| Journal of Medical Cases, ISSN 1923-4155 print, 1923-4163 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Med Cases and Elmer Press Inc |
| Journal website https://www.journalmc.org |
Case Report
Volume 12, Number 12, December 2021, pages 481-484
Acute Colonic Pseudo-Obstruction in Severe Falciparum Malaria: A Case Report
Peng Fei Yaoa, Peng Jiang Zhanga, He Donga, Yang Suna, b
aThe 940th Hospital of Joint Logistics Support Force of PLA, Lanzhou 730050, China
bCorresponding Author: Yang Sun, The 940th Hospital of Joint Logistics Support Force of PLA, Lanzhou 730050, China
Manuscript submitted September 29, 2021, accepted October 21, 2021, published online December 2, 2021
Short title: ACPO in Severe Falciparum Malaria
doi: https://doi.org/10.14740/jmc3801
| Abstract | ▴Top |
Severe falciparum malaria is associated with multiple organ dysfunctions. The most manifestations of severe falciparum malaria are cerebral malaria, acute lung injury, and acute kidney injury. Acute colonic pseudo-obstruction is extremely rare. Early recognition and management are essential because a delay in diagnosis is associated with substantial morbidity and mortality. A 29-year-old peacekeeper in the Democratic Republic of Congo (DRC) was diagnosed as severe falciparum malaria with high-grade fever, jaundice, electrolyte disturbance, and thrombocytopenia. Although adequate antimalaria therapy with intramuscular artemether was given, the patient had persistent fever, shallow and fast breathing, and abdominal pain. Investigations suggested a diagnosis of acute colonic pseudo-obstruction. Antimalarial therapy was continued with intravenous artesunate. And rectal decompression and fasting were taken. Soon, symptoms of colonic obstruction mitigated. And the patient was cured and discharged. Acute colonic pseudo-obstruction should be considered for severe malaria patients with abdominal distention and pain. The early diagnosis and proper management of the patient with severe malaria complicated with acute colonic pseudo-obstruction are the keys to a good prognosis.
Keywords: Acute colonic pseudo-obstruction; Malaria; Severe
| Introduction | ▴Top |
Severe malaria is a medical emergency that can rapidly develop into serious illness. Failure to make timely diagnosis and give urgent and appropriate treatment to the patient will result in multisystemic dysfunction, and eventually, death. There were an estimated 405,000 deaths from malaria globally in 2018, and 93% of them were caused by severe falciparum malaria [1]. The acute colonic pseudo-obstruction (ACPO) is a rare condition in the patient with severe malaria. There was no report so far. Early diagnosis and proper management are extremely important.
| Case Report | ▴Top |
Investigations
A 29-year-old male peacekeeper, deployed in the Democratic Republic of Congo (DRC) for 2 months, presented with a history of 3-day fever, headache, fatigue and 1-day jaundice. There was no past medical history. He was taking compound dihydroartemisinin tablets (dihydroartemisinin + piperaquine phosphate + trimethoprim) weekly as chemoprophylaxis since entering the mission area. Physical examination showed fever (39.4 °C), acute sick looking, poor spirit, yellow staining of skin and sclera.
Diagnosis
Pulse oxygen saturation was 96%. Glasgow coma scale (GCS) was 15. Ultrasonic examination of the abdomen showed splenomegaly. The blood smear revealed 8% parasitemia. The laboratory results after admission were summarized in Table 1. Of note were hyperbilirubinemia (total bilirubin 81.3 µmol/L), electrolyte disturbance, and thrombocytopenia. Hepatitis series tests were negative. A rapid diagnostic test was positive for Plasmodium falciparum. A diagnosis of severe falciparum malaria was made.
