| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 12, Number 8, August 2021, pages 319-324
Diagnosing Disseminated Nocardiosis in a Patient With COVID-19 Pneumonia
Francis Atemnkenga, b, James Duceya, Ambreen Khalila, Azza Elemama, Keith Diaza
aRichmond University Medical Center, Staten Island, NY, USA
bCorresponding Author: Francis Atemnkeng, Richmond University Medical Center, Staten Island, NY, USA
Manuscript submitted May 24, 2021, accepted June 10, 2021, published online July 3, 2021
Short title: Nocardiosis in COVID-19 Pneumonia
doi: https://doi.org/10.14740/jmc3716
| Abstract | ▴Top |
Signs and symptoms of atypical pneumonia include fever, shortness of breath, cough, and chest pain. During the coronavirus disease 2019 (COVID-19) pandemic, identifying other causes of febrile respiratory illness in patients who tested positive for COVID-19 has been very challenging. Concerns over infecting healthcare personnel and other patients can impede further evaluations like bronchial lavage, lung biopsies, and other invasive tests. A very high index of suspicion, perhaps unreasonably so, is required to perform invasive tests to investigate alternative possible causes of the illness. We present the case of a 63-year-old man who presented to the hospital with dyspnea. Chest X-ray demonstrated a consolidation in the left lower lobe lung field with a possible underlying mass, and the patient tested positive for COVID-19. He received the standard treatment for COVID pneumonia at the time in our institution (remdesivir and dexamethasone), empiric antibiotics for community-acquired pneumonia, and was eventually discharged home with supplemental oxygen. Several days later, the patient returned to the hospital again with worsening dyspnea and was readmitted. Persistent illness and worsening imaging prompted bronchoscopy. The bronchoscopy showed narrowing of the airway in the left upper lobe, and Nocardia asteroides was isolated from bronchial aspirate. The isolation of Nocardia prompted an investigation for central nervous system involvement with an magnetic resonance imaging (MRI) of the head. The MRI demonstrated multiple bilateral ring-enhancing lesions in the brain. To our knowledge, this is the first reported case of disseminated nocardiosis superimposed on COVID-19 pneumonia.
Keywords: Nocardia; COVID-19; Pneumonia; Meningitis; Disseminated nocardiosis
| Introduction | ▴Top |
Since its identification in Wuhan, China, coronavirus disease 2019 (COVID-19) presents with a variable spectrum of disease ranging from asymptomatic to multiple organ failure requiring prolonged critical care. Common symptoms include shortness of breath, cough, chest pain, anosmia, anorexia, nausea, diarrhea, and can be as severe as multiorgan failure [1]. Most patients who require hospitalization suffer primarily from respiratory symptoms, and frequently demonstrate imaging findings consistent with atypical pneumonia. The most common imaging findings include patchy ground-glass opacities, with a peripheral posterior-basilar predilection. However, many other patterns have also been described [2]. The diversity of COVID-19 presentation renders identification of other underlying pathologies very challenging, as the presenting signs and symptoms can be linked to COVID-19.
Nocardiosis is a localized or disseminated infection caused by the actinomycete Nocardia species which primarily affects immunocompromised patients [3]. Nocardiosis is commonly diagnosed in patients afflicted with AIDS, malignancies, as well as organ transplant recipients [3]. It also has a marked tendency to recur despite appropriate therapy [4, 5]. Nocardia asteroides, and to a lesser extent, Nocardia brasiliensis are responsible for most cases of nocardia pneumonia. Nocardiosis presents as acute, sub-acute, or chronic infection, and represents a high morbidity and mortality rate, 44% in disseminated cases [6, 7]. Symptoms include fever, anorexia, productive cough, and chest pain. Neurologic signs may also be present when infection involves the central nervous system. Chest X-ray findings for nocardia pneumonia range from infiltrates to lobar consolidation, as well as abscesses, cavitation, and pleural effusion [8].
In this article, we present a case of a patient initially admitted and treated for COVID pneumonia, discharged home on supplemental oxygen, and was subsequently readmitted due to persistent worsening dyspnea. Further evaluation revealed Nocardia asteroides from bronchial washing, and magnetic resonance imaging (MRI) of the head confirmed central nervous system involvement.
| Case Report | ▴Top |
Investigations
A 63-year-old morbidly obese man with a past medical history of type 2 diabetes mellitus was brought in by ambulance complaining of shortness of breath and productive cough, which started 1 week prior to presentation. Patient was initially treated by his primary care provider with 5-day course of azithromycin. His symptoms were persistent and progressive, prompting him to seek further medical evaluation. In the emergency room (ER), patient’s initial oxygen saturation was 77% on room air, improved to 98% on application of a non-rebreather mask (NRM). Initial physical examination was significant for dyspnea and inspiratory crackles on the left lower lung field.
