| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 12, Number 9, September 2021, pages 373-376
A Fatal Case of Massive Verapamil Overdose: An Overview of the Treatment Options
Francis Atemnkenga, b, Jawad Shabania, Lu Chena, Bhavesh Galaa, Jonathan Ramalhoa, Keith Diaza, Jay Nfonoyima
aRichmond University Medical Center, Staten Island, NY, USA
bCorresponding Author: Francis Atemnkeng, Richmond University Medical Center, Staten Island, NY, USA
Manuscript submitted July 30, 2021, accepted August 13, 2021, published online August 25, 2021
Short title: A Fatal Case of Verapamil Overdose
doi: https://doi.org/10.14740/jmc3763
| Abstract | ▴Top |
Calcium channel blocker overdose is usually very fatal and challenging to manage. The patients are usually asymptomatic on admission, but deteriorate very rapidly. Currently, there is no specific antidote, and the treatment is supportive requiring high level of critical care, and may necessitate extracorporeal membrane oxygenation. The use of high-dose insulin is reported to help stabilize the blood pressure and wean off inotropes. The recommendations for supportive treatment in patients with calcium channel blocker overdose are based upon low-quality evidence reports including case series and animal studies. We present the case of a 55-year-old male with a history of atrial fibrillation who was admitted to the hospital 30 min after intentionally ingesting 80 tablets of 180 mg extended release verapamil. On admission, the patient was asymptomatic, but electrocardiogram (ECG) showed a complete heart block which necessitated a transcutaneous pacing, followed by transvenous pacemaker placement. Rapid deterioration of the patient’s hemodynamic status led to the patient getting intubated and was started on pressors as well as high-dose insulin. Despite all the aggressive measures, the patient died in less than 24 h after being admitted. We report this case to provide a brief review of the treatment options available at this time, because to date, there is no specific antidote for such overdose, and it remains very fatal despite the amount of supportive care provided.
Keywords: Calcium channel blocker overdose; Verapamil overdose; Antidote; Atrioventricular dissociation; High-dose insulin
| Introduction | ▴Top |
Calcium channel blocker overdose is very fatal and challenging to manage with a mortality of approximately 38% [1]. According to the latest 2019 National Poison Data System (NPDS) Annual Report published by The American Association of Poison Control Centers, calcium channel blockers, alone or in combination with other substances, are listed as the sixth leading cause of fatal drug-related toxicities [2]. Patients may present to the hospital asymptomatic, but deteriorate very rapidly. Ingesting more than 5 - 10 times the usual dose may lead to signs and symptoms such as drowsiness, hypotension, bradycardia and respiratory and heart failures [3]. Currently, there is no antidote for calcium channel blocker overdose, and treatment options are supported by very low-quality evidence including case series and animal studies [4-6]. The treatment is usually supportive and options include gastric lavage, intravenous (IV) calcium, glucagon, catecholamines, and high-dose insulin. Patients might also get severe heart blocks requiring transvenous pacemaker. For severely poisoned patients, extracorporeal membrane oxygenation (ECMO) may be a necessity if available in the hospital [7-10]. We present a fatal case of massive, intentional sustained-release verapamil overdose despite optimal supportive treatment. This case highlights the quick deterioration of such patients, the lack of potential reversal of outcomes, and the need for novel treatments such as antidotes.
| Case Report | ▴Top |
Investigations
A 55-year-old male with a history of hypertension, atrial fibrillation, chronic obstructive pulmonary disease (COPD), obstructive sleep apnea, major depressive disorder, pulmonary embolism and upper gastrointestinal bleed presented to the emergency department (ED) 30 min after he intentionally ingested 80 tablets of 180 mg sustained-release verapamil. At the time of presentation, the patient endorsed suicidal ideation, headache, dizziness and mild shortness of breath. He denied chest pain, palpitations, abdominal pain, nausea and vomiting. When the patient arrived in the ED, he was alert and oriented to person, place and time, and in no apparent distress. His blood pressure was 126/80 mm Hg, with a heart rate of 93 beats/min (bpm). The lungs were clear to auscultation bilaterally, heart sounds were regular with no murmurs.