 Click to view | Table 1. Laboratory Investigations |
Treatment
We carried out antimalaria therapy with intramuscular artemether 240 mg at admission and 160 mg at 12, 24 h later (artesunate was temporarily unavailable), correcting dehydration and the electrolyte disturbance, and protecting liver function. The patient did not sweat and the body temperature did not drop after antimalarial treatment. It was above 39.0 °C. Thirty-six hours after admission, he felt left upper quadrant pain, combined by nausea, vomiting, and diarrhea, all of which occurred for three times. The pain was so severe that he could not take a deep breath or cough, resulting in shallow and fast breathing, and a pulse oxygen saturation of 92%. And this was followed with progressive abdominal distension and an inability to pass stool and flatus. On examination, the patient was extremely weak and tired. Without abdominal guarding and rigidity, tenderness was obvious in the left. There was no rebound tenderness. Bowel sounds disappeared. In addition, the blood smear revealed 5% parasitemia. Liver function deteriorated (total bilirubin 189.5 µmol/L), and platelets decreased further (52 × 109/L). Fifty-five hours after admission, his abdominal pain was significantly worse. The consciousness was gradually indifferent, and GCS was 13. Breath rate was 45/min, and pulse oxygen saturation was 89%. X-ray of the chest showed lung texture thickening and upright abdominal plain film indicating that the colon was dilated and gas accumulation in the splenic flexure (Fig. 1a). Ultrasound of the abdomen showed hepatomegaly and splenomegaly. So we considered the patient was complicated by ACPO. At this time artesunate was available and 2.4 mg/kg body weight administered intravenously (time = 0), then at 12 h and 24 h. At the same time, fasting, no retention enema, rectal decompression tubes and oral 30 mL paraffin oil were taken. One day after these measures, he passed a small quantity of feces; and abdominal pain and distension were relieved. Body temperature also gradually decreased. Blood test showed bilirubin level dropped than before (total bilirubin 165.7 µmol/L), platelets level rose to a certain extent (81 × 109/L), and the blood smear revealed 1% parasitemia. X-ray of the abdomen revealed that dilation of the left colon disappeared, and intestinal gas accumulation decreased (Fig. 1b). Five days after admission, the patient could tolerate oral therapy, so he completed a treatment of 3-day artemisinin-based combination therapies.
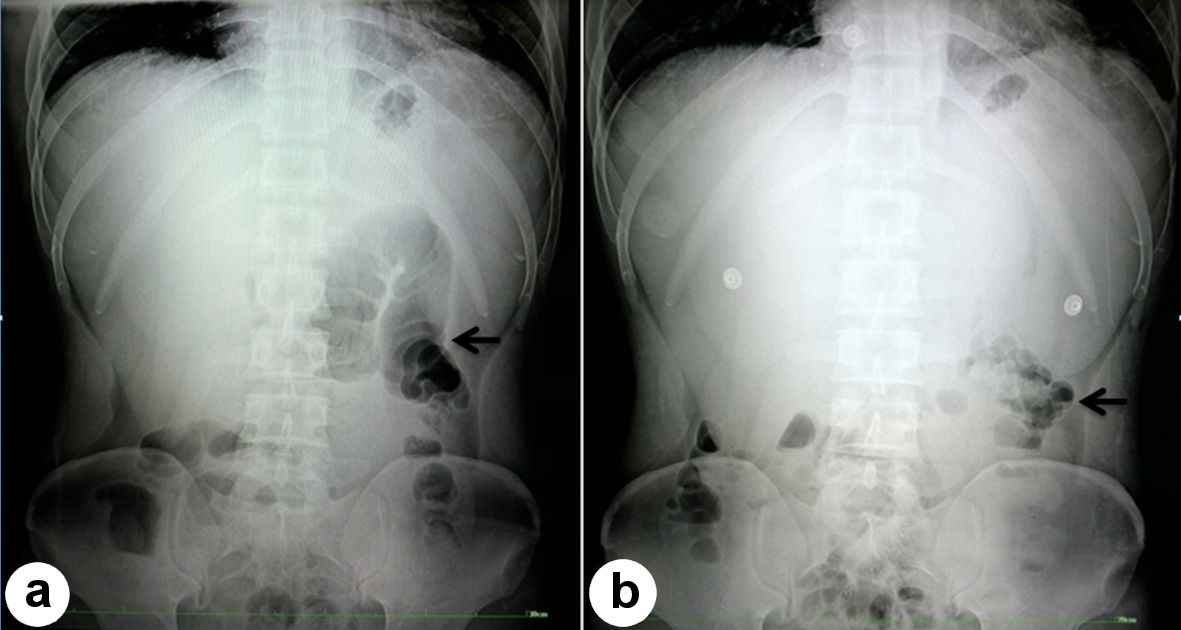 Click for large image | Figure 1. Upright abdominal plain film. (a) Fifty-five hours after admission, the colon was dilated and gas accumulation shown in the splenic flexure (arrow). (b) One day after taking new measures, dilation of the left colon disappeared and intestinal gas accumulation decreased (arrow). |
Follow-up and outcomes
We concluded that ACPO was secondary to malaria. Ten days later, all symptoms disappeared and the patient was discharged. His 1-month follow-up was unremarkable.
