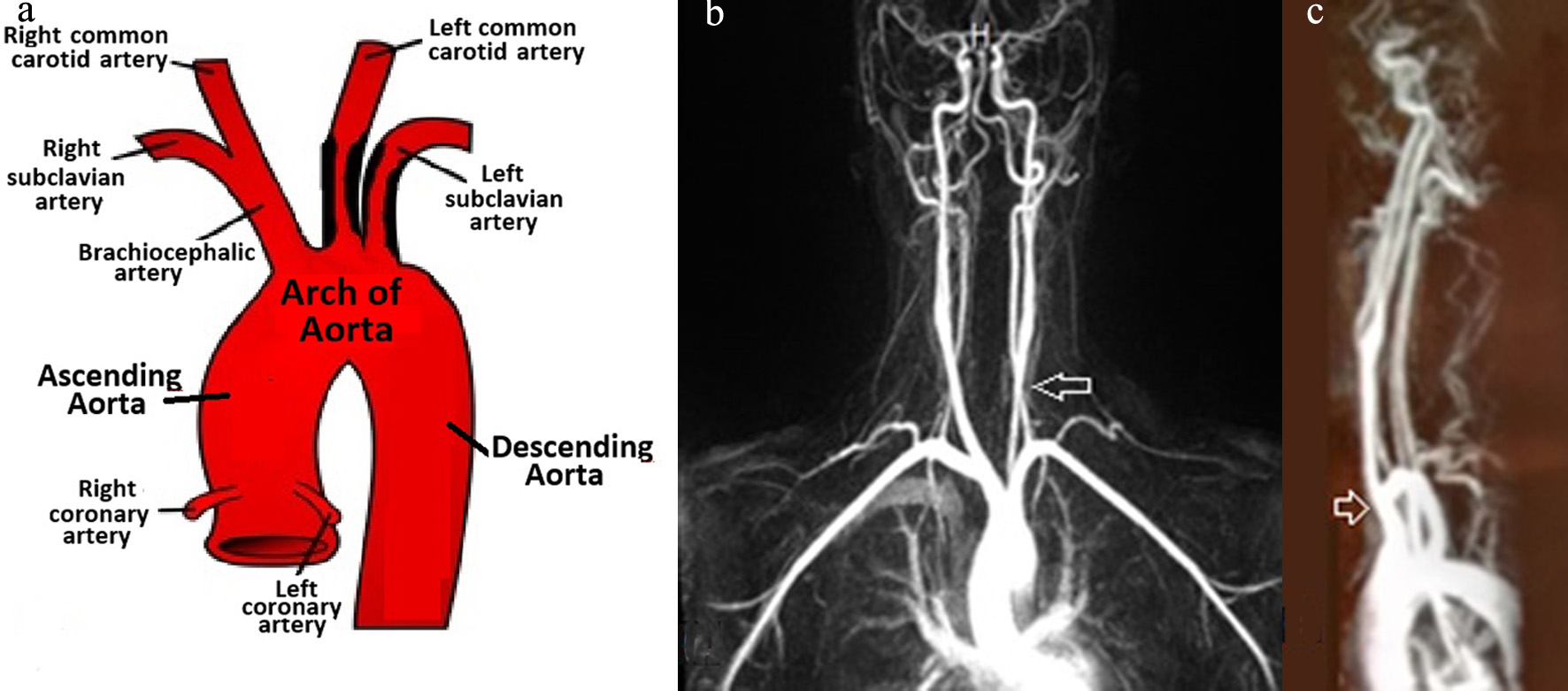 Click for large image | Figure 1. (a) Carotid Doppler ultrasound shows stenosis of approximately 50-70% of the left common carotid artery. Bilateral, permeable vertebral circulation is shown. (b) Angioresonance with contrast in the neck is shown, and the arrow indicates a decrease in the caliber of the left common carotid before the bifurcation and the left subclavian artery. (c) Angioresonance with contrast in the neck with a side view is shown, and the arrow indicates caliber thickening of the origin in the right brachiocephalic trunk that could correspond to TA. |
| Discussion | ▴Top |
The pathophysiology of TA starts with inflammation, and endothelial damage usually leads to thickening of the wall, thrombus formation, stenotic and occlusive lesions, while the destruction of the muscular and elastic layers originates - dilation and aneurysms. These lesions often result in organic-cellular dysfunction secondary to ischemia [6, 8].
The clinical manifestations of TA are different according to the temporary point along the course of the disease. During the first active inflammatory phase, systemic symptoms are usually nonspecific, predominating for weeks or months, but are often overlooked, making people confuse it with acute illnesses. During this stage, the course of the disease may follow a form of sending-relapsing, which makes diagnosis and early management difficult [9, 10]. The recurrent disease often occurs in new arterial territories, with the consequent coexistence of active and inactive lesions (sequelae). The late chronic phase (the “pulseless” stage) is characterized by ischemia and symptoms secondary to arterial occlusion.
