| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 10, Number 2, February 2019, pages 49-52
A Rare Case of Pericarditis due to Listeria monocytogenes 1/2a and 4b Serotypes
Isabel Dominguesa, d, Pedro Arosob, Mariana Goncalvesc, Edgar Pratasa, Joao Carvalhoa, Sara Pinheiroa, Filipe Bredac, Lelita Santosc
aDepartment of Medical Oncology, Portuguese Institute of Oncology of Coimbra Francisco Gentil (IPOCFG), Coimbra, Portugal
bDepartment of Physical Rehabilitation, Coimbra Hospital and University Centre (CHUC), Coimbra, Portugal
cDepartment of Internal Medicine, Coimbra Hospital and University Centre (CHUC), Coimbra, Portugal
dCorresponding Author: Isabel Domingues, Department of Medical Oncology, Portuguese Institute of Oncology of Coimbra Francisco Gentil (IPOCFG), Avenida Bissaya Barreto 98, 3000-075 Coimbra, Portugal
Manuscript submitted January 1, 2019, accepted January 14, 2019
Short title: Pericarditis due to Listeria monocytogenes
doi: https://doi.org/10.14740/jmc3244
| Abstract | ▴Top |
Listeriosis is associated with the consumption of contaminated food and has a higher incidence in the elderly, immunocompromised and pregnant. There are a few reported cases of pericarditis due to Listeria monocytogenes, with a high mortality. We present a successful case of Listeria monocytogenes pericarditis in a 61-year-old patient and provide the clinical presentation, pathology and diagnostic challenge. Increasing awareness of foodborne infections would be important to promote its early diagnosis.
Keywords: Listeria monocytogenes; Pericarditis; Listeriosis; Foodborne infections
| Introduction | ▴Top |
Listeria monocytogenes is a ubiquitous gram-positive bacillus, and a facultative intracellular and fastidious pathogen, which is able to proliferate in adverse conditions. Consumption of contaminated food, mostly raw products (milk, meat, fish, flour, and fresh cheese) [1-3], is the major cause of listeriosis. It has a higher incidence and severity in the elderly, immunocompromised people (with lymphoma, human immunodeficiency virus (HIV) infection), pregnant women and newborns [2]. Listeriosis is associated with high a morbidity and mortality. The most common presentations are bacteremia, meningitis and meningoencephalitis. Pericarditis due to Listeria monocytogenes is an extremely rare disease; therefore, knowledge of its pathogenesis, diagnosis and treatment is limited [4]. We present a patient with pericarditis caused by Listeria monocytogenes, persistent and difficult to diagnose and manage. We show the importance of differential diagnosis and the importance of foodborne infections.
| Case Report | ▴Top |
We present a 61-year-old man with 1-month history of mild fever, dyspnea and thoracic pain.
During this disease evolution, he had several visits to urgency department and received two antibiotic courses, aiming at an upper respiratory infection. He was medicated firstly with amoxicillin/clavulanate plus azithromycin, with clinical remission. He also presented with an atrial fibrillation (AF) of recent onset. Anticoagulation was started and cardiac rhythm was controlled. After 3 weeks he had recurrence of mild fever and mild cough, and he received doxycycline, without remission of fever. He had no other cardiac events and chest X-ray did not show pulmonary findings.
After 1 month of fever history the patient had a third admission to urgency department, presenting with high fever. Additionally, he presented with respiratory deterioration, with shortness of breath, dry cough and left thoracic pleuritic pain. He never had gastrointestinal symptoms. He had a past medical history of Ann Arbor stage IV Hodgkin lymphoma, in remission for 34 years. He was submitted to chemotherapy with mechlorethamine, vincristine, procarbazine and prednisone (MOPP) protocol, followed by splenectomy. He also reported a recent trip to Portugal north coast, where he had consumed a large quantity of fresh fish.
On physical examination, the patient presented with subfebrile temperature and mild hypotension, but was eupneic (peripheral oxygen saturation of 97%). He had irregular cardiac sounds, bilateral pulmonary rales and mild hepatomegaly. He presented with mild bilateral pitting edema up to the knees. There were no meningeal signs. Laboratory findings were relevant for white blood cell count (12.8 × 109 cells/L; 76% neutrophils), C-reactive protein (16.38 mg/dL), hemoglobin (11.2 g/dL, normocytic), light elevation of cardiac troponin I (2.95 ng/mL), with normal myoglobin and creatine kinase. He had normal iron kinetics. Electrocardiogram showed AF. Chest X-ray revealed a bilateral pleural effusion, cardiomegaly and left diaphragmatic elevation (splenectomy sequelae; Fig. 1). Transthoracic echocardiography showed small pericardial effusion, with no signs of ischemia.