| Discussion | ▴Top |
As a peacekeeper in the DRC from Asia, the risk for severe falciparum malaria is greater due to lack of immunity. Various symptoms may appear. Abdominal pain is a common symptom of malaria. The causes of abdominal pain in malaria are diverse, such as gastroenteritis, hepatitis [2], acute abdomen [3], splenic rupture [4], acute pancreatitis [5], sub-acute intestinal obstruction [6], and so on. In this patient, abdominal pain affecting respiration was related to ACPO. ACPO is a rare condition characterized by acute colonic dilatation in the absence of mechanical obstruction [7]. It is even less common in adult malaria cases, and there was no report so far. However, several cases of sub-acute bowel obstruction caused by malaria have been reported. One is a 42-year-old man in Cameroonian [6] and the other is an 18-month-old girl in India [2].
ACPO is a functional obstruction characterized by absent peristalsis or peristalsis which can be present but in a non-propulsive form. It usually occurs in hospitalized patients with severe illness or trauma, or follows general, orthopedic, neurosurgical, gynecological or other surgical procedures [7], with an associated mortality rate of 15% to 44% because of colonic ischemia or perforation [8].The pathophysiology underlying ACPO resulted from malaria remains blurred.
After admission, the patient in this study was treated with artemether immediately,however his condition significantly aggravated. A non-immune adult and a few days of illness allowed a large number of plasmodium parasites to reproduce in the blood, leading to persistent hyperparasitemia. Infected red blood cell was sequestrated in microvascular beds of multiple organs, and resulted in microvascular occlusion and tissue ischemia [9]. Infected erythrocytes also adhered to surrounding uninfected red blood cells to form rosetting, or activated platelets to form clumping. Both rosetting and clumping further contributed to microvascular obstruction [10]. The splenic flexure of the colon is at the junction of the blood supply at the end of two arteries, which is prone to insufficient supply of blood. When the local circulation continues to stagnate without improvement, it can cause colonic wall infarction or even perforation. However, we discovered the trouble early and adjusted the treatment in time. Artesunate acts faster and has a high intestinal distribution dose. So we switch from artemether to artesunate. And artesunate may kill late-staged sequestered parasites [11]. Clogged microvascular restored blood flow, and the colon function gradually recovered.
Electrolyte disturbance is also one cause of the ACPO. Electrolyte disturbances are common in patients with severe malaria, especially falciparum [12]. The patient in this study had hypokalemia, hyponatremia, and hypochlorous. The minimum potassium is 3.3 mmol/L, and the minimum sodium is 126 mmol/L. Changes in potassium and other electrolyte concentrations affect ion channel function and may alter pacemaker activity generated by interstitial cells of Cajal or smooth muscle activity [7].
Autonomic dysfunction is also one of the reasons. Colonic function is regulated by sympathetic and parasympathetic nerves systems. Most patients with major illness have increased systemic sympathetic drive, potentially contributing to autonomic imbalance at the level of the colon [7]. An imbalance in autonomic nervous activity with an increased sympathetic tone and decreased parasympathetic tone leads to functional obstruction in the distal colon [13].