Diagnosis
Electrocardiogram (ECG) showed a third degree heart block with narrow complex ventricular escape rhythm (Fig. 1); chest X-ray was unremarkable. Laboratory studies on admission showed a blood glucose of 172 mg/dL, corrected calcium of 9.2 mg/dL, hypomagnesemia (1.6 mg/dL) and low-normal levels of potassium (3.6 mmol/L).
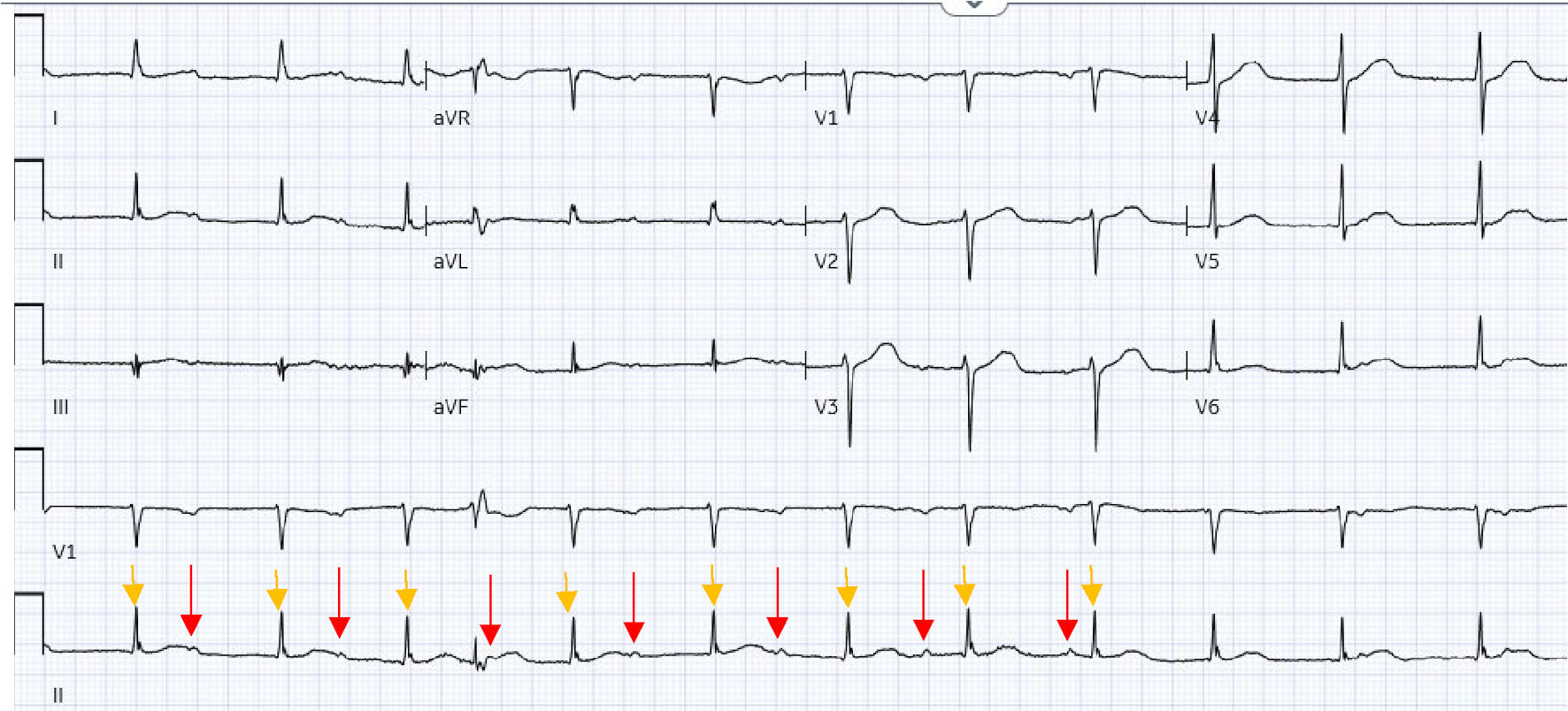 Click for large image | Figure 1. ECG when patient arrived in the emergency department. It showed atrioventricular dissociation with accelerated junctional rhythm with occasional premature ventricular complexes. P waves (red arrows) were not in accordance with QRS complexes (yellow arrows). ECG: electrocardiogram. |
Treatment
An urgent cardiology consult was called, and the patient was immediately placed on telemetry monitoring while a transcutaneous pacemaker along with a trial of atropine were attempted without resolution of the heart block. The patient was administered IV fluids and electrolyte repletion. An immediate consult was placed with the Regional Poison Control Center as well, and they recommended 50 g of activated charcoal which was administered, and to start whole bowel irrigation with polyethylene glycol.