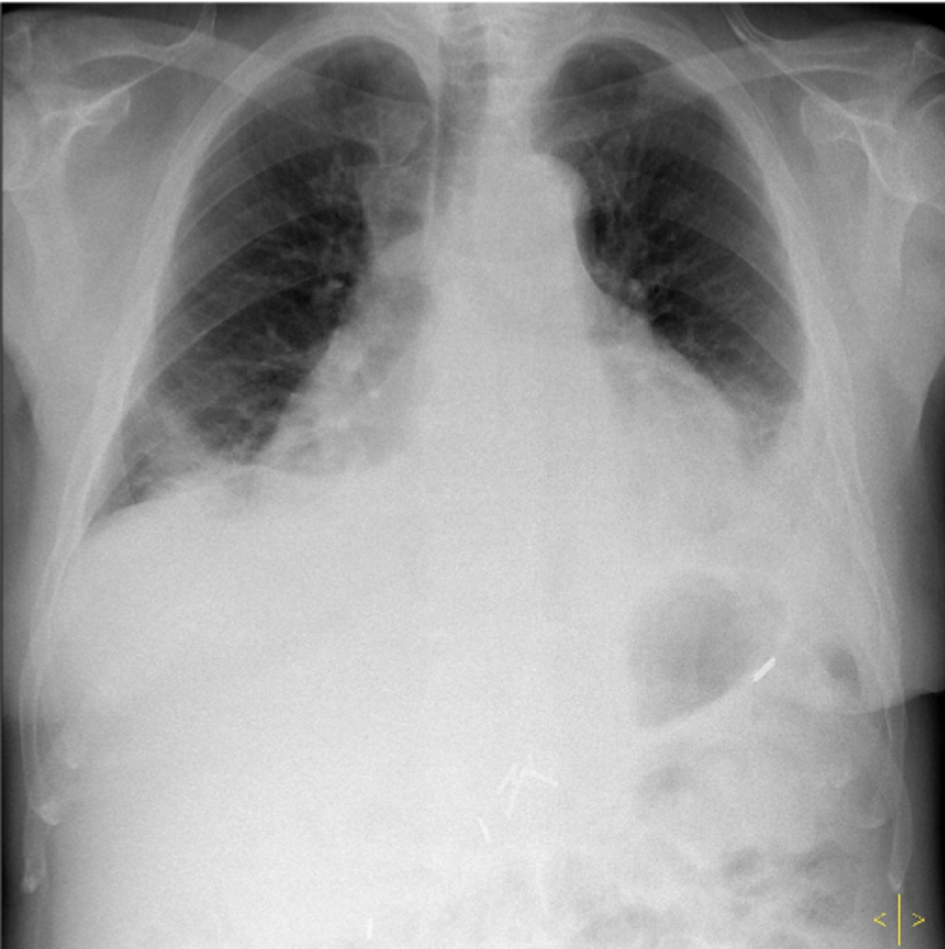 Click for large image | Figure 1. Patient chest X-ray on admission, showing a bilateral pleural effusion and cardiomegaly. |
He was admitted for investigation of fever of unknown origin, and cardiac failure of new onset New York Heart Association (NYHA) grade III. All cultures of blood, urine and respiratory secretions were negative. Mantoux test presented unspecific reaction and the determination of gamma interferon was negative. Viral infections were excluded. He underwent a thoracentesis revealing a pleural transudate, normal adenosine deaminase, reactive mesothelial cells, no tumor cells, and negative microbiology. Abdominal ultrasound did not show significant alterations.
During the clinical investigation, the patient presented with persistent fever, dyspnea, light to mild chest pain, mild hypotension, and increasing inflammatory parameters. He maintained a stable light elevation of troponin I. He received antibiotic therapy with piperacillin/tazobactam, followed by meropenem and vancomycin, analgesics, low dose of diuretics and anticoagulation. Transesophageal echocardiography showed a small volume (< 1 cm) of circumferential pericardial effusion, maintaining a good left ventricular systolic function. There were no signs of ischemia or vegetations, and no signs of hematological disease on blood investigations. He underwent a computerized tomography (CT) scan revealing a diffuse pericardium thickening, few mediastinal reactive lymph nodes, moderate right pleural effusion (Figs. 2, 3), and a mild hepatomegaly.
