| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website http://www.journalmc.org |
Case Report
Volume 10, Number 10, October 2019, pages 312-314
Disseminated Gonococcal Infection: A Case Report of Arthritis-Dermatitis Syndrome
Mariana da Cruza, d, Nuno Zarcos Palmaa, Rita Veiga Ferrazb, Marvin Oliveirac, Ricardo Meirelesa
aInternal Medicine Service, Centro Hospitalar Tamega e Sousa, Penafiel, Portugal
bInfectious Diseases Service, Centro Hospitalar Tamega e Sousa, Penafiel, Portugal
cMicrobiology Service, Centro Hospitalar Tamega e Sousa, Penafiel, Portugal
dCorresponding Author: Mariana da Cruz, Internal Medicine Service, Centro Hospitalar Tamega e Sousa, Penafiel 4560-136, Portugal
Manuscript submitted October 2, 2019, accepted October 21, 2019
Short title: Disseminated Gonococcal Infection
doi: https://doi.org/10.14740/jmc3381
| Abstract | ▴Top |
The bacteremic spread of the sexually transmitted pathogen, Neisseria gonorrhoeae (N. gonorrhoeae), results in disseminated gonococcal infection (DGI), which can lead to a variety of clinical signs and symptoms, such as multiple skin lesions, tenosynovitis and arthralgias/arthritis. The Centers for Disease Control and Prevention listed that drug-resistant N. gonorrhoeae (cephalosporin resistance) poses an urgent threat due to antimicrobial resistance. The authors describe the case of a young woman presenting in the emergency department (ED) with skin lesions and malaise. DGI was confirmed by blood cultures, nucleic acid amplification testing (NAAT) in cervical mucosa and urine gonococcal probe. One week of intravenous ceftriaxone was administrated with complete clinical and analytical resolution. The patient made a full clinical recovery. Clinicians must be aware of the signs and symptoms of this rare yet reemerging disease.
Keywords: Skin lesions; Disseminated gonococcal infection; Neisseria gonorrhoeae; Arthritis-dermatitis syndrome
| Introduction | ▴Top |
Neisseria gonorrhoeae (N. gonorrhoeae) is a sexually transmitted pathogen. The most frequent clinical manifestations of N. gonorrhoeae infection include cervicitis and pelvic inflammatory disease in women and urethritis and epididymitis in men. Extragenital infections are common, and clinical manifestations are dependent on the site of inoculation [1]. Dissemination of gonococci occurs rarely, but can cause specific syndromes, such as arthritis-dermatitis syndrome, characterized by tenosynovitis, arthralgia, and skin lesions [2]. This syndrome is a relatively common manifestation of disseminated gonococcal infection (DGI) and is the presenting feature of 60% adults with DGI [1-3]. Effective treatment is currently available for several sexually transmitted infections (STIs); however, antimicrobial resistance (AMR), particularly in N. gonorrhoeae, has increased rapidly in recent years and has reduced treatment options [4]. In this report, we describe the case of a young woman with tenosynovitis, arthritis and skin lesions as first manifestations of a gonococcal infection.
| Case Report | ▴Top |
A 27-year-old healthy woman with allergic rhinitis presented to the emergency department (ED) reporting a 4-day history of fever, odynophagia/sore throat, painful skin lesions (Fig. 1), muscle aches as well as unilateral wrist, elbow and ankle pain.
 Click for large image | Figure 1. Skin lesions: hemorrhagic pustules with dusky center and peripheral erythema. |
The patient confirmed unprotected oral and vaginal sexual intercourse exclusively with her partner for the past 6 months. Physical examination showed sparse erythematous pustules on the palmar face of the fingers. Following the skin lesions, she developed inflammatory signs on the left ankle with pain in passive and active motion and tenosynovitis involving the left plantar extensors and the right arm flexors. A closer examination of the patient’s hand revealed a necrotic papule with a surrounding rim of erythema at the proximal phalangeal of the third digit. She denied any painful urination, urethral discharge nor genital lesions. She did not report travels abroad.
Systolic/diastolic blood pressure was of 127/72 mm Hg, pulse 82 beats per minute (bpm), respiratory rate 16 cycles per minute (cpm), temperature 39 °C (tympanic) and SpO2 100% (fraction of inspiration O2 (FiO2) 0.21). Urine pregnancy test was negative. Lab results revealed white blood count (WBC) of 12.89 × 103/µL (normal 4.5 - 11 × 103/µL), with 73.6% of neutrophils, and C-reactive protein (CRP) of 69.8 mg/L (normal < 7.5 mg/L) suggesting bacterial infection. Antibody anti-streptolysin O was negative. Human immunodeficiency virus-1 (HIV-1), HIV-2 and hepatitis C virus (HCV) antibodies were negative, and she was immune for hepatitis B virus (HBV).