In the meantime, the patient was transferred to the cardiac intensive care unit (CCU) and was started on IV calcium gluconate. About 1 h after the patient was transferred to CCU, he quickly became hypotensive and bradycardic with a respiratory rate in the 40s and an oxygen saturation level of 92% on 4 L of oxygen through nasal cannula. Due to his inability to protect his airway, the decision was made to intubate the patient. A right internal jugular vein transvenous pacemaker was placed, as well as a left internal jugular vein central line for IV access; and he was started on norepinephrine and dopamine drips. For more optimal blood pressure control, an arterial line was placed.
A repeat finger stick blood glucose was 275 mg/dL, most likely due to the verapamil overdose. The patient was started on insulin with a loading dose of 1 U/kg, with a total of 172 units given as IV push, followed by a continuous drip at a dose of 0.5 U/kg/h, with a total of 86 U/h (see blood glucose measurements in Fig. 2).
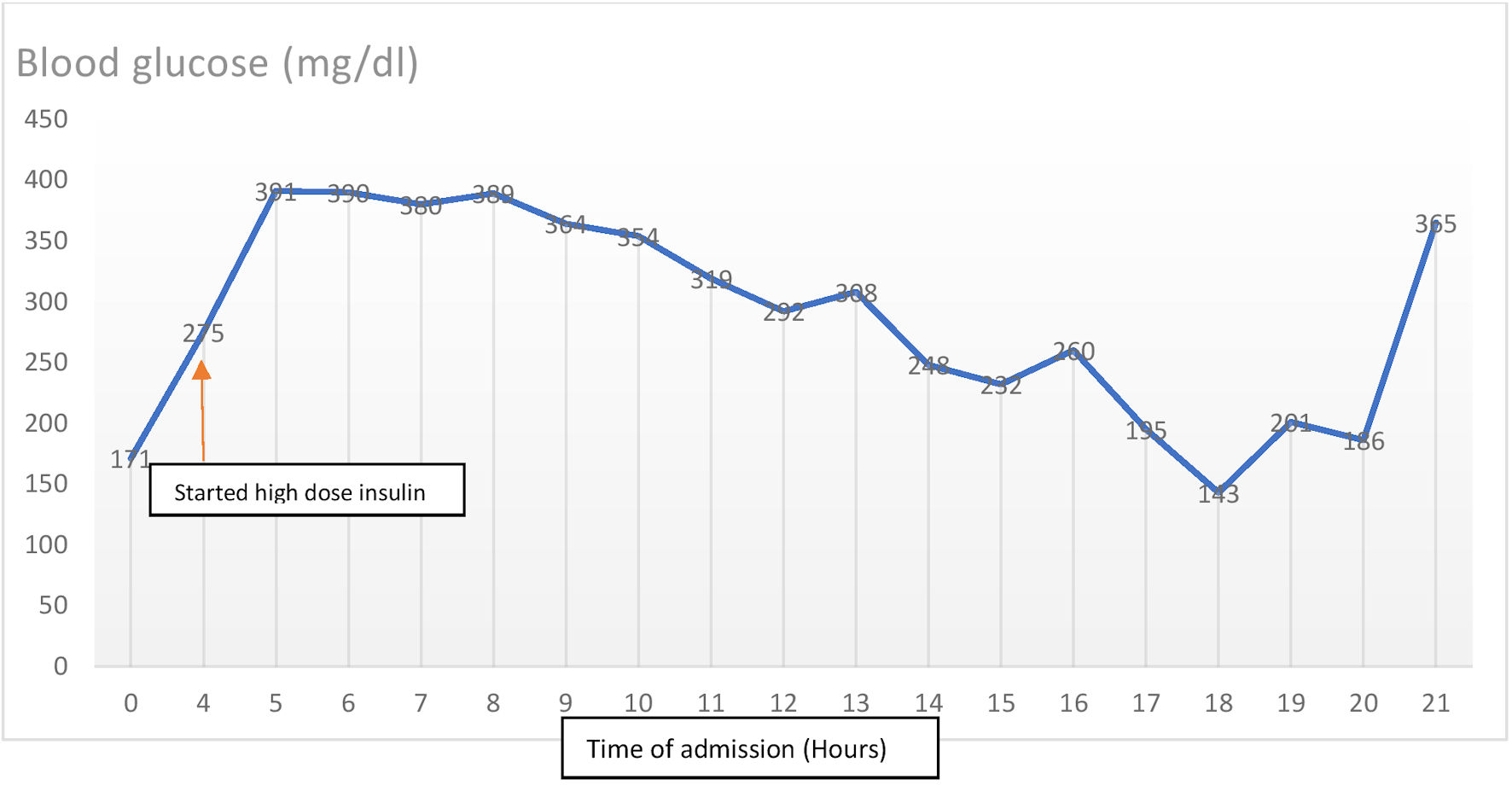 Click for large image | Figure 2. Evolution of blood glucose during admission and after starting high dose insulin. |
Despite receiving norepinephrine at a rate of 40 µg/min and dopamine at a rate of 20 µg/kg/min, the patient’s mean arterial pressure was persistently less than 65 mm Hg; thus vasopressin drip was added at a rate of 0.03 units/min (see blood pressure measurements in Fig. 3). The oxygen saturation recorded was ranging between 70% and 80% on assist-control mode of ventilation set at rate of 18 breaths/min, tidal volume of 500 mL/breath, fraction of inspired oxygen (FiO2) of 100% and a positive end-expiratory pressure (PEEP) of 10 cm H2O.