In conclusion, ACPO should be considered for severe malaria patients with abdominal distention and pain. Early recognition of ACPO in malaria is extremely important, and the appropriate conservative treatment can achieve a good prognosis.
Acknowledgments
We would like to thank Dr. Rui Zhao and Dr. Yong Zhao for their supports and all staff of Chinese Level II Hospital in DRC involved in the care of this patient.
Financial Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that there are no competing interests.
Informed Consent
The patient authorized the main author, in written form, to publish this case report and the accompanying image (X-ray).
Author Contributions
Peng Fei Yao wrote the paper. Yang Sun managed the case and Peng Jiang Zhang and He Dong analyzed the blood sample. All authors read and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Organization WH. WORLD MALARIA Report 2019. Geneva: World Health Organization https://www.who.int/publications/i/item/world-malaria-report-2019.
- Dass R, Barman H, Duwarah SG, Deka NM, Jain P, Choudhury V. Unusual presentations of malaria in children: an experience from a tertiary care center in North East India. Indian J Pediatr. 2010;77(6):655-660.
doi pubmed - Molina-Infante J, Perez-Gallardo B, Gonzalez-Garcia G, Fernandez-Bermejo M, Mateos-Rodriguez JM, Robledo-Andres P. Octreotide LAR for severe obscure-overt gastrointestinal haemorrhage in high-risk patients on anticoagulation therapy. Gut. 2007;56(3):447.
doi pubmed - Chang CY, Pui WC, Kadir KA, Singh B. Spontaneous splenic rupture in Plasmodium knowlesi malaria. Malar J. 2018;17(1):448.
doi pubmed - Barman B, Bhattacharya PK, Lynrah KG, Ete T, Issar NK. Acute Pancreatitis in a Patient with Complicated Falciparum Malaria. J Clin Diagn Res. 2016;10(1):OD18-20.
doi pubmed - Bonghaseh TD, Ekaney DSM, Budzi M, Ekwen G, Kyota S. Sub-acute intestinal obstruction - a rare complication of Plasmodium falciparum malaria in an adult: a case report. J Med Case Rep. 2018;12(1):190.
doi pubmed - Wells CI, O'Grady G, Bissett IP. Acute colonic pseudo-obstruction: A systematic review of aetiology and mechanisms. World J Gastroenterol. 2017;23(30):5634-5644.
doi pubmed - Mankaney GN, Sarvepalli S, Arora Z, Kamal A, Lopez R, Vargo JJ, Burke CA. Colonic decompression reduces proximal acute colonic pseudo-obstruction and related symptoms. Dis Colon Rectum. 2020;63(1):60-67.
doi pubmed - Arakawa C, Gunnarsson C, Howard C, Bernabeu M, Phong K, Yang E, DeForest CA, et al. Biophysical and biomolecular interactions of malaria-infected erythrocytes in engineered human capillaries. Sci Adv. 2020;6(3):eaay7243.
doi pubmed - Cowman AF, Healer J, Marapana D, Marsh K. Malaria: Biology and disease. Cell. 2016;167(3):610-624.
doi pubmed - Plewes K, Leopold SJ, Kingston HWF, Dondorp AM. Malaria: what's new in the management of malaria? Infect Dis Clin North Am. 2019;33(1):39-60.
doi pubmed - Rani A, Akhtar S, Nawaz SK, Irfan S, Azam S, Arshad M. Electrolyte Disturbance and the Type of Malarial Infection. Iran J Public Health. 2015;44(11):1492-1497.
- Jayaram P, Mohan M, Lindow S, Konje J. Postpartum Acute Colonic Pseudo-Obstruction (Ogilvie's Syndrome): A systematic review of case reports and case series. Eur J Obstet Gynecol Reprod Biol. 2017;214:145-149.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Medical Cases is published by Elmer Press Inc.