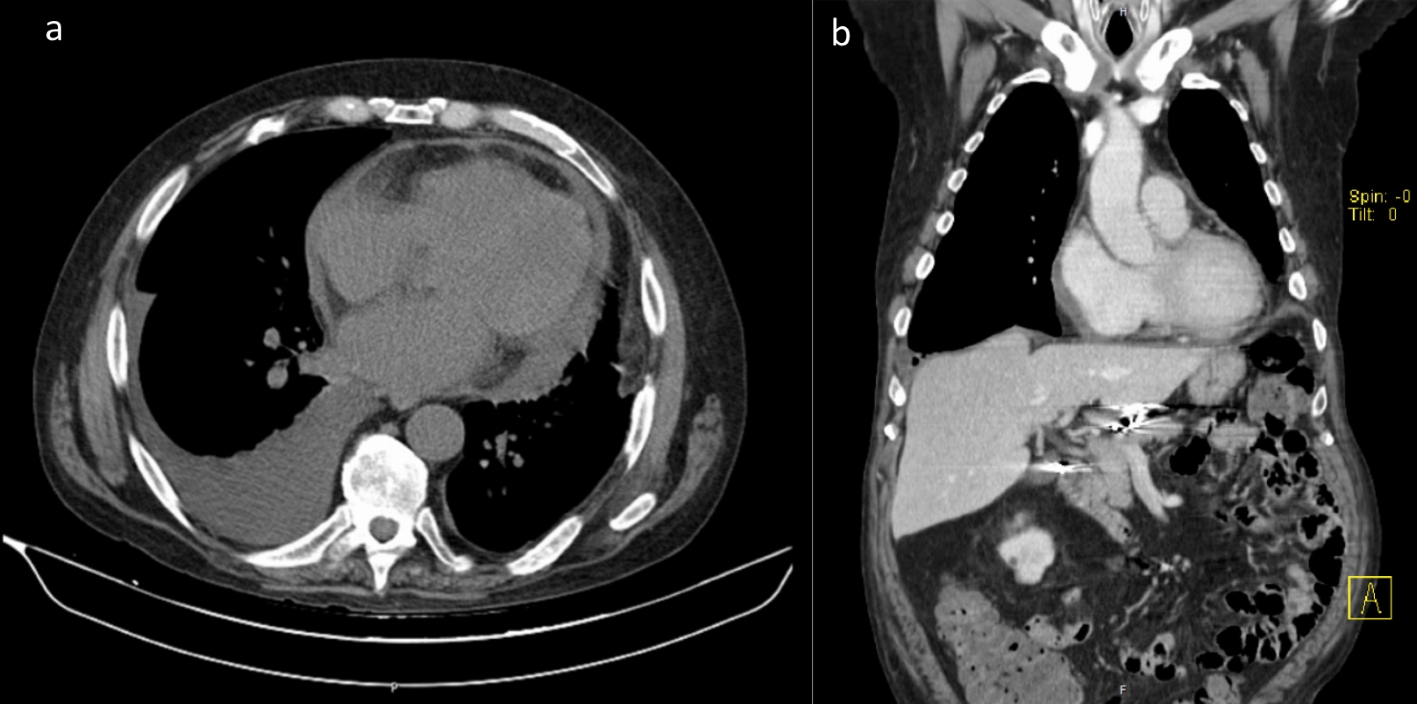 Click for large image | Figure 2. Computerized tomography (CT), diffuse thickening of the pericardium, some mediastinal lymph nodes and moderate right pleural effusion (after left thoracentesis). |
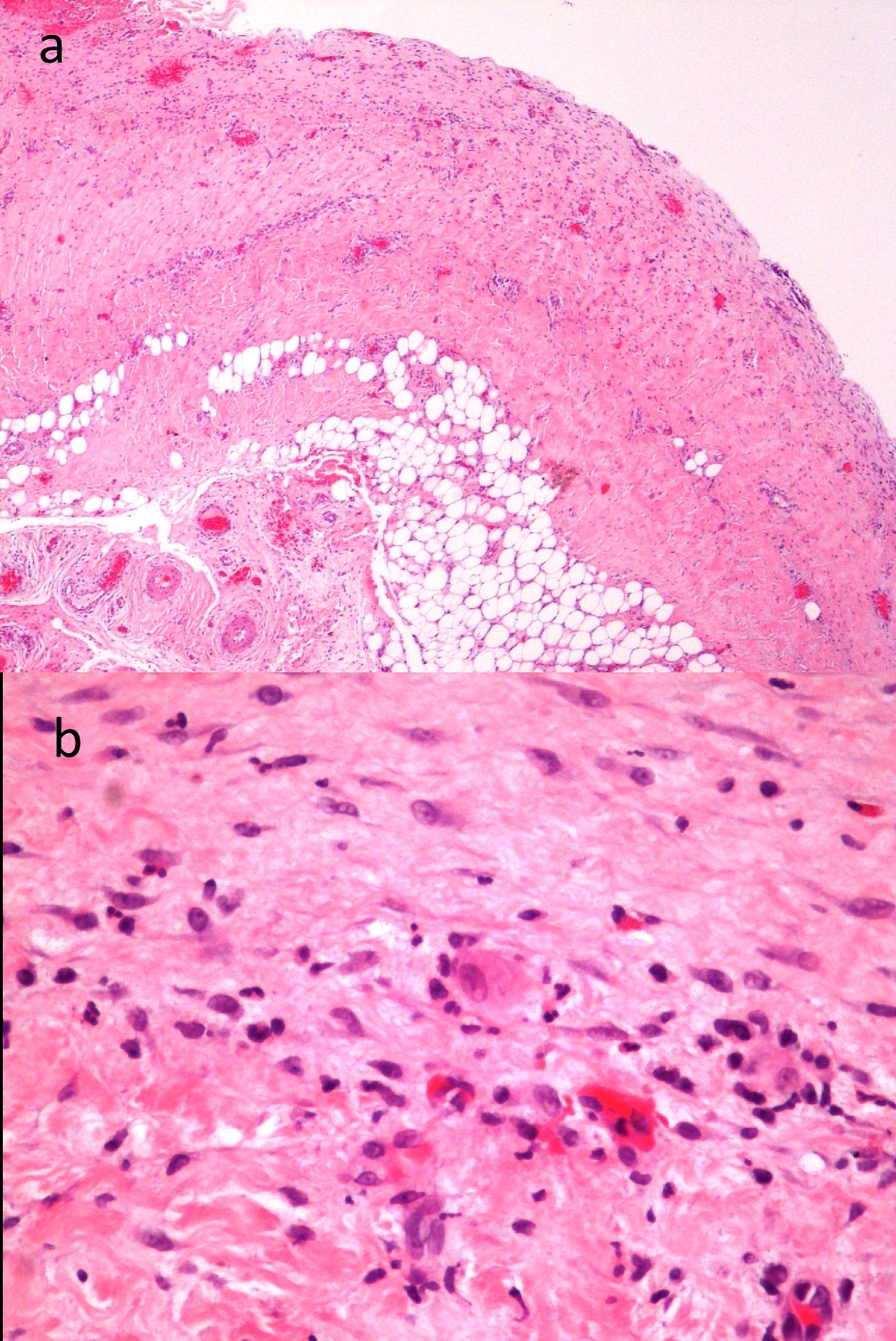 Click for large image | Figure 3. Pericardial biopsy presenting pericardial thickening, acute inflammatory activity, with perivascular inflammatory infiltrate, including some polynucleated neutrophils. (a) 40 ampliation fields, and (b) 400 ampliation fields. |
Finally, the investigation for atypical agents was positive for Listeria monocytogenes infection. We observed elevation of serum levels of serotype 1/2a immunoglobulin G (IgG) and serotype 4b IgG (both quantifications were 800, by indirect immunofluorescence). Biopsy of pericardium showed features of acute inflammatory pericarditis, revealed by perivascular inflammatory infiltrate and pericardium infiltration by neutrophils, probably of bacterial etiology (Figs. 4, 5). It was not possible to analyze microbiologically the sample. Given the high probability of an acute pericarditis due to Listeria monocytogenes, the patient received amoxicillin for 4 weeks.
He presented with fever resolution and progressive clinical recovery, after 12 days of treatment. He was discharged and completed antibiotic at ambulatory. During 1-year follow-up, he remained clinically recovered, presenting with normalization blood tests and resolution of cardiac AF (to sinus rhythm). Pericardium was also normalized on CT scan imaging.
| Discussion | ▴Top |
The incidence of listeriosis is still uncertain worldwide. This is mostly because of under diagnosis, the lack of notification and variable food security policies. In our country, it is not a notifiable infection [5]. Cardiovascular involvement is very rare and potentially fatal. By analyzing the previously reported cases, we find that Listeria monocytogenes pericarditis has a mortality rate of about 60% (fatal in 6/10 cases) [3, 4, 6-11]. This is higher than the reported mortality of purulent pericarditis [12, 13]. In these reported cases, patients were 54 years old or older. They mostly presented with fever, dyspnea, chest pain and peripheral edema. The presence of weak immune system (human immunodeficiency virus (HIV) infection, cirrhosis, neoplasia, corticosteroids and immunosuppressants) and iron overload states (hemochromatosis, hemodialysis) were noticed. Our patient was in the same age group and splenectomized. All the other causes of immunosuppression and iron overload reported on previous case reports were excluded.