Diagnosis
Initial chest X-ray demonstrated a consolidation in the left lower lobe lung field with a possible underlying mass (Fig. 1a). Further evaluation revealed infection with COVID-19 based on PCR of nasal swab, as well as elevated inflammatory markers, as seen in Table 1.
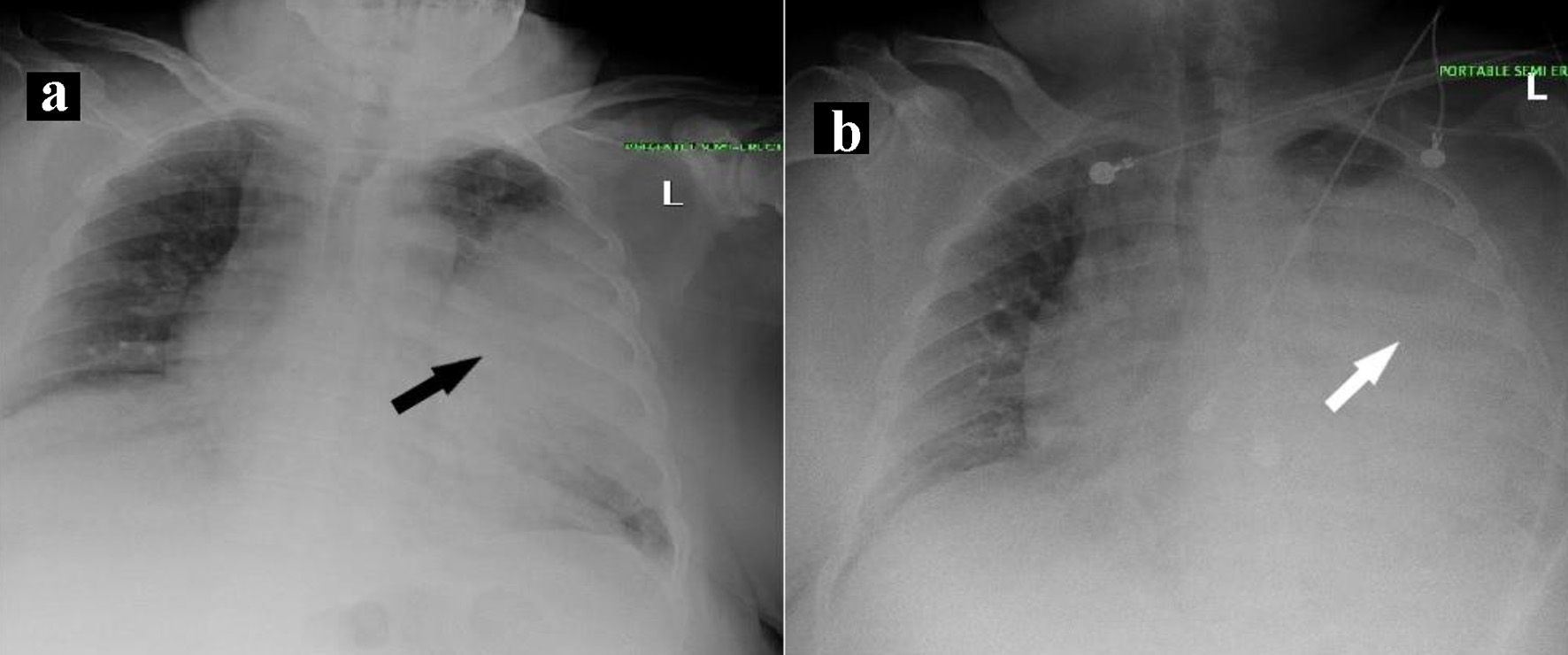 Click for large image | Figure 1. Chest X-ray findings during initial hospital admission. (a) Chest X-ray on day 1 of admission. Black arrow shows consolidation of left mid to lower lung field with possibility of an associated underlying mass. (b) Chest X-ray on day 3 of admission. White arrow shows near-complete opacification of the left hemithorax with minimal sparing of the apical region. |
 Click to view | Table 1. Laboratory Values on Day 1 of Initial Hospital Admission |
Initial treatment included 10 days of remdesivir, dexamethasone, and enoxaparin for COVID pneumonia. Antibiotic regimen of ceftriaxone and azithromycin was also administered for treatment of community-acquired pneumonia. Chest computed tomography (CT) demonstrated consolidation involving the left upper lobe, patchy infiltrates in the left lower lobe, and moderate left pleural effusion. On day 2 of admission, the patient’s respiratory status worsened, requiring non-invasive continuous positive airway pressure (CPAP). The clinical course progressed with respiratory support alternating between CPAP and NRM with FiO2 and pressures titrated as tolerated. Thoracentesis yielded 1,400 mL of exudative fluid demonstrated by an effusion protein to serum protein ratio of 0.6. Culture of the fluid was negative for any bacteria, and cytology revealed many macrophages, but no malignant cells. The clinical course was complicated by significantly elevated blood glucose levels, ranging in the high 300s to 400s mg/dL throughout the day, which remained difficult to control throughout his admission, likely secondary to the steroids, managed with subcutaneous insulin. Hemoglobin A1c (HbA1c) on admission was 13.7% implying poorly controlled diabetes mellitus.