Ultrasound showed a moderately effusion and surrounding edema of the left ankle. Transthoracic echocardiography and thoracic, abdominal and pelvic tomography were unremarkable. A workup for autoimmune disease including antinuclear antibody, rheumatoid factor and anticyclic citrullinated peptide was negative. Venereal Disease Research Laboratory (VDRL) test was nonreactive. Borrelia, Brucella, Rickettsia, cytomegalovirus (CMV) and Epstein-Barr virus (EBV) acute infections were excluded.
Gram stain of positive blood cultures revealed Gram-negative diplococci (Fig. 2). Less than 24 h later, growth was observed on the chocolate agar plate incubated at 37 °C with 5% CO2 (Fig. 3). Bacterial identification was performed (API® NH system, bioMerieux) and confirmed N. gonorrhoeae, supporting the diagnosis of DGI. Antimicrobial susceptibility testing did not reveal any resistance. N. gonorrhoeae DNA was detected in pharyngeal urogenital and urine samples by nucleic acid amplification testing (NAAT). Chlamydia trachomatis (C. trachomatis) co-infection was excluded.
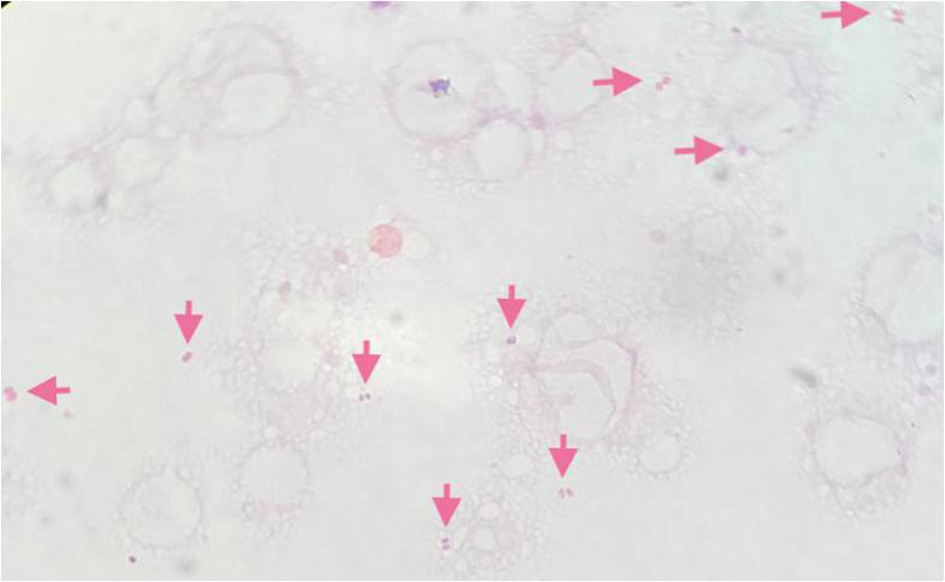 Click for large image | Figure 2. Gram stain of blood cultures demonstrating Gram-negative diplococci in pairs suggestive of Neisseria species. |
 Click for large image | Figure 3. Growth of Neisseria gonorrhoeae on microbiologic culture media. Visible colonies on chocolate agar. |
Patient completed a 7-day course of intravenous ceftriaxone (1 g/day) plus a single 1 g oral dose of azithromycin, with significant clinical improvement, being discharged 9 days after admission. Her partner was referred for counseling and treatment. During 3 months of follow-up, the patient remained asymptomatic.
| Discussion | ▴Top |
STIs represent an increasingly relevant public health problem. More than one million STIs are acquired every day, and gonorrhoeae is among the most common STIs worldwide, with an estimated 87 million new cases in 2016 [4]. In the European Union/European Economic Area (EU/EEA), gonorrhoeae is the second most notified STI after chlamydia [5]. The sexually transmitted pathogen N. gonorrhoeae is regarded as being on the way to becoming an untreatable superbug due to emerging AMR [6].