In this case, the patient consulted at the beginning of the recurrent phase, due to intermittent pain in the thorax, hands, and feet, muscle fatigue and intense headaches that confuse the diagnosis. However, a prominent symptom to suspect TA was amaurosis in the left eye that lasted a week due to intermittent ischemic processes, which led the physician to perform an exhaustive physical examination finding radial pulse tardus parvus and left carotid murmur proper in the chronic phase of the disease.
Almost 20% of patients with TA show neurological compromise. The most common neurological symptoms are severe headaches, organic confusion, cognitive dysfunction, prolonged amaurosis, stroke, meningitis, middle cerebral artery aneurysm, reversible encephalopathy, and seizures (unrelated to hypertension) [11].
Moreover, hypertension constituted an essential symptom to suspect TA, which is present in over 80% of the cases. In young patients it needs to rule out secondary causes, the most usual being renovascular hypertension, which may be asymptomatic in about 50% of patients [12]. Additionally, the surgical history of cholecystectomy due to cholelithiasis might be due to ischemic processes that generated bilirubin stones, since this pathology is present in elderly patients.
In conclusion, chronic migraine is an unusual manifestation of TA. However, it can delay the management of the underlying disease by treating the individual symptoms separately. Therefore, a syndromic approach from the beginning establishes an early diagnosis, which is essential for a better prognosis, since TA is associated with high morbidity and mortality. This patient required aggressive immunosuppressive therapy with satisfactory clinical evolution, without a headache or complications.
Conflict of Interest
I have no conflict of interest to declare.
Grant Support
None.
| References | ▴Top |
- Yang PP, Yang YH, Kuang TG, Yang MF, Wang JF, Huang Q, Yang SQ, et al. [Pulmonary cavities with Takayasu arteritis: report of 3 cases and literature review]. Zhonghua Jie He He Hu Xi Za Zhi. 2018;41(10):787-792.
pubmed - Espinoza JL, Ai S, Matsumura I. new insights on the pathogenesis of Takayasu arteritis: revisiting the microbial theory. Pathogens. 2018;7(3):73.
doi pubmed - Reinhold-Keller E, Herlyn K, Wagner-Bastmeyer R, Gross WL. Stable incidence of primary systemic vasculitides over five years: results from the German vasculitis register. Arthritis Rheum. 2005;53(1):93-99.
doi pubmed - Watts R, Al-Taiar A, Mooney J, Scott D, Macgregor A. The epidemiology of Takayasu arteritis in the UK. Rheumatology (Oxford). 2009;48(8):1008-1011.
doi pubmed - Garen T, Lerang K, Hoffmann-Vold AM, Andersson H, Midtvedt O, Brunborg C, Kilian K, et al. Mortality and causes of death across the systemic connective tissue diseases and the primary systemic vasculitides. Rheumatology (Oxford). 2018.
- de Graeff N, Groot N, Brogan P, Ozen S, Avcin T, Bader-Meunier B, Dolezalova P, et al. European consensus-based recommendations for the diagnosis and treatment of rare paediatric vasculitides - the SHARE initiative. Rheumatology (Oxford). 2018.
- Medrea I, Christi S. Chronic Migraine - Evolution of the Concept and Clinical Implications. Headache. 2018;58(9):1495-1500.
doi pubmed - Berti A, Dejaco C. Update on the epidemiology, risk factors, and outcomes of systemic vasculitides. Best Pract Res Clin Rheumatol. 2018;32(2):271-294.
doi pubmed - Goel R, Kumar TS, Danda D, Joseph G, Jeyaseelan V, Surin AK, Bacon P. Childhood-onset Takayasu arteritis - experience from a tertiary care center in South India. J Rheumatol. 2014;41(6):1183-1189.
doi pubmed - Eleftheriou D, Varnier G, Dolezalova P, McMahon AM, Al-Obaidi M, Brogan PA. Takayasu arteritis in childhood: retrospective experience from a tertiary referral centre in the United Kingdom. Arthritis Res Ther. 2015;17:36.
doi pubmed - Benjaminsen E, Reigstad A, Cengija V, Lilleby V, Carlsson M. Stroke as the Sole Manifestation of Takayasu Arteritis in a 15-Year-Old Boy with Latent Tuberculosis. Case Rep Neurol Med. 2016;2016:8736248.
doi - Brunner J, Feldman BM, Tyrrell PN, Kuemmerle-Deschner JB, Zimmerhackl LB, Gassner I, Benseler SM. Takayasu arteritis in children and adolescents. Rheumatology (Oxford). 2010;49(10):1806-1814.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