On day 14 of admission, the patient was on CPAP with a pressure of 12 mm Hg and FiO2 of 80%. A repeat chest CT showed a 6.9 × 5.3 cm left upper lobe mass, consolidations in the left upper and lower lobes with air bronchograms, as well as vague nodular densities in right upper lobe (Fig. 2). This prompted a needle biopsy of the left upper lobe mass by interventional radiology, and pathology demonstrated non-necrotizing chronic granulomatous inflammatory changes with crystalloid deposition. There was no evidence of fungal growth, and iron depositions were present, a finding associated with COVID-19 pneumonia. A repeat COVID-19 PCR test was negative on day 20 of admission. The patient tolerated de-escalation of respiratory support down to supplemental oxygen through nasal cannula and was discharged home on day 26.
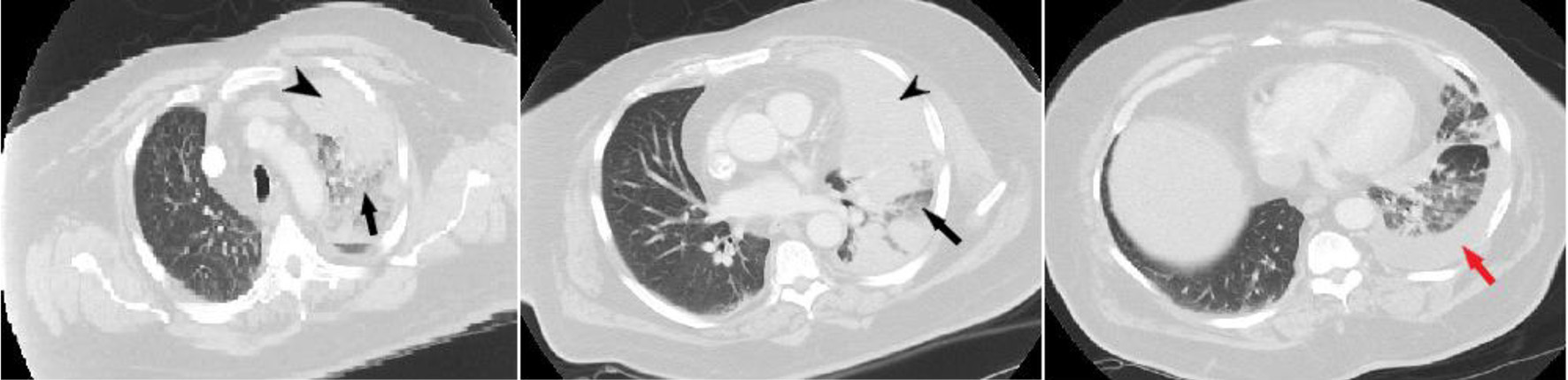 Click for large image | Figure 2. Results of chest computed tomography with contrast. Black arrowhead shows left upper lobe mass extending from chest wall to the mediastinum. Black arrow shows consolidation with air bronchograms. Red arrow shows left pleural effusion. |
One week after discharge, the patient was again brought in by ambulance from home with worsening shortness of breath. Chest X-ray showed near-total opacification of the left hemithorax, which had progressed from the imaging studies prior to discharge (Fig. 3). Repeat chest CT did not demonstrate any significant changes from the previous study and COVID-19 PCR by nasal swab was negative. The patient was empirically started on linezolid and piperacillin/tazobactam. Considering worsening clinical condition, it was decided to perform bronchoscopy with bronchoalveolar lavage to further evaluate the left upper lobe consolidation, which did not demonstrate an endobronchial mass or lesion. There were diffuse polypoid mucosal lesions with severe airway narrowing (Fig. 4). Samples were sent for bacterial, mycobacterial, fungal cultures, and cytology, including COVID-19 testing by PCR. The patient completed 10 days of linezolid and piperacillin/tazobactam and clinically improved, with respiratory support deescalated to 5 L of nasal cannula (NC). Preliminary report of the bronchial washing showed no growth of Mycobacteria, no organism on gram stain, no yeast isolated on fungal culture, and negative for COVID-19. The cytology report was negative for malignant cells but did demonstrate the presence of many neutrophils and sparse foamy macrophages. On day 13 of this admission, the patient was discharged home on NC while awaiting final culture results.