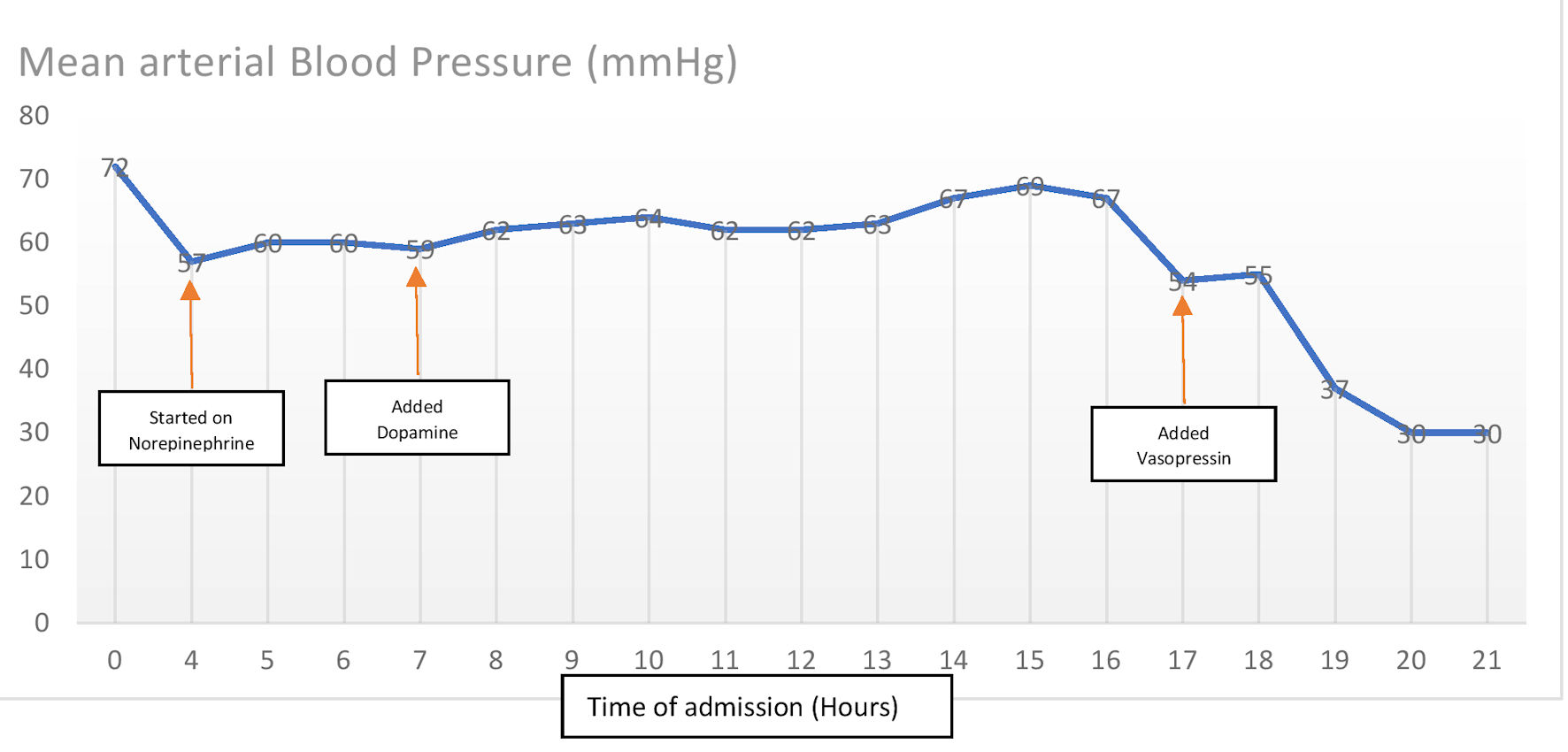 Click for large image | Figure 3. Evolution of blood pressure during the course of admission. |
Follow-up and outcomes
The patient was considered for ECMO at a nearby specialized center but he was deemed as a poor candidate due to being very unstable for transfer. Bedside echocardiography was performed, which showed adequate ejection fraction and no obvious regional wall motion abnormalities. His refractory shock was consistently unchanged despite addition of phenylephrine and the patient subsequently sustained cardiopulmonary arrest after about 22 h since admission, without return of spontaneous circulation.
| Discussion | ▴Top |
The potential toxicity of calcium channel blockers is often underappreciated, and currently, there are no antidotes present. The non-dihydropyridine group such as verapamil selectively blocks the L-type calcium channels in the myocardium, which are responsible for myocardial contractility, vascular smooth muscle contraction, as well as conducting and pacemaker cells [11]. Verapamil toxicity will therefore cause peripheral vasodilation, decreased cardiac contractility and bradycardia. Our patient who ingested a massive dose of verapamil (14,400 mg) subsequently became hypotensive due to the decreased contractility and the vasodilatory effects of the medication, as well as developing an atrioventricular dissociation as seen on the ECG. Verapamil is highly protein bound, with clearance through the liver. The extended release form, as consumed by our patient prolongs the effects and renders the absorption unpredictable due to its high volume of distribution. Most of the time, the patients are usually asymptomatic on arrival, but can deteriorate very rapidly, therefore requiring frequent reassessment.
Presently, there is no antidote for calcium channel blocker overdose, and current treatment options are based upon limited evidence from case series and animal studies [4]. These treatment options are mainly supportive, until the medication reaches a safe level in the blood stream. The first step to treatment is to consult a poison control center and report the case. Orogastric lavage is usually recommended in patients who present within 1 - 2 h following ingestion of greater than 5 - 10 times the standard dose. Activated charcoal should also be administered regardless if the patients are asymptomatic. Our patient, who initially did not have any symptoms, received activated charcoal and whole bowel irrigation as recommended by poison control. The presence of atrioventricular dissociation with ventricular escape rhythm present on the ECG upon admission probably represented the possibility that a large quantity of the verapamil had already been absorbed, or the patient had ingested it longer than the 30 min prior, contrary to which he informed us. Despite the activated charcoal and the continuous bowel irrigation, our patient deteriorated rapidly and became hypotensive, bradycardic and developed respiratory failure which required intubation, transvenous pacemaker placement and the use of vasopressors.