Usually, the diagnosis was made by pericarditis and Listeria monocytogenes bacteremia confirmation. The isolation of Listeria monocytogenes in a pericardium culture is the gold standard for diagnosis, but it is often difficult to achieve. Its isolation in cultures is unlikely after the prior antibiotic regimens. On the other hand, we had high serologies for serotypes 1/2a and 4b, strongly suggestive of infection. Additionally, listeria subpopulations with cardiotropic activity have been shown [14, 15].
The patient completely recovered under amoxicillin, supporting this diagnosis. Fatal outcomes in previous reports were seen more commonly in severe infections or even septic shock. In these cases, mostly adopted therapy was a penicillin alone (amoxicillin or ampicillin), or in association with gentamicin, during 4 - 6 weeks. There is one successful report of erythromycin treatment for 4 weeks [3, 4, 6-11].
This case report aims to increase awareness of foodborne infections among health professionals and promote early diagnosis. It is important that there is a careful management of antibiotics, especially when there are not microbiological findings (or an infectious focus suspected) to guide the treatment. Further studies are needed to know more about Listeria monocytogenes subpopulations and improve food security.
Disclaimers
This is an original work, and it was not submitted in any previous abstracts, presentations, reports, or publications.
Disclosures
There are no financial interests or affiliations with institutions, organizations, or companies.
| References | ▴Top |
- Boerlin P, Boerlin-Petzold F, Bannerman E, Bille J, Jemmi T. Typing Listeria monocytogenes isolates from fish products and human listeriosis cases. Appl Environ Microbiol. 1997;63(4):1338-1343.
pubmed - Goulet V, Hedberg C, Le Monnier A, de Valk H. Increasing incidence of listeriosis in France and other European countries. Emerg Infect Dis. 2008;14(5):734-740.
doi pubmed - Manso C, Rivas I, Peraire J, Vidal F, Richart C. Fatal Listeria meningitis, endocarditis and pericarditis in a patient with haemochromatosis. Scand J Infect Dis. 1997;29(3):308-309.
doi pubmed - Khan A, Rosen KM, Rahimtoola SH, Gunnar RM. Listeria bacteremia with acute pericarditis. Chest. 1971;60(5):496-497.
doi pubmed - Almeida GN, Gibbs PA, Hogg TA, Teixeira PC. Listeriosis in Portugal: an existing but under reported infection. BMC Infect Dis. 2006;6:153.
doi pubmed - Carvajal A, Samuelsson S, Rothgardt NP, Frederiksen W. The treatment of Listeria monocytogenes septicaemia. Acta Microbiol Hung. 1989;36(2-3):165-168.
pubmed - Delvallee M, Ettahar N, Loiez C, Decoene C, Courcol R, Wallet F. An unusual case of fatal pericarditis due to Listeria monocytogenes. Jpn J Infect Dis. 2012;65(4):312-314.
doi pubmed - Dias V, Cabral S, Anjo D, Vieira M, Antunes N, Carvalheiras G, Gomes C, et al. Successful management of Listeria monocytogenes pericarditis: case report and review of the literature. Acta Cardiol. 2011;66(4):537-538.
doi pubmed - Ferguson R, Yee S, Finkle H, Rose T, Schneider V, Gee G. Listeria-associated pericarditis in an AIDS patient. J Natl Med Assoc. 1993;85(3):225-228.
pubmed - Holoshitz J, Schneider M, Yaretzky A, Bernheim J, Klajman A. Listeria monocytogenes pericarditis in a chronically hemodialyzed patient. Am J Med Sci. 1984;288(1):34-37.
doi pubmed - Revathi G, Suneja A, Talwar V, Aggarwal N. Fatal pericarditis due to Listeria monocytogenes. Eur J Clin Microbiol Infect Dis. 1995;14(3):254-255.
doi pubmed - LeWinter MM. Clinical practice. Acute pericarditis. N Engl J Med. 2014;371(25):2410-2416.
doi pubmed - Pankuweit S, Ristic AD, Seferovic PM, Maisch B. Bacterial pericarditis: diagnosis and management. Am J Cardiovasc Drugs. 2005;5(2):103-112.
doi pubmed - Liu D. Identification, subtyping and virulence determination of Listeria monocytogenes, an important foodborne pathogen. J Med Microbiol. 2006;55(Pt 6):645-659.
doi pubmed - McMullen PD, Gillaspy AF, Gipson J, Bobo LD, Skiest DJ, Freitag NE. Genome sequence of Listeria monocytogenes 07PF0776, a cardiotropic serovar 4b strain. J Bacteriol. 2012;194(13):3552.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