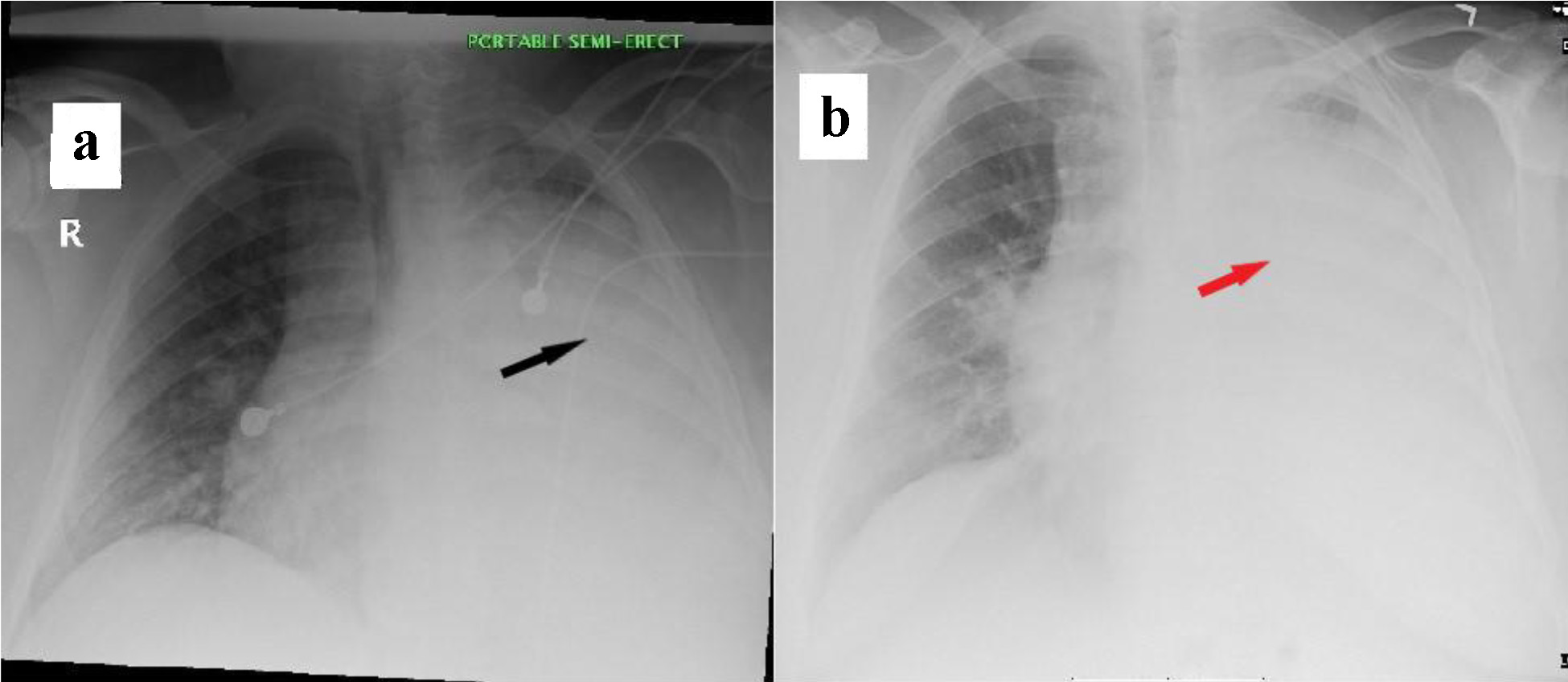 Click for large image | Figure 3. Chest X-ray findings during readmissions. (a) Chest X-ray on day of first readmission. Black arrow shows diffuse dense opacification of the left hemithorax with minimal sparing of the extreme apex. (b) Chest X-ray on day of second readmission. Red arrow shows opacification of left hemithorax with minimal sparing of the apex. |
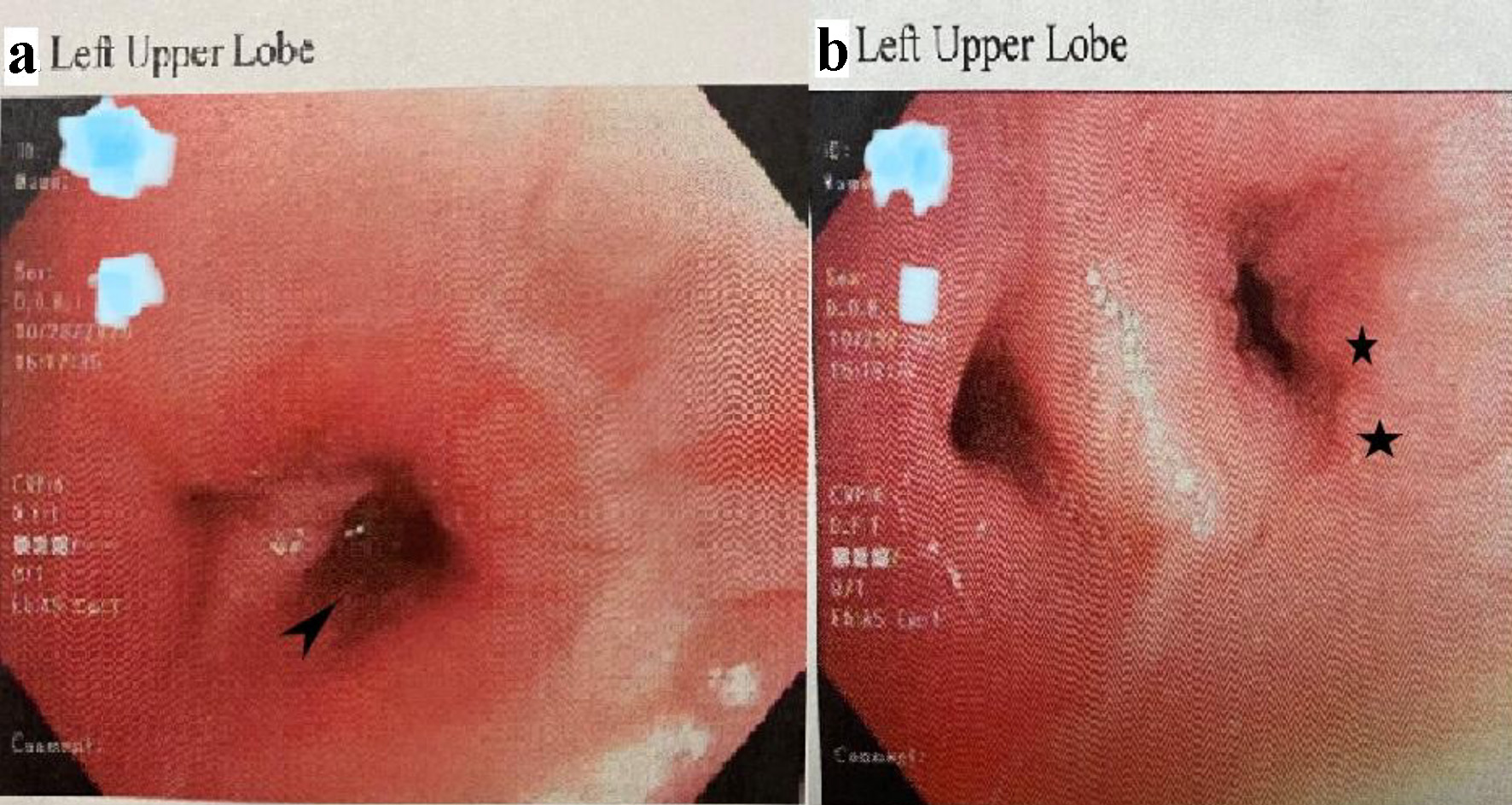 Click for large image | Figure 4. Images of bronchoscopy showing severe airway narrowing of left bronchi. (a) Left upper lobe (apical posterior). Arrowhead shows narrowing of the airway. (b) Left upper lobe (carina and lingula). Black star shows diffuse polypoid mucosal findings with irregular contours. |
On outpatient follow-up with the pulmonologist 2 weeks post-discharge, the patient continued to complain of dyspnea and associated chest pain. Subsequent chest X-ray demonstrated progression of the opacification of the left lung with minimal sparing of the extreme apex (Fig. 3). COVID-19 PCR nasal swab was again negative. Results of the cultures from the bronchial lavage now showed Nocardia species.