Patients who develop severe symptoms require simultaneous interventions including stabilization of airway, IV boluses of isotonic crystalloid, IV calcium, glucagon, high-dose insulin and glucose, vasopressors, and sometimes ECMO as last resort [6]. The choice of vasopressors will require a direct-acting agent with positive inotropy, chronotropy and vasoconstrictive effects such as norepinephrine, and to be titrated upwards with a goal mean arterial blood pressure of 65 mm Hg or higher. Despite initiating these treatment options on our patient as well as starting norepinephrine, a dose of 40 µg/min did not raise the mean arterial pressure above 65 mm Hg, so dopamine was added. The use of high-dose insulin has also been shown to have positive inotropic effects in animal models and case reports [8]. Despite starting our patient on high-dose insulin therapy, the patient still had refractory hypotension, leading to the addition of a third vasopressor and eventually a fourth. Attempts were made to transfer the patient to a center capable of performing ECMO, but due to the patient being very unstable, the transfer could not be initiated. The dangerous combination of hypotension and bradycardia can be profound and refractory, even to maximal treatment. Despite all the therapeutic interventions, the patient died in less than 24 h of admission. This case highlights the fatality of calcium channel blocker overdose and the lack of an antidote, with treatment options based upon case series and animal studies.
Conclusions
Calcium channel blocker overdose is very fatal with a mortality of 38%, and symptoms can be refractory despite maximal treatment. Currently, there is no antidote and treatment options are based upon weak evidence from case series and animal studies. Further research is needed to obtain a cure, and to acquire stronger evidence for supportive treatment options.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors report no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
F. Atemnkeng collected the data, guided the literature search, wrote the manuscript, and is the research guarantor. J. Shabani, L. Chen, J. Ramalho, B. Gala, and K. Diaz helped with the data collection and writing of the article. J. Nfonoyim reviewed and supervised the study.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Watson WA, Litovitz TL, Rodgers GC, Jr., Klein-Schwartz W, Youniss J, Rose SR, Borys D, et al. 2002 annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 2003;21(5):353-421.
doi pubmed - Gummin DD, Mowry JB, Beuhler MC, Spyker DA, Brooks DE, Dibert KW, Rivers LJ, et al. 2019 annual report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 37th annual report. Clin Toxicol (Phila). 2020;58(12):1360-1541.
doi pubmed - Lindeman E, Alebring J, Johansson A, Ahlner J, Kugelberg FC, Nordmark Grass J. The unknown known: non-cardiogenic pulmonary edema in amlodipine poisoning, a cohort study. Clin Toxicol (Phila). 2020;58(11):1042-1049.
doi pubmed - St-Onge M, Dube PA, Gosselin S, Guimont C, Godwin J, Archambault PM, Chauny JM, et al. Treatment for calcium channel blocker poisoning: a systematic review. Clin Toxicol (Phila). 2014;52(9):926-944.
doi pubmed - Ashraf M, Chaudhary K, Nelson J, Thompson W. Massive overdose of sustained-release verapamil: a case report and review of literature. Am J Med Sci. 1995;310(6):258-263.
pubmed - Hofer CA, Smith JK, Tenholder MF. Verapamil intoxication: a literature review of overdoses and discussion of therapeutic options. Am J Med. 1993;95(4):431-438.
doi pubmed - Thanacoody R, Caravati EM, Troutman B, Hojer J, Benson B, Hoppu K, Erdman A, et al. Position paper update: whole bowel irrigation for gastrointestinal decontamination of overdose patients. Clin Toxicol (Phila). 2015;53(1):5-12.
doi pubmed - Kline JA, Tomaszewski CA, Schroeder JD, Raymond RM. Insulin is a superior antidote for cardiovascular toxicity induced by verapamil in the anesthetized canine. J Pharmacol Exp Ther. 1993;267(2):744-750.
pubmed - Boyer EW, Shannon M. Treatment of calcium-channel-blocker intoxication with insulin infusion. N Engl J Med. 2001;344(22):1721-1722.
doi pubmed - Durward A, Guerguerian AM, Lefebvre M, Shemie SD. Massive diltiazem overdose treated with extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2003;4(3):372-376.
doi pubmed - Katz AM. Cardiac ion channels. N Engl J Med. 1993;328(17):1244-1251.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