N. gonorrhoeae is transmitted during vaginal, oral, or anal sex with an infected person, and during childbirth. Urethral infections caused by N. gonorrhoeae among men can produce symptoms that cause them to seek curative treatment soon enough to prevent sequelae. Among women, gonococcal infections are commonly asymptomatic or might not produce recognizable symptoms until complications have occurred, which was the case in our patient. N. gonorrhoeae can spread through the bloodstream resulting in DGI, which occurs only in 0.5% to 3% of patients infected with N. gonorrhoeae. The likelihood of the organism spreading to the joints and other tissues depends upon host, microbial, and possibly immune factors. Presenting signs and symptoms may include fever, chills, malaise, polyarthralgia of small and/or large joints, tenosynovitis, and dermatitis; this panoply of symptoms were present in our patient. Symmetrical polyarthralgia is uncommon [7].
The number of cases is increasing, and the largest increases (> 15 cases/year) were reported by France and Portugal [5].
As described in the literature [1-3], arthritis-dermatitis syndrome corresponds to the classic findings of joint disease (86% of DGI), cutaneous lesions (60% of DGI) and tenosynovitis occurring in unison and is primarily a clinical diagnosis, consistent with the case presented. If untreated, progression to pyogenic septic arthritis occurs in less than a third of patients [1], which did not happen in our patient given the rapid diagnosis and initiation of treatment. The differential diagnosis can include bacterial endocarditis with septic embolization, chronic meningococcemia, erythema multiforme, rat-bite, rickettsial disease, and secondary syphilis [8].
Although pustules are thought to be the result of bacterial embolization, cultures tend to be negative since N. gonorrhoeae is fragile and requires unique conditions to grow. NAAT and cultures from mucosal sites, urine polymerase chain reaction test and biopsy of cutaneous lesions are all plausible diagnostic methods [9].
Growing concern for antibiotic resistance in recent decades has presented a new challenge in treating patients with local and DGIs. The majority of clinical isolates are resistant to penicillin, tetracyclines, and fluoroquinolones; thus, these drugs are no longer recommended for treatment [10]. Susceptibility testing now focuses on emerging resistance to cephalosporins and azithromycin. Currently, the DGI gold standard treatment is parenteral ceftriaxone (1 g) for a duration of 7 - 14 days alongside with a single dose of azithromycin for combination therapy to reduce the emergence of resistance and treat possible C. trachomatis coinfection, which was the scheme performed in our patient [11].
We report the case of a 27-year-old woman presenting with DGI. DGI is rare and the presentation with classic triad tenosynovitis, dermatitis, and polyarthralgia without purulent arthritis is even rarer. Diagnosis was confirmed by urine probe NAAT from mucosal and blood cultures, although positive blood cultures are found only in 50% of patients with DGI that present with arthritis-dermatitis syndrome [2].
It is imperative that healthcare providers are educated on the clinical signs and symptoms of this condition, including its cutaneous and articular manifestations.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent has been signed by the patient.
Author Contributions
MDC wrote the manuscript and conducted patient interviews; NZP wrote the manuscript; RM conducted patient interviews and took the skin lesions photo; RVF conducted patient interviews; MO provided Figures 1, 2; All authors reviewed the final manuscript.
| References | ▴Top |
- Burns JE, Graf EH. The Brief Case: Disseminated Neisseria gonorrhoeae in an 18-Year-Old Female. J Clin Microbiol. 2018;56(4):e00933-17.
doi pubmed - Hoving V, Borg EJT. A young male with arthritis and skin lesions. Arch Rheumatol. 2018;33(3):387-388.
doi pubmed - Rice PA. Gonococcal arthritis (disseminated gonococcal infection). Infect Dis Clin North Am. 2005;19(4):853-861.
doi pubmed - World Health Organization. Report on global sexually transmitted infection surveillance 2018. 2018.
- European Centre for Disease Prevention and Control. Introduction to the annual epidemiological report. Stockholm, 2017.
- Centers for Disease Control and Prevention. CDC. 2013. [Online]. Available: www.cdc.gov/drugresistance/biggest_threats.html. [Accessed 01 Julho 2019].
- Tuttle CS, Van Dantzig T, Brady S, Ward J, Maguire G. The epidemiology of gonococcal arthritis in an Indigenous Australian population. Sex Transm Infect. 2015;91(7):497-501.
doi pubmed - English JC, Monk JS. Gonococcal dermatitis-arthritis syndrome. Am Fam Physician. 1986;34(1):77-79.
- Centers for Disease Control and Prevention. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae - 2014. MMWR Recomm Rep. 2014;63(RR-02):1-19.
- Workowski KA, Bolan GA, Centers for Disease C, Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64(RR-03):1-137.
- Sexually transmitted diseases: summary of 2015 CDC treatment guidelines. J Miss State Med Assoc. 2015;56(12):372-375.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