Treatment
With the worsening of dyspnea and chest X-ray findings, and the new diagnosis of Nocardia species, the decision was made to readmit the patient to the hospital. He was started on meropenem and trimethoprim/sulfamethoxazole (TPM/SMX), pending sensitivities and speciation of the organism. An MRI of the head during this third admission revealed multiple ring-enhancing lesions bilaterally in the cerebral and cerebellar cortexes with restricted diffusion (Fig. 5). At this time, the patient did not have any neurologic symptoms. Due to continuous dense consolidation and severe airway narrowing, there was a consideration for stenting in the left lung as seen on the bronchoscopy that was performed in the previous admission, so the patient was transferred to a tertiary care center capable of stent placement on day 4 of the third admission.
 Click for large image | Figure 5. Magnetic resonance imaging of head with gadolinium showing central nervous system involvement of Nocardia. Black arrows show multiple ring-enhancing lesions in the cerebral and cerebellar hemispheres bilaterally. |
Follow-up and outcomes
While in the tertiary hospital, the finalized culture and sensitivity studies from prior bronchoscopy revealed Nocardia asteroides which was resistant to Carbapenems, so meropenem was discontinued, and the patient was started on linezolid. He received linezolid and TMP/SMX via intravenous route for an additional 36 days before being discharged home on an oral form of linezolid and TMP/SMX for a total of 12 months and to follow up as an outpatient. The patient was reported to have neurologic deficits while in the tertiary center, but resolved as soon as meropenem was changed to linezolid. On subsequent follow-up as an outpatient 1 month later, he was seen by the infectious disease doctor and the pulmonologist, who noted improvement in clinical state and chest X-ray findings.
| Discussion | ▴Top |
COVID-19 presents with variable spectrum of disease ranging from asymptomatic to multiple organ failure resulting in a clinical course requiring prolonged critical care [1]. Treatment options are currently limited, and research is still ongoing on pharmacologic agents that can reduce morbidity and mortality in these patients. Currently, remdesivir, dexamethasone, and baricitinib have been shown to have some benefits in decreasing the mortality in patients with severe disease requiring critical care [9-11]. Our patient presented with dyspnea, which required NRM, so he was started on a combination of remdesivir and dexamethasone for 10 days as the standard of care in our institution. It remains unclear if the patient had pre-existing nocardiosis, or was predisposed due to COVID-19 pneumonia, or was especially susceptible secondary to immunosuppressive agents commonly used as part of the treatment regimen for COVID-19 infection.
Nocardia usually causes infections in immunosuppressed patients, but about a third of the patients infected are immunocompetent [6, 12]. Predisposing factors may have caused him to be infected by Nocardia species including uncontrolled diabetes mellitus with HbA1c of 13.7% and less likely the use of dexamethasone for the treatment of COVID-19. Given the nearly opacified lung on chest X-ray and dissemination to the brain seen on MRI, it is likely the patient had nocardiosis prior to initial presentation to the hospital. Under this assumption, the patient would be among the rare immunocompetent individuals who develop disseminated nocardia infection.
The presentation of febrile respiratory illness and isolation of COVID-19 initially overshadowed a concomitant underlying nocardiosis. In the era of the COVID-19 pandemic, significant concern exists regarding performing routine procedures that may cause aerosolization and increase infectivity, such as bronchoscopy. These procedures are commonly necessary to evaluate lung pathology, and deferment of invasive evaluation likely delayed the diagnosis of nocardia in this patient, which requires the isolation of the bacteria [12]. Due to the persistence of symptoms, a needle biopsy was performed, which showed findings still consistent with COVID-19. Finally, a bronchoscopy isolated Nocardia asteroides. This complexity of the diagnosis is what renders the case very unique. To date, no case has been reported showing isolation of Nocardia species in a patient infected with COVID-19.
Upon isolation of the Nocardia species, it is usually recommended to treat with two or three intravenous agents while awaiting antibiotic sensitivities. Empiric treatment usually contains TMP/SMX with either amikacin, imipenem, or a third-generation cephalosporin [6]. Our patient was empirically started on TMP/SMX and meropenem while awaiting the final sensitivity profile, which showed resistance to imipenem, prompting a change in therapy to linezolid to which the pathogen was sensitive. The length of treatment of patients with associated central nervous system (CNS) involvement can be as long as 12 months. Our patient received short courses of ceftriaxone and linezolid during subsequent readmissions, which might have caused his temporary clinical improvement during his hospital stay, but discontinuation of the treatment resulted in relapse upon discharge. Once the organism was identified and long-term treatment initiated, our patient did not have any further relapse of symptoms.
Nocardia species can disseminate to any organ and the resilience of the pathogen results in a high rate of relapse, despite appropriate therapy. The delay in diagnosis and treatment may have possibly allowed for progression from nocardia pneumonia to disseminated nocardiosis involving the central nervous system. Due to the association between nocardia infection and CNS involvement, a brain MRI was done with gadolinium that confirmed multiple ring-enhancing lesions in the brain. This MRI result was critical in definitive diagnosis of the extent of this patient’s disease burden and greatly influenced the decision of the length of therapy required to appropriately treat our patient, as well as necessitate outpatient follow-up.
Conclusion
We presented the case of a 63-year-old man who presented with dyspnea, initially treated for COVID pneumonia, and discharged home on 3 L NC. He later returned with progressive symptomatology and ultimately diagnosed with disseminated nocardiosis on further assessment. This case highlights the needs to maintain a high index of suspicion in COVID-19 patients who fail to improve despite current goal-directed therapies.
Acknowledgments
None to declare.
Financial Disclosure or Funding
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
F. Atemnkeng collected the data, guided the literature search, wrote the manuscript, and is the research guarantor. J. Ducey, A. Khalil, and A. Elemam helped with the data collection and writing of the article. K. Diaz reviewed and supervised the study.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720.
doi pubmed - Cozzi D, Albanesi M, Cavigli E, Moroni C, Bindi A, Luvara S, Lucarini S, et al. Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: findings and correlation with clinical outcome. Radiol Med. 2020;125(8):730-737.
doi pubmed - Boiron P, Locci R, Goodfellow M, Gumaa SA, Isik K, Kim B, McNeil MM, et al. Nocardia, nocardiosis and mycetoma. Med Mycol. 1998;36(Suppl 1):26-37.
- Filice GA. Nocardiosis in persons with human immunodeficiency virus infection, transplant recipients, and large, geographically defined populations. J Lab Clin Med. 2005;145(3):156-162.
doi pubmed - Khorrami P, Heffeman EJ. Pneumonia and meningitis due to Nocardia asteroides in a patient with AIDS. Clin Infect Dis. 1993;17(6):1084-1085.
doi pubmed - Marrie TJ. Pneumonia caused by Nocardia species. Semin Respir Infect. 1994;9(3):207-213.
- Radhakrishnan K, Heaton D. Disseminated nocardiosis. Intern Med J. 2008;38(9):740.
doi pubmed - Smilack JD. Images in clinical medicine. Pulmonary and disseminated nocardiosis. N Engl J Med. 1999;341(12):885.
doi pubmed - Titanji BK, Farley MM, Mehta A, Connor-Schuler R, Moanna A, Cribbs SK, O'Shea J, et al. Use of baricitinib in patients with moderate to severe coronavirus disease 2019. Clin Infect Dis. 2021;72(7):1247-1250.
doi pubmed - Recovery Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384(8):693-704.
doi pubmed - Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, Hohmann E, et al. Remdesivir for the treatment of COVID-19 - final report. N Engl J Med. 2020;383(19):1813-1826.
doi pubmed - Georghiou PR, Blacklock ZM. Infection with Nocardia species in Queensland. A review of 102 clinical isolates. Med J Aust. 1992;156(10):692-697.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


